5 Standard Protocol for Breast Ultrasound Examinations A thorough history should be taken prior to clinical examination, sonography, or any other imaging studies. Many practices ask patients to complete a questionnaire as a means of obtaining pertinent personal, clinical, and family history. The first question to be answered is the reason for the visit: mass, focal pain, thickening, nipple discharge. The history should include allergies, medical and surgical history, history of breast or other carcinomas, medications (hormone replacement or oral contraceptive use, risk reducers or breast cancer treatment such as tamoxifen or chemo-therapy), and reproductive history. The majority of women who undergo mammography regularly are asymptomatic and complying with screening recommendations, but ultrasound examinations are most often done for problem-solving. Ultrasound screening remains a research focus in the United States, although there is recognition from individual studies that survey ultrasound can increase the yield of carcinomas above and beyond those identifiable clinically or by mammography. It is of great importance at the outset to determine a patient’s risk of breast cancer. Factors associated with the highest risk include personal history of breast cancer, prior radiation therapy to the mediastinum for lymphoma or to the thorax for tuberculosis, genetic aberrations (BRCA1 and 2 genes), family history of breast carcinoma in a premenopausal first-degree relative (mother, sister, or daughter), and histological findings of lobular carcinoma in situ, atypical lobular hyperplasia, or atypical ductal hyperplasia on previous biopsies. Other factors that increase breast cancer risk, although of lower relative risk than the preceding, include personal history of ovarian or endometrial carcinoma (and prostatic carcinoma in male relatives), nulliparity or first pregnancy after the age of 30 years, and family history of breast cancer in a first-degree relative, not premenopausal. Prior surgical history can be helpful in correlating sonographic with mammographic or clinical findings. Expected sonographic changes following lumpectomy for carcinoma followed by radiation therapy are discussed in Chapter 11. Reduction mammoplasty is a common procedure that may result in areas of scarring or fat necrosis, and sonographic findings associated with intra- or extracapsular ruptures of breast implants placed for reconstruction or augmentation are known. The patient should also be questioned about previous surgery on other organs, given the potential for metastases to the breast and lymph nodes from tumors at other locations. Previous gynecologic disorders are also important, as they may direct attention to hormonal changes that affect the breast (Table 5.1).
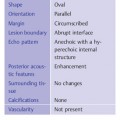
Patient History
|
|
|
|
|
|
|
|
Findings | Localization |
Breast size | Symmetry |
Skin redness, edema | Right, left, bilateral |
Skin dimpling or protrusion | Diffuse, circumscribed |
Skin thickening | Quadrant, clock-face position |
Nipple: Paget, eczema, retraction | Central, peripheral Distance from the nipple (in cm) |
Findings | Localization |
No palpable abnormalities | Symmetry |
Mild nodularity | Right, left, bilateral |
Moderate nodularity | Diffuse, circumscribed |
Coarse nodularity | Quadrant, clock-face position |
Indurations | Central, peripheral |
Masses: soft, firm, rubbery, smooth, lobulated, irregular, mobile, fixed | Distance from the nipple (cm) |
Clinical Examination
The findings from physical inspection and palpation should also be documented (Tables 5.2, 5.3). Spontaneous pain and diffuse or focal tenderness should be noted. It should be determined whether the pain is constant, sporadic, or cyclic in its occurrence, and its severity should be noted. It is important to know when visible or palpable changes first appeared and how they have progressed over time. Surgical scars should be diagrammed, and the date of the procedure and its histologic findings should be noted. If the breasts have not been examined prior to sonography, physical examination to correlate with the ultrasound findings is opportunely done by the sonologist at the time of sonography.
Breast parenchyma | ACR density I (parenchyma < 25%, involution), II (25–50%), III (50–75%), IV (parenchyma >75%, dense breast tissue) |
Focal densities | Round, oval, smooth, sharp, ill-defined, spiculated |
Macrocalcifications and micro-calcifications | Disseminated, focal clusters, clumped, rounded, pleomorphic |
Benign–malignant differentiation | BI-RADS categories I–V |
Architecture | Homogeneous/heterogeneous |
Background echotexture | Fat Fibroglandular Mixed pattern |
Proportion of fat | According to ACR mammography classification (I–IV) |
Ducts | Diameter (mm) Smooth, irregular Anechoic, low-level internal echoes |
Prior Mammograms
If sonography is directed to evaluation of a mammographic finding, mammograms and reports should be available for review. Whether or not the prior mammograms were normal, the breast density should be noted according to the mammography BI-RADS categorization (fat, scattered fibroglandular density, heterogeneously dense, extremely dense; see Chapter 3), the sensitivity of mammography decreasing as the breast density increases. Federal legislation in the United States requires that breast density be reported along with the mammographic findings. The sonograms should be placed in context of mammographic findings, the relative importance of the ultrasound examination increasing concomitantly with progressive breast density on mammograms.
In addition to diffuse changes, symmetry of the breasts can be an important diagnostic criterion. Nonspecific asymmetric densities may correlate with sonographically visible abnormalities or patterns of fibroglandular parenchyma. All circumscribed focal lesions as well as diffuse and clustered microcalcifications should be characterized using BI-RADS descriptors (Table 5.4).
Other Studies
The results of previous ultrasound and other examinations (e. g., Doppler scans, MRI, percutaneous aspiration or needle biopsy, radionuclide scans, CT scans, and PET and other special studies) should be accounted for and correlated with findings of the current ultrasound examination.
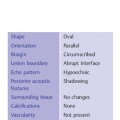
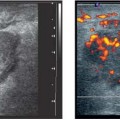
Ultrasound Findings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Menarche, menopause
Menarche, menopause Menstrual history
Menstrual history Obstetric history
Obstetric history Medications, including hormones
Medications, including hormones Family risk factors
Family risk factors Prior operations and histology
Prior operations and histology Prior gynecologic disorders
Prior gynecologic disorders Reason for seeking medical attention
Reason for seeking medical attention