and Zdeněk Fryšák1
(1)
Department of Internal Medicine III – Nephrology, Rheumatology and Endocrinology, Faculty of Medicine and Dentistry, Palacky University Olomouc and University Hospital Olomouc, Olomouc, Czech Republic
Keywords
Subacute granulomatous thyroiditisTendernessThyrotoxicosisFocal lesionRelapseCorticosteroid therapy5.1 Essential Facts
In 1904 the Swiss surgeon Fritz de Quervain published a complete work about “Subacute Nonsuppurative Thyroiditis”. The disease would later be known as “de Quervain’s thyroiditis” [1].
The incidence of subacute granulomatous thyroiditis (SGT):
12.1 per 100,000 per year.
higher in females (19.1 per 100,000 per year) than in males (4.4 per 100,000 per year).
highest in young adulthood (30–40 years), with 24 per 100,000 per year, and middle age (40–50 years), with 35 per 100,000 per year.
incidence declines with increasing age [2].
SGT is most likely caused by a viral infection and is generally preceded by an upper respiratory tract infection.
Clinical findings: SGT is indicated by painful swelling of the thyroid; at times, the pain begins and may be confined to the one lobe, but usually spreads rapidly to involve the rest of the gland (“creeping thyroiditis”). Pain may radiate to the jaw or the ears, and malaise, fatigue, myalgia, and arthralgia are common. A mild-to-moderate fever is expected, and at times a high fever of 40.0 °C may occur. A transient vocal cord paresis may occur. The disease process may reach its peak within 3–4 days and subside and disappear within a week, but more typically, onset extends over 1–2 weeks and continues with fluctuating intensity for 3–6 weeks. Thyrotoxicosis is present in 50% of patients in the acute phase [3, 4].
Physical examination: The thyroid gland is typically enlarged, smooth, firm, and tender to palpation [4].
Laboratory findings: There is a markedly elevated C-reactive protein (CRP), as well as an elevated erythrocyte sedimentation rate (a normal ESR essentially rules out the diagnosis). The leukocyte count is normal or slightly elevated, and levels of thyroid stimulating hormone (TSH) are low to undetectable. Thyroglobulin (TGB) is elevated (a normal level rules out the diagnosis), and the radioactive iodine uptake test (RAIU) is notably low [3, 4].
Therapy: anti-inflammatory medications and corticosteroids; therapy may improve clinical findings often within 24 h [4].
Course after therapy: Up to 20% of patients have the recurrence of SGT on discontinuation of prednisone. In 90% or more of patients, there is a complete recovery and a return to normal thyroid function. However up to 5–10% of the patients may become hypothyroid and require permanent replacement with levothyroxine [3, 4].
5.2 US Features of Subacute Granulomatous Thyroiditis [5]
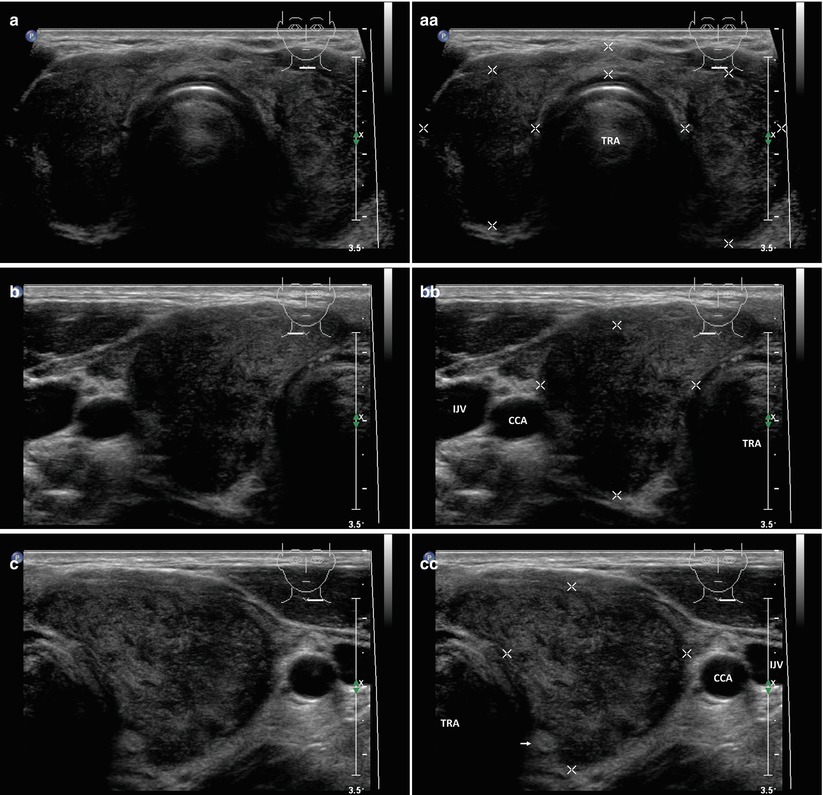
Unilateral thyroid involvement (Fig. 5.3aa) is more common than bilateral thyroid involvement (Figs. 5.1aa and 5.2aa).
Thyroid gland is typically enlarged, unilateral (Fig. 5.3aa), or bilateral enlargement (Fig. 5.1aa), but can be normally sized (Fig. 5.2aa).
In the affected lobe are focally ill-defined heterogeneously hypoechoic areas with an irregular or microlobulated margin (Fig. 5.2aa), without round or ovoid mass formation.
No hypervascularity (case of thyrotoxicosis) on the CFDS, typically minimal vascularity—pattern 0 (Fig. 5.1dd); normal (Fig. 5.1jj) or increased vascularity was seen in the recovery stage [6, 7].
Focal lesion can mimic thyroid carcinoma (Fig. 5.3aa), but the presence of pain or tenderness should allow differentiation of SGT from these other typically nontender entities [7].
Cytopathological examination for SGT reveals a severe inflammatory area, with non-caseating granulomas.
Heterogeneity of the thyroid affected by SGT can mimic the changes of Hashimoto thyroiditis as well. The differences are clinical and biochemical [7].
Characteristic findings of subacute thyroiditis on US in combination with the presence of neck pain can provide a more sensitive and specific diagnosis [7].
US performed 3 months or more (Fig. 5.3jj) from the initial US examination shows complete resolution of the changes [7].
On corticosteroid therapy, symptoms of SGT, the enlargement of thyroid gland, and laboratory signs of inflammation and thyrotoxicosis disappear quickly, in 2–6 weeks, but full normalization of thyroid gland structure during US follow up is slower, taking 2–6 months. SGT is mostly bilateral. Relapse (Fig. 5.3ff) after end of treatment is rare, but may be more severe than the first episode (personal observations).