Class
Original RTOG definition
Median survival (months)
Two-year survival (%)
RTOG
EORTC/NCIC
RTOG
EORTC/NCIC
I
Age <50, AA, normal mental status
58.6
n/a
76
n/a
II
Age ≥50, KPS 70–100, AA, ≥3 months from first symptoms to treatment
37.4
n/a
68
n/a
III
Age <50, AA, abnormal mental status or
17.9
21.4
35
43.4
Age <50, GBM, KPS 90–100
IV
Age <50, GBM, KPS <90 or
11.1
16.3
15
27.9
Age ≥50, KPS 70–100, AA, ≥3 months from first symptoms to treatment or
Age >50, GBM, surgical resection, good neurologic function
V
Age ≥50, KPS 70–100, GBM, either surgical resection and poor neurologic function or biopsy only followed by ≥54.4 Gy EBRT or
8.9
10.3
6
16.5
Age ≥50, KPS <70, normal mental status
VI
Age ≤50, KPS <70, abnormal mental status
4.6
n/a
4
n/a
Age ≥50, KPS 70–100, GBM, biopsy only, <54.4 Gy EBRT
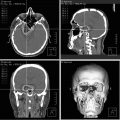
Despite intermittent waves of enthusiasm regarding various treatment modalities, the survival of patients with HGG has only improved modestly from 1950 to 2000. In this chapter, we describe and contextualize the use of stereotactic radiosurgery (SRS) and fractionated stereotactic radiotherapy (F-SRT) in the management of primary and recurrent malignant gliomas.
Historical Perspective
The poor prognosis of HGG is known for many years. In 1926, Bailey and Cushing, in reference to what they at the time called “spongioblastoma multiforme,” made the following observation: “Operative procedures, howsoever radical [block extirpations repeated on signs of recurrence; saturation with X-rays or radium emanations after wide decompression with or without surgical interference with the tumor], have apparently done little more than to prolong life, save vision, and alleviate headache for an average of a few months. Whether deep Roentgenization ever does more than hold the growth temporarily in check is problematical” [12].
By the time Elvidge, Penfield, and Cone published their “McGill series” in 1937, the name “glioblastoma multiforme” had become widely accepted and neurosurgery was still faced with the same “difficult human problem” posed by these patients [13].
Thirteen years after the publication of Elvidge and colleagues, the following case history was published as part of a paper reviewing 70 glioblastoma multiforme patients treated at the Montefiore Hospital [14].
Case 17.1 represented the longest surviving patient in the literature of the day [14]. Prognostic factors for the Montefiore series were reviewed: “An analysis of factors in survival revealed that operation had no significant effect on longevity and irradiation a slight effect, if any. The longest survivals occurred in patients with onset at 24–42 years of age. However, age at onset was not a constant prognostic factor. The sex of the patient, the location of the neoplasm, or the histologic appearance gave no indication as to longevity. A significant lengthening of survival was found in those patients whose initial symptom was a motor seizure.” If patients dying within one week of surgery were excluded the median overall survival was 13.1 months with postoperative irradiation and 12 months without. It must, however, be noted that for all cases of prolonged survival reported in this paper, the patient had received irradiation.
As demonstrated by the previous series, irradiation had been in common use long before randomized trials demonstrating its efficacy. In 1947 Bush and Christensen wrote: “While it is very difficult to judge of the effect of radiation in these cases, it is our impression that this therapy is of definite value. A half-hearted attempt of giving every other patient Roentgen therapy was never carried through as we felt ourselves unable to deprive the particular patient of what we felt was the best chance” [15].
It was only in the early 1980s that both the Brain Tumor Cooperative Group (BTCG) and the Scandinavian Glioblastoma Study Group (SGSG) published results of randomized trials of adjuvant irradiation [16, 17]. These trials confirmed a large and significant increase in median survival following the administration of postoperative irradiation, as compared to surgery alone. In the Scandinavian trial, 45 Gy of whole-brain irradiation increased the median survival from 5.2 months to 10.8 months. In BTSG study 6901, median survival increased from 3.2 to 8.1 months following 50–60 Gy of whole-brain radiotherapy.
Looking at the role of chemotherapy, a 1993 meta-analysis by Fine et al. collated data from 16 randomized trials involving more than 3,000 patients [18]. Optimistic physicians saw a large (52 %) difference in 2-year survival; pessimistic physicians saw a relatively small difference in median survival. A subsequent meta-analysis from the Glioma Meta-analysis Trialists group confirmed a 1.5-month increase in median survival and failed to demonstrate any benefit of multi-drug regimens over single agent nitrosourea compounds [19]. Adjuvant BCNU chemotherapy was considered standard of care by most, although it was used variably in clinical practice. Subsequently, in a joint European Organization for Research and Treatment of Cancer (EORTC) and National Cancer Institute of Canada (NCIC) randomized trial [20], concomitant and adjuvant temozolomide was shown to significantly increase the survival of patients diagnosed with glioblastoma multiforme. The median survival went from 12.1 to 14.6 months and the 2-year survival more than doubled (26.5 % vs. 10.4 %). It is of interest to note that the control arm (radiotherapy alone) had the same median survival as reported in the 1949 series from the Montefiore Hospital, highlighting how little progress had been made in the previous 50 years.
Based on this EORTC/NCIC trial, the current standard of care for GBM patients with a performance status of 0–1 (on subgroup analysis, there was no benefit for patients with an ECOG performance status of 2) is external beam radiotherapy to 60 Gy and temozolomide. Although patients with AA histology were not included in the trial, this regimen has become for many a de facto standard as we await data from current prospective studies.
Rationale for Stereotactic Radiosurgery
Infiltrating high-grade glial neoplasms would appear to be poor candidates for the stereotactic application of single fraction irradiation. These tumors are hypoxic, acute-responding [21] and admixed with normal tissue [22, 23]. Despite these biological roadblocks, stereotactic radiation has been pursued in the management of HGG. The use of SRS (defined here as a radiotherapy technique characterized by accurate delivery of high doses of radiation in a single session to small intracranial targets in such a way that the dose fall-off outside the target volume is very sharp) has been based on the pattern of failure of this disease, the dose–response data from external beam radiation, and early data from interstitial brachytherapy trials [24, 25].
As mentioned previously, up to 90 % of patients recur within 2 cm of the contrast-enhancing lesions—this despite the fact that tumor cells can be found pathologically at larger distances, often following the peri-tumoral edema. Furthermore, multicentric or metastatic disease is rare [11]. Moreover, in an analysis of the Brain Tumor Study Group data, a dose–response relationship has been shown for doses of 50 to 60 Gy [26]. In this data set, the median survival increases from 28 weeks at 50 Gy to 42 weeks at the 60 Gy level. Significant improvement in median survival was also observed in the randomized British trial comparing 45–60 Gy [27]. All of these characteristics made SRS an attractive option to be used as a focal boost in selected patients with HGG.
In the early 1990s, phase I/II data suggested that interstitial brachytherapy improved local control and survival in selected primary and recurrent HGG patients. At University of California at San Francisco (UCSF), the median survival of the first 18 patients treated with interstitial brachytherapy for recurrent GBM was 52 weeks with two patients surviving more than 5 years [28]. In a subsequent NCOG study [25], 107 patients with HGG were enrolled in a program of brachytherapy added to external beam radiation therapy (EBRT) and adjuvant PCV chemotherapy. In the 63 evaluable patients who were actually implanted, the median survivals were 157 weeks and 88 weeks, respectively, for patients with grade III astrocytoma and GBM. Brachytherapy was associated with a high risk of radionecrosis and it was felt that SRS might offer the focal dose escalation benefits of implants with lessened toxicity. Unfortunately concerns about selection bias [29], as a possible explanation for these improved median survivals following brachytherapy, appear to be have been confirmed by two subsequent negative phase III trials of brachytherapy by the BTSG [30] and the Princess Margaret Hospital [31] groups. In these randomized studies, the added use of a focal brachytherapy boost did not lead to either a clinically or statistically significant improvement in survival for patients harboring a HGG. In the Toronto trial, the median survival was 13.2 months on the standard arm and 13.8 on the brachytherapy arm, while in the BTSG study it was 58.8 weeks on the standard arm and 64.1 on the brachytherapy arm.
In 1985, Columbo et al. reported on the first patients treated in Vinceza, Italy with a new technique for linear accelerator-based radiosurgery using non-coplanar arcs [32]. Only 6/22 patients had adequate follow-up. Of these, one patient was treated for a 3.5 cm grade III astrocytoma. Two doses of 20 Gy were delivered during separate procedures. This patient worsened within 2 months and underwent reoperation. Following this early experience, several institutional reports have been published on the use of SRS boost in the management of patients with HGG either at presentation or time of recurrence. The non-invasive nature of SRS coupled with the promising early results of interstitial brachytherapy led to the inflated enthusiasm for the technique in patients with HGG and a growing number of publications became available over the years (Fig. 17.1). Many of these reports were published before the results of the randomized trials of brachytherapy and SRS were available.


Fig. 17.1
Publications on the radiosurgical treatment of HGG
Radiosurgery has predominantly been used in one of two scenarios: in primary lesions as a supplement to wider volume EBRT and in recurrent lesions as a single modality. Initially F-SRT was explored to increase the therapeutic ratio in previously irradiated patients; it has since also been explored as a boost in the treatment of newly diagnosed HGG patients. With the advent of non-invasive immobilization devices and sophisticated image-guidance, the use of F-SRT has become more common—it has also become more difficult to distinguish from what is now “conventional” radiotherapy. We have thus chosen to exclude from our review protracted treatment schedules—even if labeled “stereotactic.”
Treatment Planning
Although each case must be approached on an individual basis, the following general guidelines represent a reasonable approach to the delivery of stereotactic therapy for HGG.
Stereotactic Radiosurgery
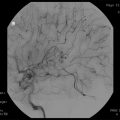
In the primary treatment of HGG, SRS is used as a boost to EBRT. The goal of radiosurgery is to inflict precise damage to tissue within the target volume, in this case proliferating glial cells. Thus, only tumors with a limited diameter (at presentation or postoperatively) should be considered for SRS. The RTOG considered a diameter of 40 mm the maximum diameter allowed for patient entry into the SRS trials. As a larger area of potential microscopic disease is targeted by the EBRT, the SRS target volume (PTV) is limited to the tumor without margins. Individual programs have developed expertise in PET or advanced MRI imaging. As long as the technical and clinical limitations of these modalities are understood, their use is reasonable—however, T1 contrast MRI remains the standard modality for GTV definition. Completely resected tumors are generally not considered for SRS boosts but, in selected cases, reactive enhancement or a rim of normal-appearing parenchyma can form the radiosurgery target [33].
The maximum clinically tolerated doses for the treatment of HGG have been derived from the RTOG 90–05 phase I study and are tumor size-dependent [34]. Single doses of 24, 18, and 15 Gy were found to be the maximum tolerated doses for tumors diameters of ≤20 mm, 21–30, and 31–40, respectively. These doses are usually prescribed to an isodose surface between 50 and 90 %. Caution should be exercised when treating brain stem lesions and lesions within 10 mm of the optic chiasm, as these lesions were not included in the RTOG study and the maximum tolerated radiosurgery dose has not been clearly established for these structures.
For recurrent disease, similar principles apply. It is also a general rule that only lesions smaller than 4 cm are considered for SRS. In these cases the GTV is the enhancing lesion on the T1 MRI. On a case-by-case basis, a CTV of a few millimeters (~2–5 mm) can be added. For rigid immobilization systems and systems with intra-fraction image-guidance, no additional margin is added for the PTV.
Table 17.2 contrasts commonly used treatment parameters for stereotactic irradiation in HGG.
Table 17.2
Comparison of common parameters for stereotactic irradiation modalities
Parameter | SRS | F-SRT |
|---|---|---|
Tumor Size | ≤40 mm | ≤60 mm |
Total Dose | 15–24 Gy | Variable (∼30 Gy in 5) |
Fractions | Single | Multiple |
Prescription isodose | 50–80 % | 70–90 % |
Margins | 0–2 mm | 2–5 mm |
Fractionated Stereotactic Radiation Therapy
For both primary and recurrent lesions, larger volumes can be considered for F-SRT than SRS. Depending on the planned dose of F-SRT and the use (concurrent or prior) of EBRT, volumes of up to approximately 100 cm3 can be considered for treatment. Margins will depend on the volume to be treated, proximity of critical structures, prior treatment, and the image-guidance used. A reasonable approach for recurrent disease would have the GTV equal to the enhancing lesion on a gadolinium-enhanced T1 MRI with a combined CTV/PTV margin of 3 mm (mainly accounting for the reproducibility of standard IGRT or a common three ply thermoplastic mask-based immobilization system [35, 36]). Table 17.3 [37–50] contains various published fractionation schemes. Depending on the technique, dose would be prescribed to the 50–90 % isodose surface after assessing the plan for volume irradiated, subjective isodose distribution, conformity, homogeneity, and dose to critical structures.
Table 17.3
Results of F-SRT for primary and recurrent high-grade gliomas
Author | Glass [37]* | Shepherd [38] | Hudes [39] | Lederman [40] | Baumert [43] | Cho [44] | Vordermark [45] | Cardinale [46] | Schwer [47] | Fokas [48] | Gutin [49] | Fields [50] | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Institution | Temple | Royal Marsden | Thomas Jefferson | Staten Island | Kentucky | Zurich | Minnesota | Würzburg | RTOG | Colorado | Marburg | MSKCC | Colorado |
Date of publication | 1997 | 1997 | 1999 | 2000 | 2000 | 2003 | 2004 | 2005 | 2006 | 2008 | 2009 | 2009 | 2012 |
Number of patients | 20 recurrent | 33 recurrent | 20 recurrent | 88 recurrent | 8 primary 1 recurrent | 17 primary | 10 primary | 19 recurrent | 76 primary | 15 recurrent | 53 recurrent | 25 recurrent | 10 recurrent |
Histology | GBM 13 | AA 29 | GBM 19 | GBM | GBM 6 | GBM 15 | GBM 10 | GBM 14 | GBM | GBM 11 | GBM | GBM 20 | GBM 7 |
AA 7 | AO 3 | AA 1 | AA 2 | AA 2 | AA 5 | AA 4 | GR III 5 | AA 3 | |||||
LGG 1 | |||||||||||||
Median age (range) | 44.5 (6–73) | 37 (19–55)a | 52 (26–77) | 56 (21–82) | ≥18 | 51 (25–64.8_ | 57 (17–80) | 50 (11–74) | 57.5 (25–83) | 47 (23–65) | 53 (22–71) | 56 (30–80) | 40 (22–72) |
KPS | – | 80 (60–100)a | 80 (60–100) | 70 (50–90) | ≥60 | (5/12 WHO 0/1, 7 WHO 2) | 70 (60–90) | 90 (60–90) | Zubrod 0–1 | 80 (60–90) | 70 | ≥ 70 | 60 (60–80) |
Time from Diagnosis (for recurrent lesions) | – | 29a | 3.1 (0.8–45.5) | 6.5 | n/a | n/a | n/a | 19 (3–116) | n/a | 12 (3–57) from EBRT | – | 14.5 (6–135) | 14.5 (7–123) |
From EBRT | |||||||||||||
Median fu (months) | – | – | 8.5 | >12 | 15a | 25 (9–50) | – | – | 22 | 7 | 8 | 6.6 | 4 |
Median tumor volume (range) | 14.3 (1.76–122) | 24 (3–93)a | 12.66 | 32.7 (1.5–150.3) | 7.4 (1.5–27.2)a | – | 34 (4–70) | 15 (4–70) | – | 41 (8.4–151) | – | 34 (2–62) | 54 (6.7–123) |
Median peripheral dose (range) | 42/7 (–) | 35/7 (20/4–50/10) | 30/10 (21/7–35/10) | 24/4 | 14–28/2–4 | 19 | 27.5/11 (20–35/8–14) | 30/6 | 50 Gy EBRT + 20–28/4 | 18–36/3 | 30/5 | 30/5 | 36/3 |
(18/4–36/4) | 7 | (20–30/2–6) | (20–60/5–30) | ||||||||||
Median survival (months) | 12.7 | AA 11 | 10.5 | 7 | 11 | 20 | 15.9 | 9.3 | 12.5 | 10 | 9 | GBM 12.5 | 6 |
1-year survival (%) | – | – | 20 | 17 | 56 | 77 | 67 | – | – | – | – | GBM 54 | – |
Median prescription isodose (range) | ≥70 | 90 (80–90) | 89 (80–95) | 90 (80–90) | 50 | prescribed at isocenter | 88 (75–90) | 80 (70–90) | 80–90 | 90 (80–93) | prescribed | 94 | 92 (90–97.6) |
at isocenter | |||||||||||||
EBRT | All prior EBRT? | All prior EBRT | All prior EBRT | 99 % | 59.4/33 | 60 | 60 (50.4–60) | All prior EBRT | 50 | All prior EBRT | All prior EBRT | All prior EBRT | All prior EBRT |
Toxicity | 15 % necrosis | 45 % at 24 monthsa | no GR III | – | 4/15 GR IVa | 6 % necrosis | 10 % necrosis | – | 20 % GR IV (mainly hematological) | No symptomatic necrosis | No > GR II | 6 GR IV no nocrosis | 3 DLT |
Linear Accelerator vs. Gamma Knife
