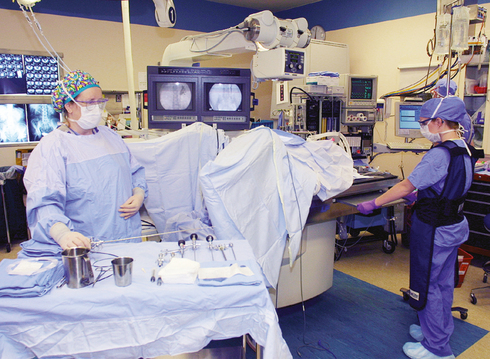
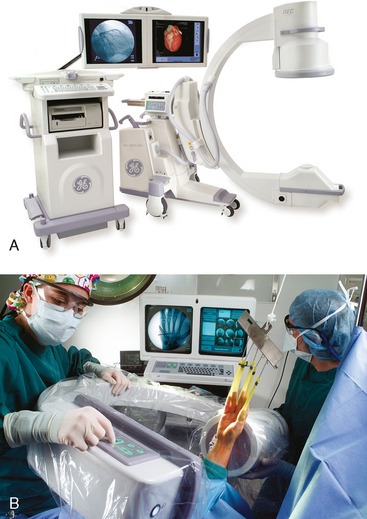
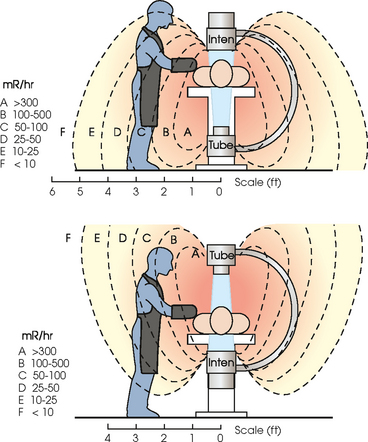
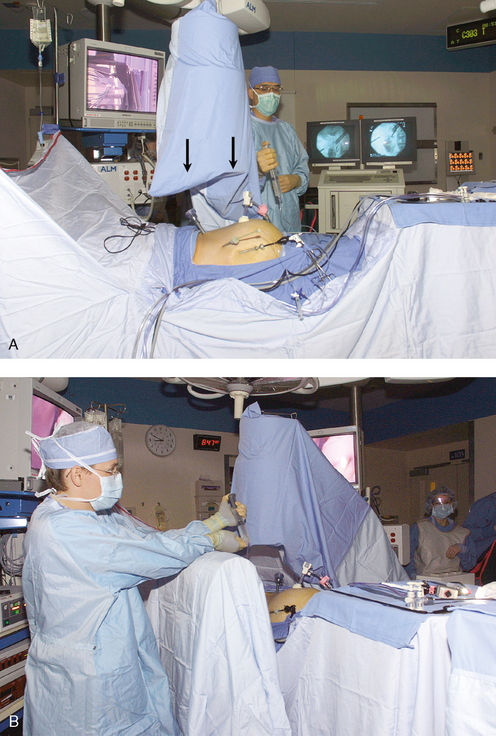
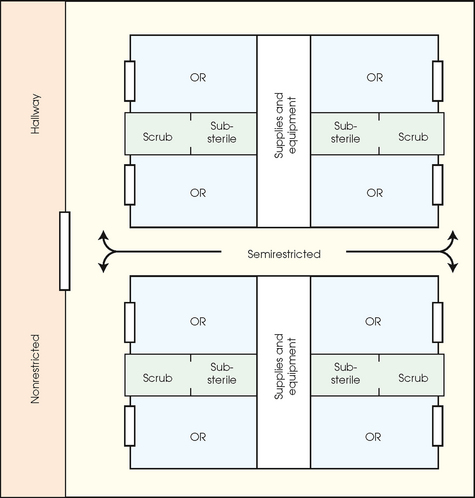
29 Surgical radiology is a dynamic experience. The challenges a radiographer encounters in the surgical suite are unique. Knowing the machinery and its capabilities and limitations is most important; in that regard, the radiographer can enter any operating room (OR) case, whether routine or extraordinary, and, with good communication, be able to perform all tasks well. An understanding of common procedures and familiarity with equipment enables the radiographer to perform most mobile examinations ordered by the physician. Surgical radiography can be a challenging and exciting environment for the radiographer but can also be intimidating and stressful. Surgical radiology requires educated personnel familiar with specific equipment routinely used during common surgical procedures. It requires expertise in teamwork. Preparedness and familiarity with equipment are key. Standard health and safety protocols must be followed to avoid contamination and to ensure patient safety. These are the basics, and the pieces come together in surgical radiology in distinctive ways. This chapter focuses on the most common procedures performed in the surgical area. The basic principles of mobile imaging are detailed, and helpful suggestions are provided for successful completion of the examinations. This chapter is not intended to cover every possible combination of examinations or situations that a radiographer may encounter, but rather provides an overview of the surgical setting and a summary of common examinations. The scope of radiologic examinations in a surgical setting is vast and may differ greatly among health care facilities (Box 29-1). The goals of this chapter are to (1) provide an overview of the surgical setting and explain the role of the radiographer as a vital member of the surgical team, (2) assist the radiographer in developing an understanding of the imaging equipment used in surgical situations, and (3) present common radiographic procedures performed in the OR. The radiographer should review the surgery department protocols because they vary from institution to institution. Sterile team members scrub their hands and arms, don a sterile gown and gloves over proper surgical attire, and enter the sterile field. The sterile field is the area of the OR that immediately surrounds and is specially prepared for the patient. To establish a sterile field, all items necessary for the surgical procedure are sterilized. After this process, the scrubbed and sterile team members function within this limited area and handle only sterile items (Fig. 29-1). The sterile team consists of the following members: • Surgeon: The surgeon is a licensed physician who is specially trained and qualified by knowledge and experience to perform surgical procedures. The surgeon’s responsibilities include preoperative diagnosis and care, selection and performance of the surgical procedure, and postoperative management of care. The surgeon assumes full responsibility for all medical acts of judgment and for the management of the surgical patient. • Surgical assistant: The first assistant is a qualified surgeon or resident in an accredited surgical educational program. The assistant should be capable of assuming responsibility for performing the procedure for the primary surgeon. Assistants help to maintain visibility of the surgical site, control bleeding, close wounds, and apply dressings. The assistant’s role varies depending on the institution and with the type of procedure or surgical specialty. • Physician assistant: The physician assistant is a nonphysician allied health practitioner who is qualified by academic and clinical training to perform designated procedures in the OR and in other areas of surgical patient care. • Scrub nurse: The scrub nurse is a registered nurse (RN) who is specially trained to work with surgeons and the medical team in the OR. • Certified surgical technologist (CST): The CST is responsible for maintaining the integrity, safety, and efficiency of the sterile field throughout the surgical procedure. The CST prepares and arranges instruments and supplies and assists the surgical procedure by providing the required sterile instruments and supplies. In some institutions, a licensed practical nurse (LPN) or RN may assume this role. • Anesthesia provider: The anesthesia provider is physician (anesthesiologist) or certified RN anesthetist who specializes in administering anesthetics. Choosing and applying appropriate agents and suitable techniques of administration, monitoring physiologic functions, maintaining fluid and electrolyte balance, and performing blood replacements are essential responsibilities of the anesthesia provider during the surgical procedure. • Circulator: The circulator is preferably an RN. The circulator monitors and coordinates all activities within the OR, provides supplies to the CST during the surgical procedure, and manages the care of the patient. • Radiographers: The radiographer’s role in the OR is to provide intraoperative imaging in a variety of examinations and with various types of equipment. • Others: The OR team may also include biomedical technicians, monitoring technologists, and individuals specialized in equipment or monitoring devices necessary during the surgical procedure. Street clothes should never be worn within semirestricted or restricted areas of the surgical suite (Fig. 29-2). Clean, fresh attire should be donned at the beginning of each shift in the OR suite and as needed if the attire becomes wet or grossly soiled. Soiled surgical attire should be changed to reduce the potential of cross-infection. Blood-stained or soiled attire including shoe covers is unattractive and can also be a source of cross-infection or contamination. Soiled attire is not worn outside of the OR suite, and steps should be taken to remove soiled clothing immediately on exiting. OR attire should not be hung in a locker for wearing a second time. Underclothing should be clean and totally covered by the scrub suit (Fig. 29-3). Other aspects of proper attire include the following: Fig. 29-2 OR suite layout showing restricted, nonrestricted, and semirestricted areas. ORs are “restricted.” • Protective eyewear: Occupational Safety and Health Administration (OSHA) regulations require eyewear to be worn when contamination from blood or body fluids is possible. • Masks: Masks should be worn at all times in the OR but are not necessary in all semirestricted areas. • Shoe covers: Shoe covers should be worn when contamination from blood or body fluids can be reasonably anticipated. Shoe covers should be changed whenever they become torn, soiled, or wet and should be removed before leaving the surgical area. • Caps: Caps should be worn to cover and contain hair at all times in the restricted and semirestricted areas of the OR suite. Hoods are also available to cover hair, such as facial hair, that cannot be contained by a cap and mask. • Gloves: Gloves should be worn when contact with blood or body substances is anticipated. • Radiation badge and identification: Radiation badge and proper identification should be worn at all times. Up to 10,000 microbial particles can be shed from the skin per minute. Nonsterile team members should not reach over a sterile field. When working over the sterile field (e.g., performing a posteroanterior [PA] lumbar spine), the sterile field should be covered with a sterile drape to protect the field (Fig. 29-4). The technologist cannot move the radiographic equipment into position over the sterile field until after the sterile cover is in place. A sterile team member should fold over the sterile drape on itself, and then a nonsterile team member should carefully remove the covering drape, being careful not to compromise the sterile field. If a sterile field is compromised, the OR staff should be notified immediately. Communication is of utmost importance. As a result of the surgical sterile field, the radiographer is unable to help position the image receptor (IR) or the patient. Good, professional communication is essential while using sound, basic knowledge of anatomy and positioning. The radiographer may have to instruct the surgeon or resident on the proper position to visualize the desired portion of the anatomy best. A surgeon or resident may be unaware of the exact rotation and foot flexion required to achieve a proper mortise view of the ankle. • Surgical technologist (CST) taking the IR: The CST holds a sterile IR cover open toward the radiographer. The radiographer should hold one end of the IR while placing the other end of the IR into the sterile IR cover. The CST grasps the IR and wraps the protective cover securely (Fig. 29-5). • Radiographer accepting the IR after exposure: After the exposure is made, the radiographer needs to retrieve the IR. The radiographer must be wearing gloves to accept a covered IR that has been in the sterile field or under an open incision. The protective cover is possibly contaminated with blood or body fluids and should be treated accordingly. The radiographer should grasp the IR, open the protective cover carefully away from himself or herself or others so as not to spread blood or body fluids, and then slide the IR out of the cover (Fig. 29-6). The radiographer should dispose of the IR cover in a proper receptacle and remember to remove gloves before handling the IR or any other equipment because the gloves are now considered contaminated. If contamination of the IR occurs, the radiographer should use hospital-approved disinfectant for cleaning before leaving the OR (Box 29-2). Some OR suites, such as those used for stereotactic or urologic cases, have dedicated radiologic equipment (Fig. 29-7). Most radiographic examinations in the OR are performed with mobile equipment, however. Mobile image machines are not as sophisticated as larger stationary machines in the radiology department. Mobile fluoroscopic units, often referred to as C-arms because of their shape (Fig. 29-8), are commonplace in the surgical suite. Mobile radiography is also widely used in the OR. Radiation protection for the radiographer, others in the immediate area, and the patient is of paramount importance when mobile fluoroscopic examinations are performed. The radiographer should wear a lead apron and stand as far away from the patient, x-ray tube, and useful beam as the procedure, OR, and exposure cable allow. The most effective means of radiation protection is distance. The recommended minimal distance is 6 ft (2 m). When possible, the radiographer should stand at a right angle (90 degrees) to the primary beam and the object being radiographed. The least amount of scatter radiation occurs at this position. The greatest amount of scatter radiation occurs on the tube side of the fluoroscopic machine. It is recommended that the x-ray tube always be placed under the patient (Fig. 29-9). Because of the significant amount of exposure to the facial and neck region, the x-ray tube should never be placed above the patient unless absolutely necessary. OPERATIVE (IMMEDIATE) CHOLANGIOGRAPHY Position of patient: The patient is supine with the abdomen exposed. In laparoscopic cases, such as cholecystectomy, the abdomen is distended because air is injected into the abdominal cavity to allow adequate room for maneuvering of the camera and instruments. The radiographer should ensure no obstacles would impede the movement of the C-arm (Fig. 29-10).
SURGICAL RADIOGRAPHY
Surgical Team
STERILE TEAM MEMBERS
NONSTERILE TEAM MEMBERS
Operating Room Attire
Dance of the Operating Room
PROPER IMAGE RECEPTOR HANDLING IN THE STERILE FIELD
Equipment
Radiation Exposure Considerations
Fluoroscopic Procedures for the Operating Room