Key Points
- ▪
Duplex ultrasound assessment of the splanchnic/visceral arteries, with careful technique and adherence to a comprehensive duplex protocol, is feasible and accurate in the majority of patients.
Atherosclerotic aortic disease may result in stenosis of the origins to the celiac or to either of the mesenteric arteries. Most atherosclerotic disease of the splanchnic/mesenteric arteries occurs at the ostium and in the proximal segment. Disease, when present, commonly involves more than one vessel.
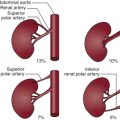
Anatomic variants of the splanchnic/mesenteric vessels occur. Anomalies such as a right hepatic artery arising from the superior mesenteric artery (SMA), a common hepatic artery arising from the SMA, or a common celiac-mesenteric trunk may be correctly recognized by ultrasound.
Many patients with disease involving the splanchnic vessels are hypertensive because their aortas are extensively and severely diseased (resulting in noncompliance systolic hypertension). Concurrent, if not adjacent, renal artery stenosis may further incite hypertension. The greater the hypertension, the higher the PSV needed to establish severity of the splanchnic (or other) vessel stenosis by use of that criterion alone.
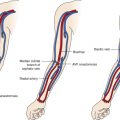
Use of PSV appears more useful than does end-diastolic velocity, which provides little additional information. The use of both fasting and postprandial scanning offers little incremental information if the SMA PSV is greater than or equal to 275 cm/sec. Patients with symptoms of chronic visceral ischemia and positive duplex studies should be considered for confirmatory angiographic testing. Duplex imaging also appears useful to follow surgical revascularization procedures ( Figs. 9-1 to 9-6 ).






Anatomy of the Splanchnic Arteries: the celiac, sma, and ima
The celiac artery (axis) is a 1.25-cm long stumpy artery arising from the anterior aspect of the aorta immediately below the diaphragm. It divides into the left gastric, splenic, and common hepatic arteries, which supply the spleen, liver, stomach, duodenum, and pancreas.
The SMA, a large artery, arises from the aorta approximately 1.25 cm distal to the celiac artery. This artery supplies the whole of the small intestine, cecum, the head of the pancreas, the ascending colon, and half of the transverse colon. The SMA lies behind the pancreas where the splenic vein crosses over its proximal segment and then courses downward and forward, crossing in front of the inferior vena cava, then diminishing in size to its terminus and anastomosis with one of its own branches, the ileal branch of the ileocolic artery. There are 12 to 15 branches that originate from the left side of the SMA; these divide and then anastomose with adjacent branches to form a series of arches supplying the small intestine.
The middle, right, and ileocolic arteries arise from the right side of the SMA. Of particular note is the middle colic artery, which forms an anastomosis with the left colic branch of the inferior mesenteric artery to create the marginal artery, an important collateral in the presence of celiac artery occlusive disease.
The inferior mesenteric artery is smaller than the SMA, arising from the anterior aspect of the aorta approximately 3 cm proximal to the aortic bifurcation at the level of the third lumbar vertebra. The inferior mesenteric artery supples the left half of the transverse colon, a greater part of the rectum, and the descending colon.
The inferior mesenteric artery lies anterior to the aorta and then runs downward on the left side, eventually crossing the left common iliac artery, after which it continues as the superior rectal hemorrhoidal artery. This important stem artery joins with other hemorrhoidal branches to provide a collateral network in cases of aortic obstruction.
Celiac Stenosis
Duplex scans are technically adequate in a very high percentage of celiac artery studies (96%); angiograms have a slightly higher technical adequacy rate (98%). A less than 50% stenosis of the celiac artery is not readily detected by ultrasound scanning, and fortunately, is not likely directly a (flow-limiting) lesion ( Table 9-1 ).
- ▪
It is important to note that portal venous flow is toward the probe, whereas that of the inferior vena cava and away from the liver.
- ▪
In the case of a high takeoff of the celiac axis, it is often possible to image/scan through the xiphisternum.
- ▪
To identify the celiac axis, look for the classic “seagull” sign, reminiscent of the body (axis) and wings (common hepatic arching to the right and then to the liver and the splenic artery arching left and onto the spleen). The axis itself can vary in its takeoff from the aorta (i.e., more lateral than anterior).
- ▪
If the superior mesenteric or celiac artery is severely diseased, there may be a compensatory increase in flow velocity in the other, and this could lead one to infer stenosis. Therefore, it is important to assess whether the identified flow velocity increase is focal or occurs throughout the vessel.
- ▪
Postprandial flow:
- ▪
In the celiac artery, there is little variation postprandially because the metabolic needs of the liver and/or spleen are relatively stable.
- ▪
The superior and inferior mesenteric artery flows change prominently postprandially; there can be a doubling of the peak systolic velocity (PSV) and a tripling of the diastolic flow in the celiac artery.
- ▪
- ▪
In the abdomen, it can be relatively easy to inadvertently compress the veins being interrogated.
- ▪
The hepatic artery normally arises from the celiac axis, but it can occasionally arise from the proximal superior mesenteric artery, resulting in turbulent flow at the confluence of the two vessels. This can possibly lead to an erroneous diagnosis of narrowing.
- ▪
Median arcuate ligament compression: where a band of this ligament (that connects the two sides of the diaphragmatic crura) is caught around the celiac axis and can cause its compression, narrowing and increasing the flow velocity at that point. This occurs in 0% to 24% of people. Because median arcuate ligament compression is most noticeable at the end of expiration, it is useful to instruct the patient to inspire deeply; this will temporarily release the band, and in doing so decrease the velocity, thus indicating that the process is not atherosclerotic.
| PARAMETER | REFERENCE | ANGIOGRAPHIC STANDARD | SENSITIVITY | SPECIFICITY | PPV | NPV |
|---|---|---|---|---|---|---|
| PSV ≥ 275 cm/sec | Mitchell | ≥70% Stenosis | 92% | 80% | 99% | |
| PSV ≥ 275 cm/sec or no flow | Moneta | 89% | 92% | 80% | ||
| PSV ≥ 275 cm/sec | Gentile | 70%–99% | ||||
| Fasting | 89% | 97% | 80% | 99% | ||
| Postprandial | 67% | 94% | 60% | 91% | ||
| Fasting and postprandial | 67% | 100% | 100 | 96% | ||
| PSV ≥ 275 cm/sec | Zwolak | ≥50%–100% | 60% | 100% | ||
| EDV ≥ 275 cm/sec | Zwolak | 90% | 91% | 90% | 91% |
Superior Mesenteric Artery Stenosis
Duplex scans are technically adequate in a very high percentage of SMA studies (98%). Angiograms have an 100% technical adequacy rate.
A specific PSV cutoff for the determination of the presence of a significant stenosis of the SMA has been elusive, because hypertension is common in this patient population ( Table 9-2 ).