Alcohol
Phenol
Mechanism of action
Dehydration, phospholipid extraction leading to Wallerian denaturation
Protein coagulation, segmental demyelination, and necrosis of all neural elements
Concentration (%)
50–100
5–10
Clinical onset
Fast
Slow
Clinical duration
Long
Short
Pain on injection
Yes
No
Patient Selection
These blocks may be associated with morbidity, and it is prudent to understand the indications, the relevant anatomy, and the appropriate patient selection. Patients with moderate to severe pain not controlled with oral analgesics and/or medication-related side effects are ideal candidates for interventional therapy.
Indications
Acute intervention for acute pain
Temporary treatment for chronic pain conditions until medication shows efficacy
Pain affecting the pelvic visceral structures
SHP: descending and sigmoid colon, rectum, bladder, prostate, prostatic urethra, testes, seminal vesicles, vaginal fundus, uterus, and ovaries
GI: distal vagina, distal rectum, distal urethra, vulva, and perineum
Malignant-related pain unresponsive to oral or parenteral medications (neurolysis)
Excessive sedation or unacceptable side effects from oral or parenteral medications
Contraindications
Patient refusal
Coagulopathy
Local/intra-abdominal infection and sepsis
Equipment
Superior Hypogastric Plexus Block
Preparation kit, sterile gloves, surgical cap and mask, 18-gauge introducer needle, 22-gauge 5- or 7-in. spinal needle, extension tubing
Fluoroscope
Medications
Lidocaine 1%
Contrast media (e.g., iohexol)
Bupivacaine 0.5% or ropivacaine 0.5% and lidocaine 2%
Cefazolin 1 g (for intravenous infusion)
Ganglion Impar Block
Preparation kit, sterile gloves, surgical cap and mask, 22-gauge 3.5-in. spinal needle, extension tubing
Fluoroscope
Medications
Lidocaine 1%
Contrast media (e.g., iohexol)
Bupivacaine 0.5% or ropivacaine 0.5% and lidocaine 2%
Neurolysis (Superior Hypogastric and Ganglion Impar)
Preparation kit, sterile gloves, surgical cap and mask, 22-gauge 5- or 7-in. spinal needle (SHP) or 3.5-in. spinal needle (GI), extension tubing
Fluoroscope
Bupivacaine 0.5% or ropivacaine 0.5%
50–100% alcohol or 5–10% phenol
Technique
Superior Hypogastric Plexus Block (Transdiscal Approach)
Fluoroscopy guidance is recommended and is described. The patient is placed on the fluoroscopy table in the prone position. After sterile preparation and drape have been accomplished, an anterior-posterior (AP) fluoroscopic image of the lower lumbar spine is obtained, centered on the L5–S1 junction. The end plate of the sacrum is aligned, reducing parallax. The fluoroscope is angled obliquely 25–30° until the superior articular process of the sacrum is approximately one-third of the lateral portion of the disk and 25–30° cephalad, placing the L5–S1 intervertebral disk space into plane view. A site just lateral to the superior articular process “the window” is marked and anesthetized using 1% lidocaine (Fig. 23.1). An 18-gauge spinal introducer needle is inserted and advanced under coaxial technique and intermittent fluoroscopic guidance towards the L5–S1 intervertebral disk. Following this, a 5-in. or 7-in. 22-gauge spinal needle is inserted through the 18-gauge introducer needle. The spinal needle is then advanced to enter the intervertebral disk (Fig. 23.2). The fluoroscope is rotated to lateral position, and the needle is advanced under intermittent fluoroscope until the needle is observed to be anterior to the L5–S1 disk. Then, 1–3 ml of contrast medium (Omnipaque 300 M) is injected anterior to the disk confirming correct needle placement (Fig. 23.3). An AP view is obtained confirming midline placement of the needle (Fig. 23.4). Following this, 8 ml of lidocaine 2%, 8 ml of bupivacaine 0.5% (16 ml total) is then injected with negative aspiration every 3 ml, utilizing intermittent fluoroscopy tracking the spread of the residual contrast anterior to the L5–S1 disk. Neurolysis is performed with phenol 5–10 ml of 5–10% or 5–10 ml of 50–100% alcohol. The needle is flushed with 2 ml of lidocaine 1% to prevent tracking of neurolytic agent and retracted from the subcutaneous tissue and skin.
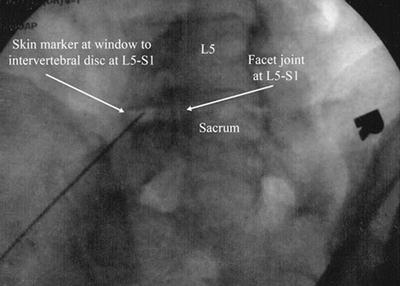
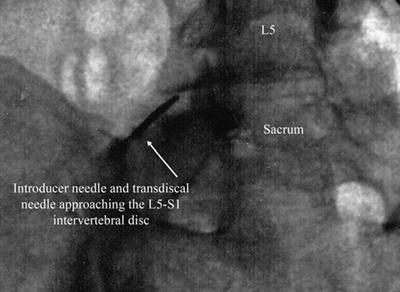
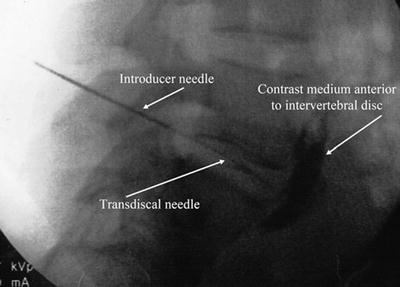
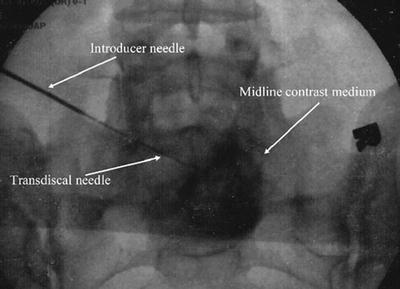
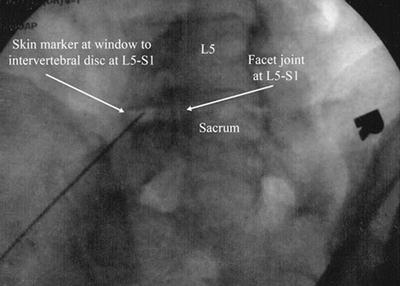
Fig. 23.1
Oblique radiographic view of entrance site
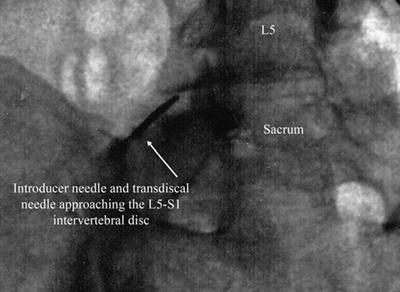
Fig. 23.2
Oblique radiographic view of transdiscal needle
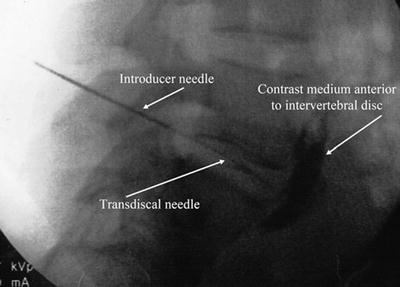
Fig. 23.3
Lateral radiographic view of transdiscal needle
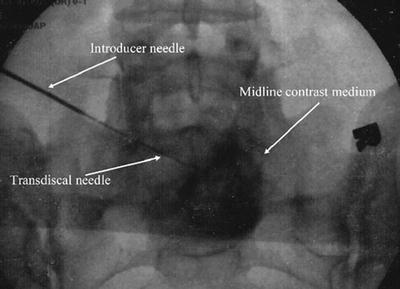
Fig. 23.4
AP radiographic view of transdiscal contrast medium
Ganglion Impar Block (Transsacrococcygeal Approach)
Fluoroscopy guidance is recommended and is described. The patient is placed on the fluoroscopy table in the prone position. After sterile preparation and drape have been accomplished, an anterior-posterior fluoroscopic image of the sacrum is obtained. The ganglion impar block is approached by rotating the fluoroscope to the lateral position and anesthetizing the area overlying the sacrococcygeal junction. A 3.5-in. 22-gauge spinal needle is inserted and advanced under intermittent fluoroscopy towards and into the sacrococcygeal disk (Fig. 23.5). The needle is advanced until the needle is witnessed anterior to the sacrococcygeal disk. One to 3 ml of contrast medium (Omnipaque 300 M) is injected anterior to the disk, confirming correct needle placement. This may produce a “comma sign” in the lateral view (Fig. 23.6




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








