Chapter 12 Subarachnoid Hemorrhage
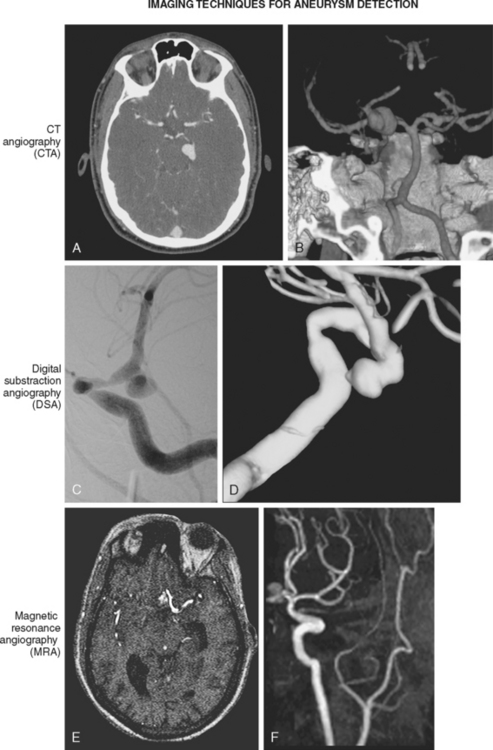
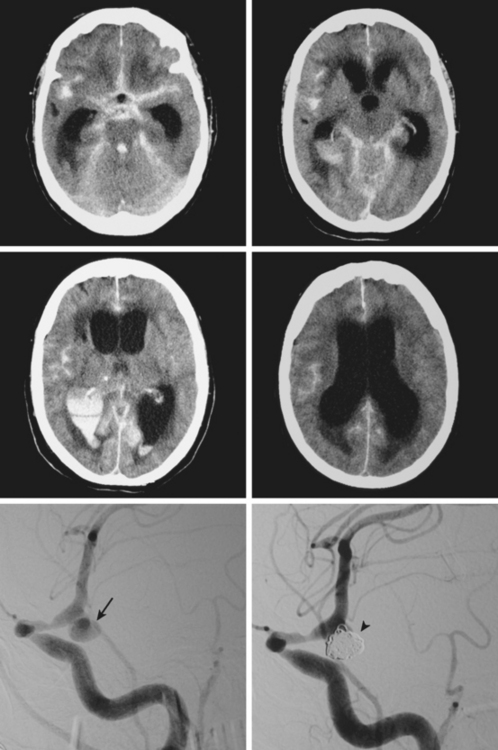
Advances in imaging technology have marked the great milestones in the history of the diagnosis and management of aneurysmal subarachnoid hemorrhage (SAH) and its complications. The development of cerebral angiography allowed in vivo visualization of saccular aneurysms, accomplished for the first time by Egas Moniz in 1933.1 It was not until 1951 that Ecker and Riemenschneider achieved the first angiographic proof of delayed vasospasm.2 Since its introduction in the 1970s, computed tomography (CT) scan has become the most reliable tool for the acute diagnosis of SAH. It did not take long before it was recognized that the amount of blood in the subarachnoid cisterns (Figure 12-1) was highly predictive of the subsequent risk of vasospasm.3–5 Transcranial Doppler (TCD) later proved valuable for noninvasive screening and monitoring of vasospasm.6 More recently, magnetic resonance imaging (MRI) techniques have enhanced our understanding of ischemic damage after SAH7 and may represent a valuable tool for the acute diagnosis of ongoing ischemia from vasospasm.8 As spiral CT angiograms9 and CT perfusion scans10 move into the scene, we may see another transformation in the management of SAH led by imaging technology in the immediate future.
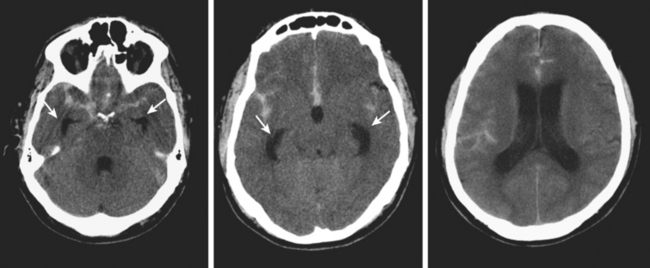
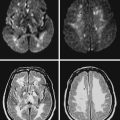
Timely and accurate diagnosis of SAH hinges on the use of brain imaging. CT scan remains by far the most widely applied technique. Its sensitivity for the acute diagnosis of SAH exceeds 95%.11 However, CT scan is most reliable early after the bleeding (particularly within the first 24–48 hours) and false-negative results become possible after a few days. Gradient-recall echo T2* MRI has comparable sensitivity to CT scan for the hyperacute diagnosis of SAH,12 and fluid-attenuated inversion recovery (FLAIR) MRI has greater sensitivity than CT scan in subacute cases (Figure 12-2).13
Currently, the use of MRI is limited because MR technology is often unavailable in the emergency setting, and CT scanning allows faster image acquisition (which becomes an important factor in patients with acute SAH who are neurologically or hemodynamically unstable) and easier visualization of extravasated blood (at least for examiners without extensive radiological training). False-positive diagnoses of SAH (pseudo-SAH) by CT scan may be caused by increased venous congestion, as seen in patients with massive cerebral edema or bilateral subdural hematomas.14–16
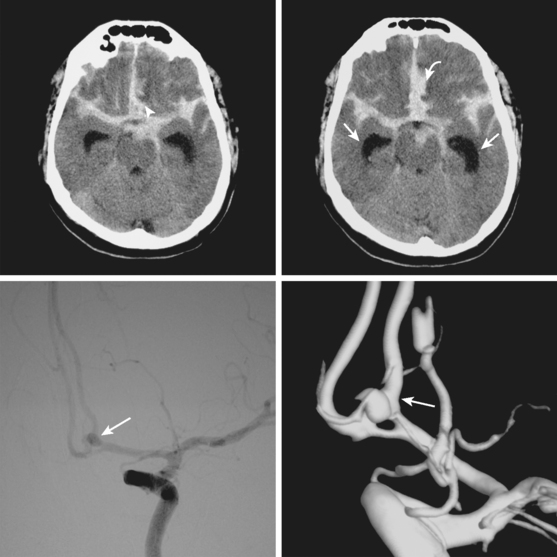
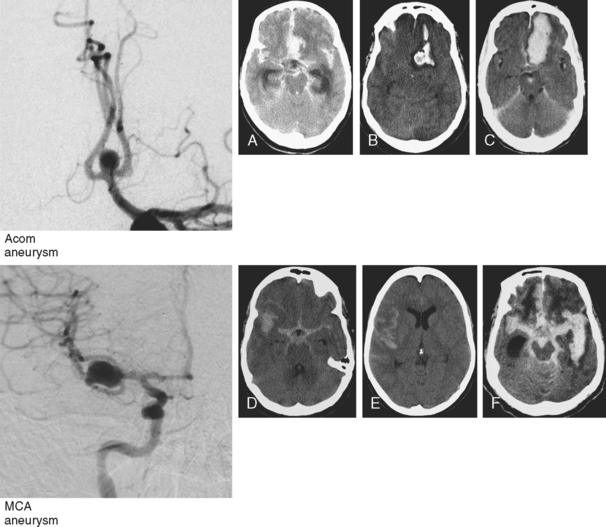
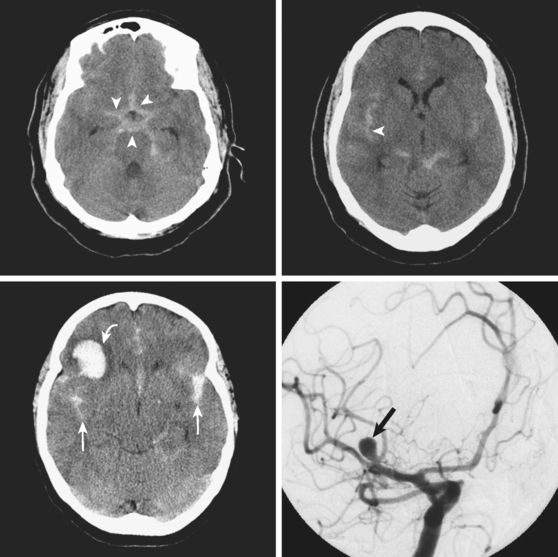
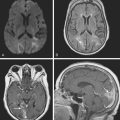
Although it is generally agreed that the amount of subarachnoid blood visualized on CT scan predicts the risk of subsequent vasospasm, there is still debate regarding the best way to quantify this risk. The grading originally proposed by C. M. Fisher et al. is still the most popular (Table 12-1; Figure 12-3).5 However, newer visual scales17 (Table 12-1) and software-based techniques18 have claimed better sensitivity and specificity. CT scan is also the modality of choice for the prompt diagnosis of hydrocephalus and rebleeding, and it clearly demonstrates the presence of global cerebral edema, a strong predictor of unfavorable outcome.19
TABLE 12-1 Predicting delayed cerebral ischemia by the appearance of the initial CT scan of the brain: Comparison of the traditional Fisher radiological grading scale and a proposed modification that incorporates the impact of IVH on the risk of vasospasm and delayed ischemic damage
| Grade | Fisher scale | Modified Fisher scale |
|---|---|---|
| 0 | No SAH or IVH | |
| 1 | No SAH or IVH | Minimal/thin SAH, no IVH in both lateral ventricles |
| 2 | Diffuse, thin SAH, no clot > 1 mm in thickness | Minimal/thin SAH with IVH in both lateral ventricles |
| 3 | Thick layer of SAH of localized subarachnoid clot > 1 mm in thickness | Thick SAH*, no IVH in both lateral ventricles |
| 4 | Predominant IVH or intracerebral hemorrhage without thick SAH | Thick SAH* with IVH in both lateral ventricles |
CT, computed tomography; IVH, intraventricular hemorrhage; SAH, subarachnoid hemorrhage.
* Completely filling ≥ 1 cistern or fissure.
Conventional cerebral angiography remains the gold standard for the diagnosis of intracranial aneurysms (Figure 12-4).20 Whereas noninvasive angiograms may be sufficient for screening of unruptured intracranial aneurysms, diagnosis of nontraumatic SAH demands the performance of catheter angiography. Newer imaging processing techniques currently allow three-dimensional reconstruction of the aneurysm, which greatly enhances the anatomical definition of the study.21 After diagnosis, endovascular coiling may be performed during the same catheterization. Conventional angiography is also considered the gold standard for the diagnosis of vasospasm and enables its treatment with angioplasty or superselective intra-arterial infusion of vasodilators in selected cases.22,23
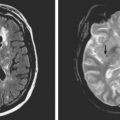
The role of MRI in the management of SAH and vasospasm continues to grow. Initially it was used to define the extent of delayed ischemic damage with exclusive prognostic purposes. MRI has considerably greater sensitivity than CT scan for the recognition of small foci of subcortical ischemia that commonly occur as sequelae of SAH, predominantly affecting the basal ganglia, claustrum, and frontal white matter.7 More recently, diffusion-weighted imaging and perfusion-weighted imaging have started to be employed for the acute detection of cerebral ischemia during the phase of vasospasm.8,24,25 These techniques may demonstrate hypoperfusion and ischemia even in patients with no definite evidence of vasospasm by either TCD or angiogram, suggesting that mechanisms other than luminal narrowing of large intracranial vessels may be responsible.
CT-based protocols combining CT perfusion with spiral CT angiograms may constitute a valuable alternative to the current practice of TCD screening and angiographic confirmation of vasospasm. These CT studies may provide direct evidence of the presence and magnitude of hypoperfusion and correlate that information with a fast and noninvasive depiction of the state of the major intracranial vessels.8–10,26 Further research to confirm the validity of these CT-based protocols is necessary to determine their optimal application.
As our understanding of the complex pathophysiological underpinnings of vasospasm improves, it appears increasingly evident that ischemia after SAH may be caused by disruption of microcirculatory function.20,27 New imaging modalities capable of providing dynamic information on the status of the microcirculation are likely to be the best candidates to forge the next revolution in the care of patients with SAH.
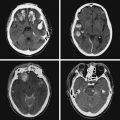
A 46-year-old woman developed thunderclap headache immediately followed by transient loss of consciousness associated with tonic posturing deemed suspicious for a seizure. She was emergently transferred to a local hospital. On initial examination, her Glasgow coma scale sum score was 13. She did not have cranial nerve deficits or hemiparesis (WFNS grade II). Her CT scan of the brain showed extensive SAH with a thick cisternal clot in the interpeduncular cistern (Fisher grade 3; Figure 12-5, upper row). There was also incipient hydrocephalus and a small left parasagittal frontal hematoma. Digital substraction angiography (DSA) disclosed a saccular aneurysm in the anterior communicating artery region, arising from the left A1 segment (Figure 12-5, lower row, left panel). The anatomical configuration of the aneurysm was much better visualized on the three-dimensional reconstructed images (Figure 12-5, lower row, left panel). The ruptured aneurysm was successfully coiled on the second day after the bleeding. Four days later, the patient developed some deterioration in the level of consciousness associated with doubling of the mean blood flow velocities in the left terminal carotid segment and the left A1 and M1 segments; similar but less severe changes were present on the right anterior circulation. The diagnosis of diffuse, severe vasospasm was confirmed angiographically. The patient improved rapidly with hemodynamic augmentation therapy and had no other complications. At 3 months, she still had mild neurobehavioral problems and occasional headaches. Six months later, she was feeling well and had returned to work, although she reported decreased endurance.
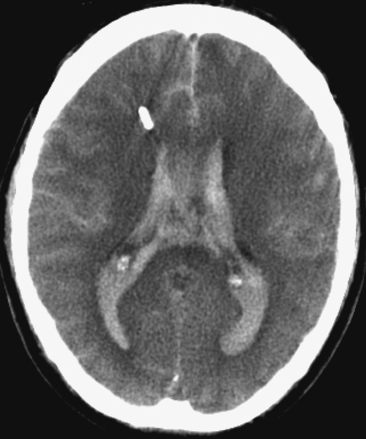
Figure 12-7 Example of extensive subarachnoid hemorrhage and intraventricular hemorrhage (“casted ventricles”).
CAUSES OF EARLY DETERIORATION: REBLEEDING AND HYDROCEPHALUS
GLOBAL CEREBRAL EDEMA
CEREBRAL VASOSPASM
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree