Fig. 15.2
Ultrasound-guided splenic biopsy. A 58-year-old woman with a history of mucinous cystadenoma of the ovary presented with an enlarging focal lesion within the spleen. Ultrasound image demonstrates the echogenic tip of the 22-gauge Chiba needle within the hypoechoic lesion in the inferior pole of the spleen. The biopsy tract was chosen to traverse the least amount of splenic tissue. The biopsy specimen yielded benign splenic tissue and the lesion is being followed clinically and by imaging
Coagulation studies (platelet count, prothrombin time, international normalized ratio (INR), and partial thromboplastin time) should be examined and any coagulopathies should be corrected prior to biopsy. In general, an INR ≤1.5 and platelet count ≥50,000/L are acceptable parameters for solid-organ biopsy. Written informed consent must be obtained before each procedure. Splenic biopsy is well tolerated and can be performed either with local anesthesia alone or with monitored, conscious sedation using intravenous midazolam and fentanyl citrate. Preprocedural, prophylactic antibiotics are not routinely recommended.
Technique
Imaging
Either ultrasound guidance or non-contrast enhanced, CT guidance can be used for splenic biopsy. The imaging modality that best demonstrates the lesion within the spleen should be selected. The advantage of ultrasound guidance is that it provides real-time imaging in multiple planes and visualization of the needle during biopsy (Fig. 15.2). An advantage of CT guidance is the ability to accurately visualize adjacent organs, such as the colon, lung, and kidney, and their anatomic relationships to the spleen (Fig. 15.3). In some cases, the lesion cannot be seen with non-contrast-enhanced CT and the administration of intravenous contrast may be necessary for lesion localization. Another advantage of CT guidance is that a non-contrast-enhanced CT scan can be obtained immediately after the procedure to evaluate for potential complications, such as pneumothorax and hemorrhage.
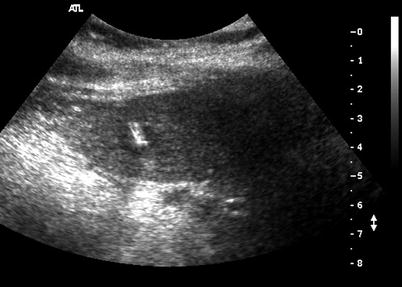

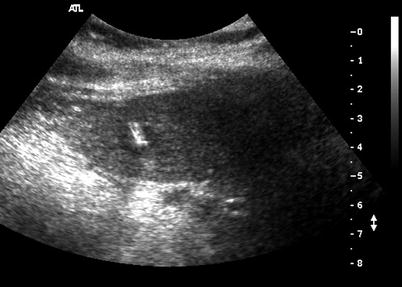
Fig. 15.3
CT-guided splenic biopsy. A 26-year-old woman with large cell lymphoma presents following chemotherapy with a residual lesion within the spleen. Biopsy was requested to evaluate for residual disease versus transformation to a higher grade of lymphoma. Axial non-contrast CT scan demonstrates use of the coaxial technique. A 19-gauge Chiba needle was inserted into the periphery of the splenic lesion using an anterolateral, intercostal approach. A 22-gauge Chiba needle was inserted coaxially and the tip lies within the center of the lesion. Both fine-needle aspiration and core biopsy were performed of this lesion. A pathologic diagnosis of atypical lymphohistiocytic infiltrate in a background of mild sclerosis and increased histiocytes, suspicious for lymphomatous involvement, was made on the examination of the 20-gauge core biopsy

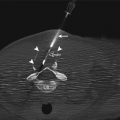
Fig. 15.1
CT-guided splenic biopsy targeting FDG-avid lesion. A 60-year-old man with a history of diffuse large B-cell lymphoma presents with a new FDG-avid lesion in the upper pole of the spleen (a). The specific area of FDG avidity was targeted during the CT-guided biopsy (b). A lateral approach was taken to traverse the least amount of splenic tissue during biopsy. A coaxial technique was used and the CT image demonstrates the core-biopsy needle within the hypodense lesion. Both fine-needle aspiration and core biopsy were performed and a pathologic diagnosis of B-cell lymphoma was made
Devices
Fine-needle aspiration of the spleen is usually performed using 20- to 22-gauge needles [3, 4, 7, 16]. Core-needle biopsies using 18- to 20-gauge needles have also been reported [17]. Biopsy with larger gauge needles (e.g., 14-gauge needles) has been reported, but the use of these larger needles is associated with an increased risk of hemorrhage [18].
Approaches and Relevant Anatomy
In contrast to liver biopsy, for which a biopsy tract through normal liver tissue is recommended to provide a tamponade effect, splenic biopsy should be performed on the most peripherally located lesion, thereby traversing the least amount of splenic tissue and minimizing the potential for hemorrhagic complications. The patient should be positioned so that the most direct path for biopsy of the lesion is accessible. Typically, when biopsy is performed under ultrasound guidance, the patient is in a supine or right lateral decubitus position [9, 17]. Several authors recommend that the patient be instructed to suspend respiration during needle insertion and biopsy to minimize needle movement and the resulting trauma to the splenic tissue [2, 8, 9, 19]. A subcostal approach is favored, although an intercostal approach may be necessary depending on the lesion’s location. For splenic lesions in the upper pole, the triangulation method or angling of the CT gantry may be necessary to avoid traversal of the pleural reflection [20]. Most ultrasound-guided biopsies are performed using a free-hand technique, as most lesions are located in the periphery of the spleen [4]. For deeper lesions, a coaxial technique may be helpful and allows for both fine-needle aspiration and core biopsy to be performed with only one puncture of the spleen.
Potential Complications and Management of Complications
Splenic biopsies can be performed on an outpatient basis. Following the procedure, patients should be observed for potential complications. Postprocedural observation times vary between 2 and 4 h [9, 11, 19] and include monitoring of the patient’s blood pressure, pulse, and oxygen saturation. Postprocedural chest radiography should be performed in patients in whom a pleural surface was traversed to evaluate for pneumothorax. Patients who remain stable following the observation period, with minimal or no discomfort, can be discharged home. Patients should be instructed to avoid heavy lifting and strenuous activity for at least 3 days, as delayed hemorrhagic complications have been reported [4, 11, 18, 19].
In 1976, Soderstrom reported no complications in a series of more than 1,000 “blind” splenic biopsies [2]. More recently, complication rates ranging from zero to 16.7 % have been reported for splenic biopsy (Table 15.1). Unfortunately, uniform criteria for reporting complications have not been applied across the studies, making direct comparisons difficult. Most postbiopsy complications are minor and self-limited, requiring no additional treatment. For example, postprocedural pain occurring in the left upper quadrant or radiating to the left shoulder has been described in up to 50 % of patients after percutaneous splenic biopsy [18]. Hemorrhage following splenic biopsy has been reported in zero to 8.3 % of patients [3, 5, 11, 16, 17, 21]. Most cases of hemorrhage are self-limited, perisplenic hematomas that do not require further intervention (Fig. 15.4); however, although rare, uncontrolled hemorrhage has been reported and can result in the need for blood transfusions, the need for emergent splenectomy, or death[1, 11, 16] (Fig. 15.5). Other complications such as pneumothorax, pleural effusion, and colonic injury have also been described [3, 5].
Table 15.1
Comparison of results of percutaneous splenic biopsy
Study | No. of biopsies | Diagnostic yield (%) | Overall accuracy (%) | Complication rate (%) |
|---|---|---|---|---|
Siniluoto et al. [23] | 42 | 97.6 | 88.1 | 0 |
Caraway et al. [1] | 50 | 88 | NR | 2 |
Venkataramu et al. [21] | 35 | 62.8 | NR | 2.9 |
Keogan et al. [7] | 20 | 88.9 | NR | 0 |
Civardi et al. [3]
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|