HGG are large infiltrating tumors for which debates about fractions of a millimeter are somewhat irrelevant. Because of the necrotic and presumed radio-resistant core of high-grade tumors, there might be a theoretical advantage to more inhomogeneous plans. As Gamma Knife (GK) treatments commonly use multiple isocenters and are prescribed to lower isodose surfaces, they might offer a theoretical advantage over more homogeneous single isocenter or dose painting plans (if this were ever clinically verified, linear accelerator (LINAC) centers could then choose to prescribe treatments to lower isodose surfaces). This hypothesis was tested by Larson and colleagues at UCSF in a Phase II trial [51]. In this trial prescriptions were made to isodoses as low as 25 %. The results, however, appear no different than would be expected with conventional treatment (15 weeks median survival for patients with recurrent grade IV tumors).
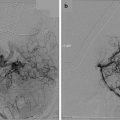
A review of the single-institution series will reveal a mix of GK and LINAC-based treatments. The two largest series are still from Pittsburgh [52] and Boston [53]—historically prototypical gamma-knife and LINAC-based programs. Not unexpectedly, there is no difference in result between these two series—both reporting a median survival of 20 months for the treatment of primary tumors. In the initial RTOG Phase I trial of radiosurgery for recurrent tumors, there appeared to be a large difference in results favoring GK in the treatment of a mixed bag of primary brain tumors [54]. This was not born out in the much larger and more homogeneous experience of the RTOG 93–05 randomized trial [55]. In this trial, in a subgroup analysis, patients treated with LINAC systems had a 14-month survival, not statistically different from the 12.1-month survival of GK patients (Fig. 17.2). If patients are to be treated with radiosurgery, delivery system should not be an issue.


Fig. 17.2
Survival by SRS treatment delivery system in RTOG 93–05 (From Souhami L, Seiferheld W, Brachman D, et al. Randomized comparison of stereotactic radiosurgery followed by conventional radiotherapy with carmustine to conventional radiotherapy with carmustine for patients with glioblastoma multiforme: report of Radiation Therapy Oncology Group 93–05 protocol. Int J Radiat Oncol Biol Phys 2004; 60:853–860. Used with permission from Elsevier.)
SRS in the Primary Management of High-Grade Gliomas
The 1990s saw the publication of several small, retrospective and prospective, series of patients treated with SRS boost in the primary treatment of malignant glioma (Table 17.4) [33, 52, 53, 56–66]. Ages ranged from 3 to 84 years and Karnofsky performance status from 40 to 100. Overall the median survival of patients treated with SRS was quite encouraging, although some series reported no benefit in survival when comparing results to historical controls. However, in a disease where more than 95 % of patients will ultimately die of their disease, the median survival is dictated more by patient-related than therapy-related factors [4]. By the very nature of SRS, patients are selected for small tumors, more complete resection (size determination being based on postoperative imaging), and a good response to initial therapy (when SRS is administered after EBRT ± chemotherapy, patients with progressive disease or decreasing performance status are likely to be excluded). Other potential sources of bias include high patient motivation, more favorable tumor biology, and aggressive treatment of recurrences. Taking these selection factors into account, only one tenth to one quarter of GBM patients will be eligible for radiosurgical boost [67].
Table 17.4
SRS in the primary management of high-grade gliomas
Authors | Selch [56] | Masciopinto [57] | Gannett [58] | Buatti [59] | Kondziolka [52] | Shenouda [60] | Shrieve [53] | Nwokedi [61] | Hsieh [62] | Smith [33] | Biswas [63] | Villavicenci [64] | Pouratian [65] | Einstein [66] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Institution | UCLA | Wisconsin | Arizona | Florida | UPMC | McGill | Harvard | Maryland | Northwestern | Phoenix | Rochester | Multi- | Virginia | Case Western |
center | ||||||||||||||
Year | 1993 | 1995 | 1995 | 1995 | 1997 | 1997 | 1999 | 2002 | 2005 | 2008 | 2009 | 2009 | 2009 | 2012 |
Number of patients | 18 | 31 | 30 | 11 | 65 | 14 | 78 | 31 | 25 | 27 | 15 | 20 | 22 | 35 |
Histology | 12 GBM | GBM | 17 GBM | 6 GBM | 45 GBM | GBM | GBM | GBM | GBM | GBM | GBM | GBM | GBM | GBM |
6 AA | 10 AA | 5 AA | 20 AA | |||||||||||
KPS (%) | 100 % >70 | 57 % >70 | 97 % >70 | all >90 | Mean KPS 90 (50–100)a | 79 % >70 | median 90 (50–100) | 61 % >70 | 70 | >60 | >70 | Median 82 (60–100) | Median 40 (40–100) | Median 90 (60–100) |
Median volume (cc) | 20 (8–46) | 16 (2–60) | 24 (2–115) | 14 (6–23) | 6.5 (1–31)a | < 34 | 10 | 25 | 23.6 | 34.6 | 13.2 | 5.8 (0.7–47) | 13.4 (4.4–56) | – |
(1.5–85) | ||||||||||||||
Median MPD (range) | 30 (15–35) | 12 (10–20) | 10 (0.5–18) | 13 (10–15) | 16 (12–25)a | 20 | 12 (6–24) | 17 | 12 | 12 | 10.4 | 20 (12–25) | 5.6 (4–10) | 15–24 |
Sequence | Post-EBRT | Pre-EBRT 12 | Within 8 weeks (median 4) | 12–109 days | GBM median 6.2 months | Pre-EBRT | Post-EBRT, median 14.2 weeks from diagnosis (range 1–42) | Within 4 weeks post-EBRT | Post-EBRT | Pre-EBRT | Post-EBRT | Alone or post-EBRT | 91 % Post-EBRT | Pre-EBRT |
Post-EBRT 17 | post EBRT | post diagnosis AA median 3.9 months | ||||||||||||
No EBRT 2 | (typically | post diagnosis | ||||||||||||
2–3 weeks) | ||||||||||||||
Median survival (months) | 9 | 9.5 | GBM 13 | 17 | GBM 20 | 10 | 19.9 | 25 | 10 | 11.5 | 10.3 | 11.5 | 15.1 | 15.8 |
AA 28 | AA 56 | |||||||||||||
2-year survival (%) | GBM 33 | – | GBM 8 | – | GBM 41 | – | 35.9 | – | – | 22 % | – | – | – | – |
AA 100 | AA 53 | AA 88 | ||||||||||||
Median prescription isodose (%) | 62 mean | Mean 67 (40–80) | 70 | 80 (70–90) | 50 (40–90)a | – | 85 (60–100) | 50 (45–65) | 50 | 50 | 80 (50–100) | 74.9 (66–89) | 70 (50–80)a | 50 |
Median age (range) | 56 (35–79) | 57.7 (20–78) | 54 (5–74) | 42.1 (15–77) | GBM 51 (3–72) | 67.5 (45–78) | 51 (12–84) | 68 % >50 | 60.3 | 61 (19–79)a | 57.8 (33–81)a | 61.3 (27–81) | 58.6 (12–76) | 62 (12–84) |
AA 45 (3–73)a | ||||||||||||||
EBRT | 78 %, 45–60 Gy | 0–66 Gy | Median 59.4 Gy (44–62) | Median 60 Gy (54–60) | GBM all, mean 60 Gy | 60 Gy | 73/78 | All, 24/31 >59 Gy | All, median 60 Gy | All 60 Gy | All 50–64 Gy | 75 % EBRT (40–60 Gy) | 96 %, 45–66.6 Gy | All 60 Gy |
Chemo | 15 % | – | 47 % | None | From 1990 | None | 68 % | 100 %
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|