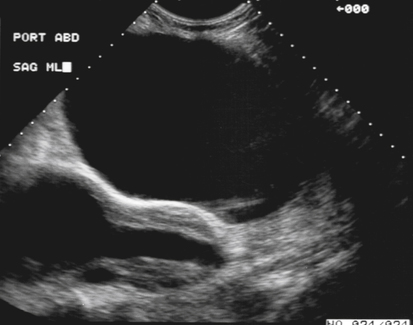
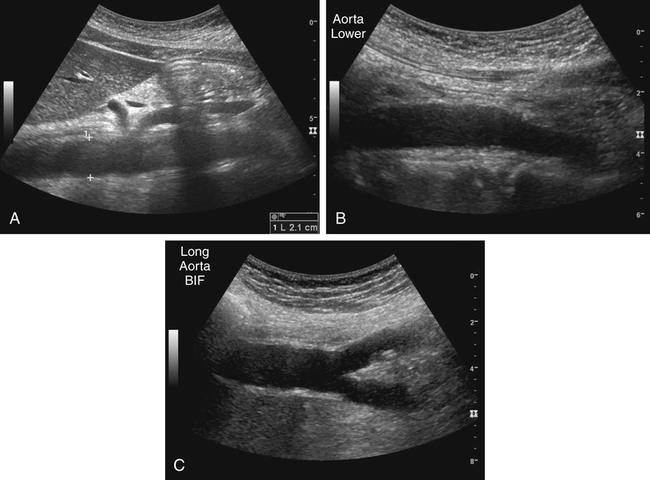
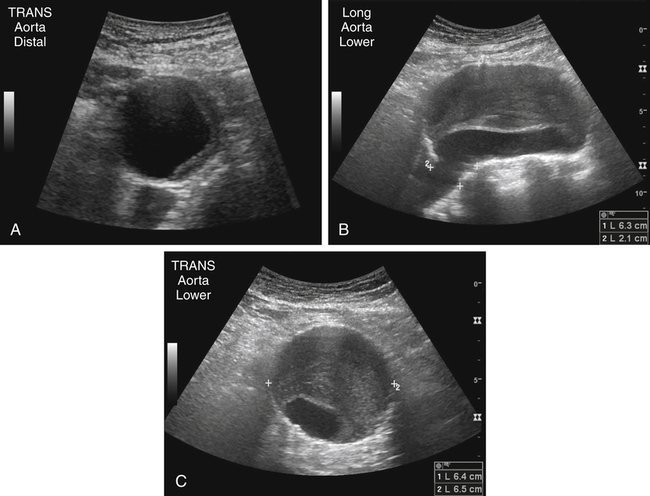
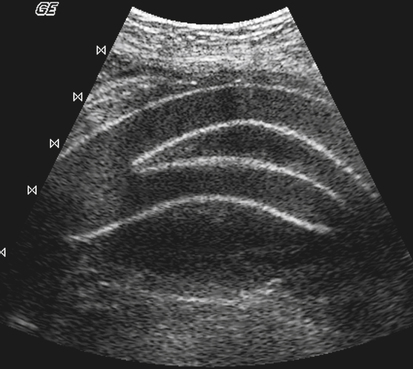
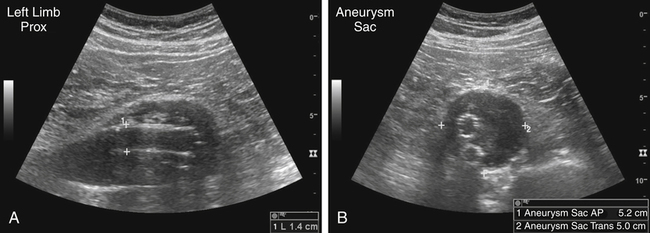
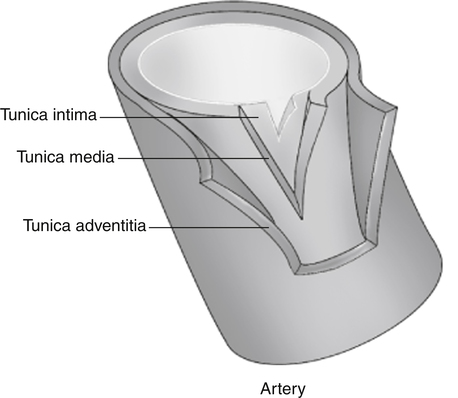
Kathryn Kuntz and John Lindsey • List the risk factors associated with abdominal aortic aneurysm, dissection, and rupture. • Describe the techniques for sonographic imaging of the abdominal aorta. • Identify the sonographic findings associated with abdominal aortic aneurysm, dissection, and rupture. • Describe the symptoms associated with abdominal aortic aneurysm, dissection, and rupture. • List the classifications used to characterize the various types of aortic dissections. • State the recommendations for aortic aneurysm surveillance and screening. Most abdominal aortic aneurysms (AAAs) are asymptomatic. They are typically not detected on physical examination and remain silent until discovered during radiologic testing for other reasons. Symptomatic aneurysms manifest with back, abdominal, buttock, groin, testicular, or leg pain and require urgent surgical attention. AAAs may be clinically silent, but the risk of rupture and the associated increased mortality rate show the importance of early detection and elective repair. Sonography is the preferred method of evaluation and screening.1 Sonographic examination of the abdominal aorta should include longitudinal and transverse images that show the proximal, middle, and distal segments (Fig. 10-2) and the iliac artery bifurcation. A normal aorta gradually tapers toward the distal segment (Fig. 10-2, B). The anteroposterior (AP) diameter should be measured in the longitudinal plane (Fig 10-2, A). The renal and iliac arteries (Fig. 10-2, C) should also be documented. The imaging challenge of overlying bowel gas can be diminished or alleviated with gentle transducer pressure and a patient preparation of an overnight fast. In addition, obese patients or patients with excessive bowel gas may benefit from various imaging techniques, including scanning the patient in a left posterior oblique or decubitus position. AAA is a common and potentially fatal condition that primarily affects older patients. Ruptured AAAs are a leading cause of death in the United States.1,2 The aortic wall comprises an inner layer, the tunica intima; a middle layer, the tunica media; and an outer layer, the tunica adventitia (Fig. 10-3). An aneurysm is a permanent focal dilation of an artery to 1.5 times its normal diameter. Normal infrarenal aortic diameters in patients older than 50 years are 1.5 cm in women and 1.7 cm in men. By convention, an infrarenal aorta 3 cm in diameter or larger is considered aneurysmal.3 AAAs develop as the tunica media, which is composed largely of smooth muscle cells, collagen, and elastin, thins. Tobacco use, hypertension, a family history of AAA, and male gender are clinical risk factors for the development of an aneurysm. AAA may be suspected when clinical examination reveals a pulsatile abdominal mass located at the level of the umbilicus or slightly cephalic to the umbilicus, although a large girth may limit the sensitivity of clinical palpation. In addition, AAA may be suspected when a tortuous calcified aorta is identified on a radiograph that may have been ordered for an unrelated condition or disease. Patients may have abdominal pain or back pain, which may indicate that the aneurysm is enlarging or, with severe symptoms, that rupture has occurred. Repair is indicated when the aneurysm becomes greater than 5.5 cm in diameter or grows more than 0.6 to 0.8 cm per year.1 Sonographic imaging of the aorta for detection of aneurysm is the preferred test because of the high sensitivity and specificity of this examination, although results may be limited by obesity, prior abdominal surgery, and overlying bowel gas. Sonography may be more effective when the patient has had nothing by mouth 8 hours before the examination. Sonographically, diagnosis of AAA can be made when the AP diameter is 3 cm or greater in the longitudinal plane. Aortic aneurysms may be fusiform (uniform dilation) or saccular (asymmetric saclike dilation) in appearance, or the aorta may have a gradual widening, referred to as aortic ectasia. Thrombus within the dilation may also be noted (Fig. 10-4) and most commonly appears as low-level echoes, although calcifications and liquefaction may also appear within thrombus. The absence of flow associated with thrombus in an aneurysm may be confirmed with color Doppler. Also, an important part of the protocol is documentation of the location of the aneurysm relative to the renal arteries—although in practice, the origins of superior mesenteric and celiac arteries are more commonly used to indicate the likelihood of infrarenal status (Fig. 10-2, A). The recommended sonographic surveillance is no further testing for patients with AAA less than 3 cm and annual sonography for AAAs measuring 3 to 4 cm. When an aneurysm reaches a diameter of 4 cm to 4.5 cm, screening should be performed every 6 months.1,4,5 Sonography is used in patient follow-up for assessment of an expanding aneurysm for planning of elective surgery. Patients with an aneurysm measuring greater than 4.5 cm should be referred to counseling for elective surgical options.1,4,5 If repair is undertaken, the walls of an aortic graft appear echogenic on sonogram (Fig. 10-5). The latest advance in the treatment of AAA is the placement of endoluminal grafts. These grafts are inserted into the aorta rather than exposing the aneurysm surgically. The advantage of the aortic endograft is that no abdominal incision is required, making recovery time considerably shorter than open resection. Most devices are configured as a metallic, self-expanding framework covered with various nonporous materials. (Fig. 10-6) The stents may be a straight tube or bifurcated. Blood flow is routed through the endograft depriving the aneurysm sac of blood. The technique of endovascular AAA exclusion (repair) is a safe and effective method for treating AAAs. Reports have shown a reduction in morbidity and decreased mortality. Despite reduction in overall complications, endoleak is a frequent occurrence after stent-graft deployment. The overall endoleak rate ranges from 7% to 47%, and it is estimated at 21% during the perioperative interval and up to 9% at 1 month after repair.7 The complication can be due to device failure during placement, changes over time, or failure to control blood flow within the aneurysm sac.7 An endoleak occurs when blood is allowed to flow into the aneurysm sac. Endoleaks are classified as one of four types, as follows:7–9 • Type 1: An attachment site leak, caused when the device is improperly sealed at the proximal or distal endpoint. • Type 2: Retrograde flow through collateral branches (i.e., lumbar branches or inferior mesenteric artery). • Type 3: Flow into the aneurysm secondary to an inadequate seal between components of the device or a tear in the fabric of the graft. • Type 4: Flow through the fabric of the graft secondary to graft porosity.
Suspect Abdominal Aortic Aneurysm
Abdominal Aorta
Normal Sonographic Anatomy
Abdominal Aortic Aneurysm
Sonographic Findings
Aortic Endografts
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine