Fig. 61.1
Limbic system: OB olfactory bulb, LOT lateral olfactory striae, INS insula, UB uncinate bundle, DB diagonal band of Broca, AMYG amygdala, SCR subcallosal radiations, HYP hypothalamus, AT anterior thalamus, MB mammillary body, MTT mammillothalamic tract, ATR anterior thalamic radiations, ST stria terminalis, HAB habenula, MFB medial forebrain bundle, SM stria medullaris, HPT habenulointerpeduncular tract, IP interpeduncular nucleus, LMA limbic midbrain area, G nucleaus of Gudden, CG central gray, and CC corpus callosum. From Mindus P: Capsulotomy in Anxiety Disorders- A Multidisciplinary Study, Dissertation at the Karolinska Institute and Hospital, in. Stockholm, Sweden, 1991

Fig. 61.2
Neuroanatomical sites for various psychosurgeries are illustrated. From Mindus P: Capsulotomy in Anxiety Disorders—A Multidisciplinary Study, Dissertation at the Karolinska Institute and Hospital, in. Stockholm, Sweden, 1991
Pain
Radiosurgery has been used to treat different forms of pain including somatic pain (i.e. cancer-related or non-cancer-related), central pain, trigeminal neuralgia, and sphenopalatine neuralgia. All of these types of pain are a manifestation of different pathophysiological processes. There is not a single anatomical circuit or target that is most appropriate. Treatment can target central anatomic structures that mediate the pain sensation (e.g., thalamus) or can target the nerve that carries the pain sensation (e.g., trigeminal nerve in trigeminal neuralgia). The complexity of neuronal network mediating pain makes its management by open or closed stereotactic techniques largely unsatisfactory. Chronic pain targeting with radiosurgery has been typically performed at the level of the medial thalamus. Young targeted the intralaminar, mediodorsal centromedian, and parafascicular nuclei in chronic pain patients [11–13]. PET or functional MRI-guided cingulotomies have also been proposed for chronic pain treatment [14].
Trigeminal neuralgia (TGN) is a paroxysmal lancinating pain confined to a distribution encompassing one or more of the branches of the trigeminal nerve on one side of the face. As early as 1941, Olivecrona understood and described that mechanical pressure along the root or at the level of the ganglion could be the cause of trigeminal neuralgia [15]. In pioneering work, Granit, Leksell, and Skoglund (1944) demonstrated that local pressure on nerve fibers could result in painful afferent discharges from the injured neural segment [16]. More recently, Jannetta and others have suggested that vascular compression of the trigeminal nerve may be a causal agent in trigeminal neuralgia [17–19]. This fact led to the hypothesis of a causal relationship between vessel compression and trigeminal neuralgia and the devising of microvascular decompression surgery. Despite such hypotheses, the fact that balloon compression of the nerve can lead to symptomatic improvement in some patients and infections and demyelinating conditions may also affect the trigeminal nerve and illicit pain underscores the true lack of understanding as to the pathophysiology of trigeminal neuralgia [20, 21].
With radiosurgery, the usual target for treating trigeminal neuralgia is the trigeminal nerve root entry zone or the cisternal segment of the trigeminal nerve at the level of the pons. Much has been written about whether or not the trigeminal nerve should be targeted more proximally or distally [22–24].
Obsessive-Compulsive Disorder and Depression
The most common radiosurgical target for obsessive-compulsive disorder (OCD) is the anterior limb of the internal capsule. A capsulotomy can be performed on the right hemisphere, left hemisphere, or both. The anatomical site for a capsultomy is depicted in Fig. 61.3 [27] and the appearance on MRI is shown in Fig. 61.4. Lippitz et al. noted a correlation between clinical success and radiological lesioning of the middle of the anterior limb of the internal capsule [28]. This was defined as parallel to a plane encompassing the anterior commissure-posterior commissure line level at the level of the foramen of Monro and 4 mm rostral by a plane defined by the internal cerebral vein [29]. Cingulotomy can also be performed for OCD and depression [30]. In addition, limbic leucotomy involving bilateral lesions of the cingulum with subcaudate tractotomy have been advocated for intractable depression [31–33].



Fig. 61.3
An axial slice of the brain depicting the target areas for bilateral capsulotomies (asterisk). From Mindus P: Capsulotomy in Anxiety Disorders—A Multidisciplinary Study, Dissertation at the Karolinska Institute and Hospital, in. Stockholm, Sweden, 1991

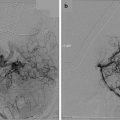
Fig. 61.4
Gamma Knife dose plan with isocenters depicted in yellow and the 6-month post-Gamma Knife coronal MRIs illustrating the imaging appearance of bilateral capsulotomies for intractable obsessive-compulsive disorder
Anxiety
Leksell was impressed with the result, yet disappointed with the prefrontal lobotomy technique made famous by Egas Moniz and Almeida Lima. He believed that the frontal lobes should have been surgically treated with more finesse, and that psychosurgery in general should have been more simple yet elegant. Drawing from the work of Henry Wycis in Philadelphia and the anatomical studies of Professor Meyer in London, Leksell used thermal injury to perform a stereotactic capsulotomy on a successful industrialist who was completely incapacitated by anxiety [2]. The result from their early case was good and prompted more psychosurgery using electrodes and later the Gamma Knife. For intractable anxiety disorders, bilateral capsulotomies have been performed with a similar target to that for OCD [28, 34, 35].
Treatment Alternatives
Chronic pain is initially treated with pharmacological treatment. Pain specialists utilize opioid agonists, nonsteroidal anti-inflammatories, local anesthetics, antidepressants, certain anticonvulsants, and muscle relaxants to optimize pain control. More recently, implantable drug delivery systems (e.g., morphine pumps), transcutaneous electrical nerve stimulation, spinal cord stimulators, and vagal nerve stimulators have been implanted to assist with the treatment of chronic pain [36–38]. Pain rehabilitation programs can also be of use.
For trigeminal neuralgia, medical management is the first line of treatment for patients. Medications such as carbamazepine, oxcarbazepine, phenytoin, gabapentin, and pregabalin are used to treat trigeminal neuralgia. However, many patients with this condition eventually fail medical therapy because of refractory pain or intolerable medication side-effects. More invasive treatment options include microvascular decompression (MVD) and percutaneous procedures such as glycerol rhizolysis, radiofrequency rhizotomy, percutaneous balloon microcompression, and peripheral nerve blocks [1, 18, 20, 21, 39–41].
Obsessive-compulsive disorder, depression, and anxiety are initially managed with pharmacological agents and psychiatric intervention/counseling. Heterocyclic compounds, monoamine oxidase inhibitors, selective serotonin reuptake inhibitors, bipolar agents, and anxiolytics/hypnotics have all been applied to these conditions with limited efficacy. Many of the patients with intractable OCD, depression, or anxiety have a high rate of comorbid Axis I diagnoses including personality disorders and other functional impairments further complicating the treatment and reducing the chances of a favorable therapeutic outcome [42]. Unfortunately, pharmacological therapies only benefit between 50 and 70 % of all OCD patients [43]. Fava and Davidson estimate that 29–46 % of depressed patients fail to respond to pharmacological agents [44].
In addition to pharmacological treatment, deep brain stimulation, vagal nerve stimulation, and transcranial magnetic stimulation have been utilized for OCD and depression [45]. The ability to reverse or modulate these neurological interventions adds to the attractiveness of these interventions over a more static lesioning achieved with radiosurgery. Electroconvulsive therapy has been utilized for depression. It typically has a transient benefit and must be readministered with some regularity.
The Argument in Favor of Radiosurgery
In most cases, radiosurgical treatment of pain and psychiatric disorders should be reserved for patients who demonstrate fairly severe symptoms and who fail medical management. However, as noted, this is not an inconsequential number of patients. In patients with psychiatric disease who require surgical intervention, functional radiosurgery offers several important clinical as well as scientific advantages over open techniques. The most important is patient tolerance. It is our experience that this psychologically vulnerable group of patients is much more willing to undergo a closed stereotactic procedure, which in contrast to open surgery, leaves minimal, if any, external marks. Theoretically, the gradual development of the radiosurgical lesion may also allow the patient to better psychologically adjust. The psychological rehabilitation phase is an important part of any psychosurgical procedure.
Stereotactic radiosurgery also does not carry the same type and degree of immediate or severe risks that open surgery (e.g., microvascular decompression, deep brain stimulation, etc) does. For instance, in a long-term series of microvascular decompression patients, there were the following risks from the series by Dr. Jannetta: 0.2 % death; 0.1 % brain stem infarct; and 1 % hearing loss 1. None of these complications were observed in our series nor were they associated with radiosurgical treatment of trigeminal neuralgia in other major centers. Complications from hardware and the risk of hemorrhage for deep brain and vagal nerve stimulators combine to yield a risk of 10–27 % [46–48]. Ultimately, the patient must choose the type of intervention he or she is willing to undergo. Such a choice inevitably involves a weighing of the relative risks and benefits of each intervention.
Of all the indications, stereotactic radiosurgery has been most embraced for the treatment of medically refractory trigeminal neuralgia. The widespread application of radiosurgery for trigeminal neuralgia is in part a testament to its acceptable degree of pain relief and few side effects. Radiosurgery for chronic pain, OCD, intractable anxiety, and depression has been applied with far less frequency. This fact stems in part from the notion that such patients are usually managed by other types of physicians (e.g., psychiatrists, pain specialists, etc.) who have little familiarity with radiosurgery. Moreover, radiation oncologists and neurosurgeons are generally uncomfortable with treating these types of disorders without the close involvement of appropriate specialists to evaluate and assist in the pre- and postoperative management.
Surgical Treatment Alternatives for Pain and Psychosurgeries
Open lesioning—Although the results of stereotactic or percutaneous lesioning (e.g., thalamotomy, radiofrequency rhizotomy, glycerol injection) have been well studied, and the beneficial effects are immediate, there remains the potential for complications such as intracranial hemorrhage, stroke, and infection. In addition, these procedures carry with them an anesthetic risk too.
Deep brain stimulation and vagal nerve stimulation—The advantages of stimulation techniques include the reversible nature of the process and the ability to modulate the neural stimulation over time. However, patients are again exposed to the risks of open surgery including infection, hemorrhage, and anesthesia. In addition, rates of hardware complications/failure are not trivial, and the batteries need periodic replacement necessitating another albeit minor surgical procedure [46–48].
Microvascular decompression for trigeminal neuralgia—This procedure remains the gold standard for surgical approaches to treat trigeminal neuralgia. Barker et al. reported excellent pain relief in 70 % of patients and partial pain relief in another 4 % at 10 years postoperatively from a microvascular decompression [17]. However, there were the following risks from the series by Dr. Jannetta: 0.2 % death; 0.1 % brain stem infarct; and 1 % hearing loss [49]. Burchiel et al. in 1988 noted a 3.5 % major recurrence rate and 1.5 % minor recurrence rate following invasive surgical approaches [50]. All surgical approaches including radiosurgery appear to have a “wearing off” effect in terms of pain relief over the years.
Radiosurgical Treatment Dosimetry
The dose must be planned so that the steepest isodose gradient of the dose distribution (usually between the 50 and 70 % isodose lines) coincides with the periphery of tissue being treated. This may require several overlapping fields of radiation, each using a different collimator size and a separate stereotactic focal point. Changing the relative time of radiation at each target may also change the isodose distribution. Finally, the radiation field may be altered by blocking some of the radiation sources, also known as plugging or shielding.
For radiosurgical capsulotomies and thalamotomies, focal lesions can be produced using a 4-mm collimator and 1–3 isocenters on each side for overlapping fields, creating a cylindrical lesion, with a maximum dose within the target volume of 200 Gy. The development of the lesions using such a plan has been followed by MRI and CT scans every 3 months. On T2-weighted images, a high signal appears in the target area after approximately 3 months. This signal is most likely produced by local edema. The edema extends a maximal volume at around 9 months and then slowly subsides. The edema is directly related to the dose and to the volume radiated. It may be sufficient to use only one isocenter and the 4-mm collimator. With these treatment parameters and a maximal dose of 180 Gy, a lesion measuring approximately 4 to 5 mm three can be expected within several weeks with only minimal transient edema. Centers have utilized maximal target doses of 120–200 Gy for radiosurgical treatment of OCD, intractable anxiety disorders, depression, and chronic pain [11, 13, 34, 35, 42, 51, 52].
Kihlstrom et al. propose that a minimum dose of 110 Gy using the 4 mm collimator is required to create a permanent lesion [35]. Friehs et al. in 1996 reported the following lesion size after delivering a dose of 160 Gy using a 4 mm collimator [51]:
Time (months) | Diameter of necrosis (mm) |
|---|---|
1 | 3 |
3 | 6 |
6 | 8 |
12 | 4 |
For trigeminal neuralgia, dose selection has been studied much more extensively. Most centers utilize maximal doses of 70–85 Gy [53–58]. Doses of 90 Gy or higher have been associated with increased risk of post-radiosurgical complications [55].
Case reports and small case series glossopharyngeal and sphenopalatine neuralgia treatment with radiosurgery have been published [25, 26]. We reported on the pain relief of a patient with glossopharyngeal neuralgia delivering 80 Gy to the glossopharyngeal meatus [59]. Pollock and Boes (2011) reported on a series of five patients with glossopharyngeal neuralgia who underwent Gamma Knife radiosurgery with a dose of 80 Gy to the distal portion of the glossopharyngeal and vagus nerves at the level of the jugular foramen [60]. Of these five patients, three experience benefit from radiosurgery, whereas two had no benefit and underwent microsurgery too with no apparent pain relief [60]. Pollock and Kondziolka performed Gamma Knife surgery twice on a patient with sphenopalatine neuralgia using a maximal dose of 90 Gy [25]. The patient underwent repeat Gamma Knife surgery for partial pain recurrence and remained pain free 2 years after repeat treatment. The North American Gamma Knife Consortium recently reviewed 17 patients who underwent Gamma Knife surgery for intractable sphenopalatine neuralgia. Favorable pain relief (Barrow Neurological Institute Grades I–IIIb) was achieved and maintained in 10 (59 %) of 17 patients at a median follow-up of 34 months.
Outcomes Based upon the Type of Radiosurgical Device
No trials have been performed to look at the results of psychosurgeries using different radiosurgical devices. In fact, very few psychosurgeries have been done with radiosurgical devices other than the Gamma Knife. However, other radiosurgical devices (e.g., the Cyberknife or Novalis) may be well suited for treating psychiatric conditions too.
Radiosurgical Treatment Outcomes
Pain Other than Trigeminal Neuralgia
Early results using the Gamma Knife to produce thalamotomies for pain control were published by Steiner et al. in 1980. All of the 52 patients treated suffered from terminal cancer and were treated prior to the advent of CT or MRI. Pneumoencephalography was used to target the thalamic centrum median-parafasciculus (CM-Pf complex). Good pain relief was obtained in 8 patients and moderate pain relief in 18. The patients had in general only temporary relief of pain. Of those with good pain relief, five died without recurrence of pain between 1 and 13 months after the procedure, and three had recurrence of pain at 3, 6, and 9 months, respectively. Doses between 100 and 250 Gy were tested. Observation of an actual lesion was only possible in 21 of 36 patients that had a postmortem examination. Not surprisingly, the presence of a lesion was associated with relief. Lesions were only reliably created with doses greater than 160 Gy. The collimators used were 3 × 5 and 3 × 7 mm. The most effective lesions were more medially located near the wall of the third ventricle, and the greatest relief was for face or arm pain [63].
These results were not particularly encouraging. However, with improvements in neuroimaging and alternate target selection, it is possible that more effective lesions can be produced. Recent reports seem to support this expectation. Hayashi et al. in 2003 reported significant pain reduction in patients with severe cancer pain and post-stroke thalamic pain after Gamma Knife lesioning of the hypophysis [64]. Using the 4 mm collimator and doses of 140–180 Gy, Young et al. have published effective pain relief in patients with chronic, intractable pain following medial thalamotomy with the Gamma Knife [11–13]. In a series of 15 patients followed for more than 3 months after a radiosurgical-induced medial thalamotomy, four (27 %) were pain free and five others (33 %) had greater than 50 % pain relief [13]. Additional investigation must be conducted before the role of the Gamma Knife for pain treatment can be fully defined.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree