Knowledge of relevant anatomy and underlying mechanisms of traumatic injury is essential for understanding the radiologic findings in craniofacial trauma and their clinical importance. Craniofacial anatomy is diverse, and as a result of this anatomic diversity, physicians from numerous different specialties scrutinize similar imaging sets, looking for different pathologic abnormalities within the same anatomic regions. Radiologists familiar with the chief concerns of this anatomically diverse region can help expedite the decision-making process by keeping those concerns in mind when they report their findings. This review provides an overview of situations wherein surgical management may be indicated.
Key points
- •
The craniofacial skeleton and the associated viscera and soft tissue encompass a range of systems, all serviced by different medical and surgical specialists.
- •
Patients with traumatic injuries involving craniofacial anatomy will often require multidisciplinary management, and prioritizing their multiple problems is critical to providing efficient and effective care.
- •
Radiologists who are familiar with some of the chief concerns of the surgeons that manage this anatomically diverse region can help expedite the decision-making process by keeping some of these concerns in mind when they report their findings.
- 1.
Review the primary imaging modalities used for assessing craniofacial trauma.
- 2.
Review the mechanisms behind the various injuries seen in craniofacial trauma patients.
- 3.
Discuss craniofacial injuries that require surgical management.
- 4.
Discuss elements of craniofacial imaging studies that are critical to the surgeon for surgical planning and decision-making.
Introduction
The key to understanding the radiologic evaluation of craniofacial trauma is through a thorough knowledge of anatomy and mechanisms of traumatic injury. Craniofacial anatomy is diverse. Bony elements include the anterior skull vault, skull base, and the facial skeleton. The viscera contained in the craniofacial skeleton consist of the frontal lobes, orbital contents, segments of all the cranial nerves, the upper airway, and the digestive tract. In addition to the individual components, structural areas must be assessed as a whole. As a result of this anatomic diversity, physicians from numerous different specialties scrutinize similar imaging sets, although looking for very different pathologic abnormalities within the same anatomic regions. A well-run trauma center can convey relevant pathologic abnormality to the appropriate services with speed, accuracy, and efficiency. It is important to have a firm understanding of injuries representing a surgical emergency versus those that may be more appropriate for less urgent intervention. The elements of imaging studies most relevant to the surgeon managing a craniofacial trauma patient are discussed.
Introduction
The key to understanding the radiologic evaluation of craniofacial trauma is through a thorough knowledge of anatomy and mechanisms of traumatic injury. Craniofacial anatomy is diverse. Bony elements include the anterior skull vault, skull base, and the facial skeleton. The viscera contained in the craniofacial skeleton consist of the frontal lobes, orbital contents, segments of all the cranial nerves, the upper airway, and the digestive tract. In addition to the individual components, structural areas must be assessed as a whole. As a result of this anatomic diversity, physicians from numerous different specialties scrutinize similar imaging sets, although looking for very different pathologic abnormalities within the same anatomic regions. A well-run trauma center can convey relevant pathologic abnormality to the appropriate services with speed, accuracy, and efficiency. It is important to have a firm understanding of injuries representing a surgical emergency versus those that may be more appropriate for less urgent intervention. The elements of imaging studies most relevant to the surgeon managing a craniofacial trauma patient are discussed.
Anatomy
Visceral Anatomy
Patients who present with a history and physical examination suggestive of a severe head injury should undergo initial evaluation with a noncontrast head computed tomography (CT), particularly if there is any neurologic deficit or airway compromise. Common screening strategies that direct decision-making for CT evaluation include the New Orleans Criteria and the Canadian Head CT Rule. Although a routine CT will adequately screen for major injuries and intracranial pathologic abnormality, more dedicated studies may be indicated to help characterize the nature of the patients’ injuries. Patients who have suspected or known facial fractures should undergo further imaging using thinner slices through the face, using both bone and soft tissue algorithms.
The craniofacial viscera are imaged in the acute trauma setting with CT. If there is an indication for further imaging, specifically with respect to the intracranial contents and the globes, a magnetic resonance (MR) imaging is typically obtained at a later time. An MR imaging protocol for a craniofacial trauma patient should include T1 and T2 weighted sequences, fluid attenuated inversion recovery (FLAIR), susceptibility weighted imaging (SWI) or gradient echo (GRE), and diffusion-weighted imaging (DWI) sequences, with scans acquired in the axial, coronal, and sagittal planes. Typically, the information gleaned from an MR image is not used in determining immediate surgical indications. However, information obtained on an MR image may help clarify a presentation that is not explained by CT findings alone. Such information may, for example, determine whether a patient needs intracranial pressure monitoring.
MR imaging becomes especially helpful in cases of severe traumatic brain injury, or when patients have undergone or will undergo a decompressive procedure. If the degree of axonal and neuronal damage is so severe that a significant recovery is not likely, it could impact the willingness of both the surgeon to operate and the family to consent to a procedure. Although decompressive craniectomies can be lifesaving, it is important for family members to have realistic expectations regarding a patient’s long-term outcome; information provided by GRE/SWI and DWI in the acute and subacute periods can help the surgeon set realistic recovery goals ( Fig. 1 ). Thus, “heroic” procedures may not be offered given additional negative prognostic findings on the MR study.
Vascular Anatomy
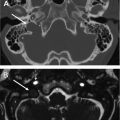
Vascular anatomy of the craniofacial region includes the carotid arteries and vertebrobasilar circulation, as well as the venous drainage of the head and neck. Direct evidence of, or mechanisms of injury suggesting (eg, distracting injuries), vascular injury should always be considered on initial imaging, even though noncontrast CT is not the proper imaging modality for such a diagnosis ( Fig. 2 ). Injury to the carotid canal, sella turcica, or dural venous sinuses should prompt further evaluation with a dedicated vascular study, such as CT or MR angiography (CTA and MRA, respectively), or digital subtraction angiography (DSA). CTA and MRA both have various strengths and weaknesses. In general, CTA is often more practical in the trauma setting, because it is a quicker study to obtain, and it is more widely available. CTA typically involves a submillimeter overlapping axial acquisition, and a rapid bolus contrast injection using a vessel tracking technique. If there is a high likelihood of an indication for intervention, the patient may be taken directly for a DSA, which can also provide a possible venue for endovascular treatment of some vascular injuries.
Skeletal Anatomy
The craniofacial skeleton is typically evaluated with a submillimeter data set, reconstructed at 1 to 3 mm in the axial, coronal, and sagittal planes. It is useful to consider the facial buttress system when evaluating the craniofacial skeleton ( Fig. 3 ). The facial buttress system is divided into vertical and horizontal buttresses, with the vertical buttresses absorbing the bulk of the force generated during mastication. The vertical buttresses consist of paired medial, lateral, and posterior buttresses, as well as a single midline buttress. Horizontal buttresses are present in each facial-third connecting and reinforcing the lateral buttresses. The facial buttresses generally correlate with ideal lines of osteosynthesis and are thus an important consideration in facial plating. Accurate knowledge of the fracture pattern and how it impacts the facial buttress system guides the craniofacial surgeon in appropriate restoration of form and function.
Imaging findings
Plain films no longer play a significant role in evaluating craniofacial trauma. Patients with outward signs of facial trauma should have a noncontrast head CT on arrival in the hospital. Assessment of imaging should be systematic and comprehensive. A useful scheme is to assess the intracranial contents first for overt pathologic abnormality. Next, the soft tissues should be examined for signs of trauma, because this will direct attention to scrutinize other structures in that area, and along the same line of force that may be impacted. Next, the bony structures are assessed, starting superficially with the cranial vault, orbits ( Box 1 ), nasal bones ( Box 2 ), and sinuses ( Box 3 ), then moving attention to the deeper structures and the skull base ( Box 4 ).
- •
Identify any grossly abnormal globe position
- •
Quantify the size of the fracture defect
- •
Assess the integrity of the lamina papyracea
- •
Identify involvement of the infraorbital canal
- •
Evaluate for orbital fat herniation, and comment on volume, as high-volume herniation contributes to entrapment
- •
Compare the ocular muscles on each side to assess for contusion
- •
Evaluate for globe injury
- •
In children, assess for trapdoor fractures
- •
Differentiate high and low defects from fractures
- •
Look for soft tissue swelling or other local evidence of trauma to determine fracture acuity
- •
Most fractures will occur in the transverse plane
- •
Crossing the plane of the nasal bone differentiates the nasociliary groove from a fracture
- •
Look for involvement of the maxilla
- •
Determine if there is an associated NOE or midface fracture
- •
Inspect the septum for swelling or deviation to diagnose septal hematoma
- •
Identify the fracture as displaced or nondisplaced
- •
Identify concomitant nasofrontal and NOE fractures
- •
Evaluate the integrity of the nasofrontal duct
- •
Evaluate the posterior table and comment on comminution, dural injury, and injury to adjacent frontal lobe
- •
Identify directionality: transverse versus longitudinal
- •
Evaluate the integrity of the otic capsule
- •
Assess for involvement of the ossicular chain
- •
Assess the carotid canal
- •
Look for the presence of pneumolabyrinth
- •
Evaluate the venous structures for injury and/or thrombus
- •
Evaluate the integrity of the tegmen tympani
Critical in the initial evaluation of head CT studies in trauma is the search for intracranial hemorrhage and mass effect, followed by evaluation for more subtle findings. After the intracranial contents have been thoroughly assessed, the bony elements are evaluated. The radiologist should keep fracture patterns in mind, along with frequently missed areas, such as the lamina papyracea, orbital rims and floor, nasolacrimal duct, carotid canal, temporal bones, and orbital apex. The radiologist should conclude with the occipital condyles, C1 and C2 vertebrae and the rest of the craniocervical junction, and the skull base. Based on initial findings, further studies may be recommended, such as dedicated imaging of the facial bones or sinuses, angiographic studies, and/or MR imaging.
Pathologic abnormality
Cranial Injuries
Cranial injuries can be categorized broadly into soft tissue, bony, and hemorrhagic injuries. The soft tissue of the cranium is essentially limited to the scalp. As such, diagnosis of injury here is not heavily reliant on imaging, with the possible exception of detection of foreign bodies. Although a growing subgaleal hematoma could require surgical intervention, such a problem should readily manifest itself on a physical examination. Skull fractures are discussed later with injuries to the craniofacial skeleton.
Hemorrhagic injuries
Hemorrhagic injuries are grouped into intra-axial and extra-axial lesions. Intra-axial blood is confined to the parenchyma, whereas extra-axial blood can be found anywhere in the ventricles or in the spaces between the calvarium and the cortex. Most of the traumatic hemorrhagic pathologic abnormalities can have atraumatic analogues that may change further diagnostic testing and management indications. Although the clinical history will typically clarify such an ambiguity, there are frequently cases where the causality between a hemorrhage and a trauma is not clear. For instance, a fall down a flight of stairs could result in traumatic subarachnoid hemorrhage; likewise, an aneurysm that ruptures in a patient who is walking down a flight of stairs could also cause a fall but would also have subarachnoid hemorrhage of a disparate cause. Patients are also frequently “found down,” and the volume of hemorrhage on a head CT may be out of proportion to a ground level fall. Noting discrepancies between the size of a given hemorrhage, and the absence of other signs of trauma, such as soft tissue injuries, skull fractures, and contrecoup injuries ( Fig. 4 ), can help the trauma team and surgeons initiate appropriate management algorithms. In these instances, MR imaging is often useful for assessing diffuse axonal injury (DAI) and other subtle findings that may be difficult to identify on CT.
Intra-axial injury
Intra-axial injury can take the form of intracerebral or intracerebellar hematomas ( Fig. 5 ), edema, contusions, and DAI. Both cortical contusions and intracerebral hematomas are the result of impact disrupting the vessels supplying the area of injury. If there is sufficient force, the injury at the impact site—or “coup” injury—may have a contrecoup sibling injury (see Fig. 4 ). Although a coup injury is the result of direct impact, contrecoup injuries are a result of the acceleration forces generated in areas of brain parenchyma that are distant from the impact point. Although common viewpoints are that coup and contrecoup injuries must be categorized along the same line of force, this is not actually the case.
The rotational acceleration underlying contrecoup lesions may also cause the microhemorrhages indicating severe DAI, depending on the mechanism of impact. Microhemorrhages occur when sheer stress injures the small vessels at points of the neuraxis joining a relatively mobile structure with one that is fixed. Anatomic sites especially prone to microhemorrhages include the corpus collosum, centrum semiovale, periventricular white matter, and the brainstem (see Fig. 1 ).
Surgical indications arise when these conditions increase intracranial pressure, necessitating a decompressive procedure and/or evacuation. DAI is not of great concern in the acute period. As mentioned earlier, widespread hemorrhagic or ischemic DAI may influence the decision to intervene surgically at a later date in a patient’s hospital course, as it is a poor prognostic factor.
Extra-axial injuries
Extra-axial hemorrhage occurs in the subdural, epidural, subarachnoid, or intraventricular spaces. Intraventricular hemorrhage will rarely occur in isolation, and when it does, atraumatic causes should be explored. Subdural hematomas can occur when bridging veins between the dura and the arachnoid are disrupted ( Fig. 6 ). This disruption can occur as a result of direct impact, but is more commonly due to inertia. Elderly people are especially susceptible to subdural hematomas, because cortical atrophy places greater stress on the bridging veins. Subdural hematomas are not bound by dural attachments and thus may cover the entire convexity.
Epidural hematomas are usually associated with a skull fracture at the site of hemorrhage; the fracture fragments tear a dural artery or vein and the blood will collect in the epidural space. Because epidural blood will be contained by dural attachments to the skull, these will typically have a lenticular shape and will have significant mass effect and sulcal effacement ( Fig. 7 ). Epidural bleeding is most commonly arterial, but it can be venous as well.
For epidural and subdural bleeding, the volume of hemorrhage and/or degree of mass effect is often used as a metric for surgical intervention. Furthermore, evidence of active bleeding, such as a “swirl sign,” could indicate the need for an emergent evacuation (see Fig. 7 ).
Traumatic subarachnoid hemorrhage is not always an indication for surgery or even advanced imaging, provided the referring clinicians are confident that the cause is trauma and not a vascular event. If there is any question as to the cause of the hemorrhage, the patient should be sent for vascular imaging. When there is a discrepancy between the mechanism of injury and the pattern of hemorrhage, there should be a low threshold for vascular imaging, because failure to treat aneurysmal bleeding or a ruptured arteriovenous malformation can have devastating consequences. Nonaneurysmal subarachnoid hemorrhage is not trivial, despite the lack of indication for intervention, as it has been shown to be an independent predictor of poor outcomes. It is, however, important to distinguish it from aneurysmal subarachnoid hemorrhage to prevent unnecessary and expensive vascular diagnostic studies, given the additional issues of radiation and contrast nephropathy.
Surgical management of traumatic brain injury
Common guidelines for surgical intervention combine radiologic findings with the patient’s mental status and overall clinical condition. The Brain Trauma Foundation Guidelines for the surgical management of various hemorrhagic conditions are outlined in Table 1 . Although the more detailed statistics may not necessarily be of great importance to the radiologist, the nature of the radiological criteria should be taken into careful consideration. Accurate documentation of findings, such as degree of midline shift, volume of hemorrhage, or the change in one of those metrics between serial studies, can help surgeons in their decision-making process. A commonly used method for quickly calculating hemorrhage volume is the ellipsoid, or “ABC method,” described in Fig. 8 .
| Pattern of Hemorrhage | Indications for Surgical Management |
|---|---|
| Epidural | Volume >30 cm 3 |
| GCS <9 with focal neurologic deficit | |
| Subdural | >10-mm thickness |
| >5-mm midline shift | |
| |
| Intracerebral | Volume >50 cm 3 |
| Medically refractory ICP | |
| Neurologic deterioration | |
| |
| Posterior fossa |
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree