Fig. 23.1
Syphilitic osteomyelitis complicated by metaphysitis and periostitis. (a) Posterior-anterior and lateral X-rays demonstrate worm-eaten-like bone destruction at the left superior tibia, with surrounding high-density area and neighboring periosteal thickening (indicated by arrow). (b) Linear transparent area of bone destruction is demonstrated at the metaphysis of left distal femur (indicated by arrowhead)
Case Study 3
A baby boy patient aged 2 days, with RPR of 1:128.
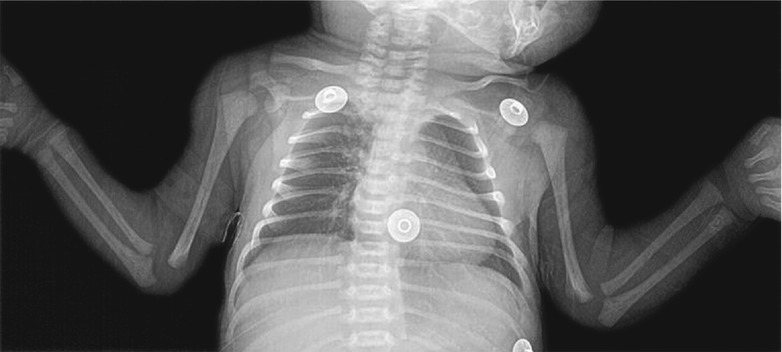
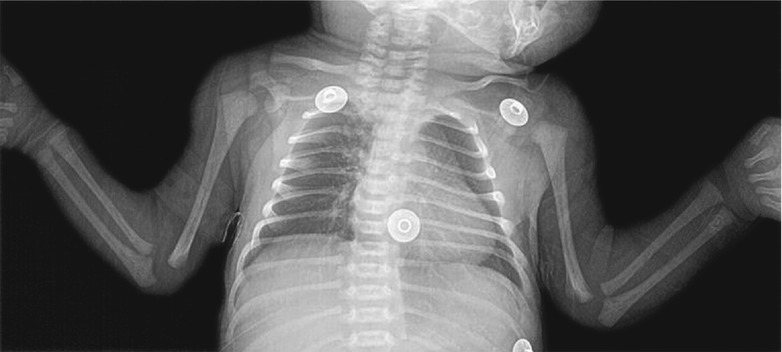
Fig. 23.2
Syphilitic metaphysitis. X-ray demonstrates round-like low-density bone lesion at the right inferior humerus
Case Study 4
A baby boy patient aged 2 months, with skin rashes for 1 month and fever and abdominal distension for 5 days.
Fig. 23.3
Syphilitic metaphysitis. (a, b) Posterior-anterior and lateral X-rays demonstrate bone destruction at the proximal metaphysis of left tibia, widened space between metaphysic and swollen adjacent soft tissue; (c, d) Posterior-anterior and lateral X-rays demonstrate coarse bone cortex at the metaphysis of right radius and ulna
(The case study 2 and the case study 3 as well as the figures are provided by Zhang N et al. from the Department of Radiology, Chengdu Infectious Diseases Hospital, Sichuan, China)
Case Study 5
A baby boy patient aged 5 months, with abnormalities by serological test for above 3 months.
For case detail and figures, please refer to from Zhang GY et al. Journal of Medical Research, 2012, 41(2): 166 (In Chinese).
Case Study 6
A baby boy patient aged 10 weeks, with pain at bilateral upper limbs. He was suspected with greenstick fracture of the left humerus.
Fig. 23.4
Syphilitic metaphysitis and periostitis. (a) X-ray demonstrates parallel thickening of periosteum at the right radius and ulna and transparency shadow below the metaphysis. (b) Thickened prior calcification is demonstrated at the left femur. (c) Irregular decalcification is demonstrated at the left proximal tibia (Reprint with permission from Marks KL. Br Med J, 1954, 1 (4869): 1018)
23.7.2 Neurosyphilis
The radiological examinations for the diagnosis of neurosyphilis mainly include CT scanning and MR imaging. X-ray and ultrasound provide information with limited diagnostic value.
23.7.2.1 Asymptomatic Neurosyphilis
The radiological examinations usually demonstrate no abnormalities of the brain parenchyma.
23.7.2.2 Meningeal Syphilis
In its early stage, CT scanning demonstrates no abnormalities. But by contrast scanning, linear enhancement of meninges sometimes can be demonstrated. By MR imaging, the meninges and brain surface are demonstrated with diffuse linear long or equal T1 signal and long T2 signal. The meningeal lesions are generally more serious at the base of brain, which can be demonstrated with obvious enhancement by contrast imaging (Fig. 23.5). There are also demonstrations of swollen adjacent brain tissues, enlarged and widened cisterns and sulci, and increased signal strength of cerebrospinal fluid. Due to accumulated and increased inflammatory exudates at the base of brain, communicating hydrocephalus commonly occurs. The meningeal lesions can disseminate along the cranial nerves at the base of brain to invade the cranial nerves, with common involvement of VII and VIII cranial nerves. Syphilitic myelitis is demonstrated as long T1 long T2 signals of the involved spinal cords. By contrast imaging, uneven enhancement can be demonstrated (Figs. 23.6 and 23.7). Due to common involvement of the meninges, the condition is also known as syphilitic meningomyelitis, manifested as inflammatory thickening of dura matter and its adhesion with pia matter of arachnoid membrane. The condition may further develop to cause lesions at the supplying vascular vessels and the nerve roots of the spinal cords, leading to spinal cord degeneration.
23.7.2.3 Meningovascular Syphilis
Meningovascular syphilis is pathologically characterized by proliferation of arteriolar endothelial cells and fibrocytes, thickening of vascular walls, stenosis, and blockage of the vascular lumen. After formation of cerebral infarction, MR imaging demonstrates typical T1WI low signal and T2WI high signal. By contrast imaging, the lesions are demonstrated with patches and cortical gyrus-like enhancement. After occurrence of encephalomalacia, the signal is the same as that of the cerebrospinal fluid.
23.7.2.4 Brain Parenchymal Syphilis
Brain parenchymal syphilis includes paralytic dementia and myelophthisis. In the early stage of brain parenchymal syphilis, CT scanning demonstrates extensive low-density change, with accompanying edema. In the advanced stage of brain parenchyma syphilis, the cortex is subject to diffuse atrophy and expanded lateral ventricles, but no ischemia and inflammatory changes. T1WI and T2WI of MR imaging demonstrate atrophy of different degrees at bilateral frontal and temporal lobes that is more obvious at the anterior parts, bilaterally symmetric dilation of brain ventricles, and glial proliferation of subcortex and hippocampus (Fig. 23.8).
23.7.2.5 Gumma Neurosyphilis
Gumma neurosyphilis can be found at any part of brain tissues, mostly at the cerebral cortex and subcortex. The round-like lesions may be singular or multiple, with a diameter of 2–2.5 cm. By T1WI, the central caseous necrosis of the lesion is demonstrated as low signal or equal low mixed signal, with surrounding low signal due to a large area of edema that shows space-occupying effect. By contrast imaging, the lesions are demonstrated with irregular ring-shaped enhancement and adjacent meningeal enhancement that indicates meningeal involvement Fig. 23.9. Intramedullary gumma neurosyphilis is manifested as swollen and thickened spinal cord, round-like or nodular lump that resembles to intracranial gumma, as well as enhancement and thickening of adjacent meninges.
Case Study 7
A male patient aged 53 years complained of dizziness with illusion for 1 month. He also experienced loss of memory, depression, and behavioral abnormalities. By laboratory tests, RPR was 1:8 and TPPA positive.
Fig. 23.5
Meningeal syphilis. (a, b) Transverse T2WI demonstrates multiple patches of long T1 long T2 signals at the bilateral semioval centrum and beside the bilateral lateral ventricles. By water and fat suppression T2WI, high signal can be observed. (c) The cortex at the inferior pole of bilateral temporal lobes and hippocampus is demonstrated to be thinner. (d, e) Contrast imaging demonstrates thickening and enhancement of the right temporal lobe and the meninges of brainstem; slight dilation of bilateral lateral ventricles
Case Study 8
A male patient aged 46 years experienced progressive instability of gait and dysuria. By physical examinations, deep reflex of both lower extremities was sensitive, bilateral Babinski sign was positive, and sensory disturbance was below L1. By laboratory tests, cell counts and protein level in the cerebrospinal fluid increased, while immunological assay of both cerebrospinal fluid and serum for syphilis was positive. The clinical diagnosis was syphilitic myelitis.
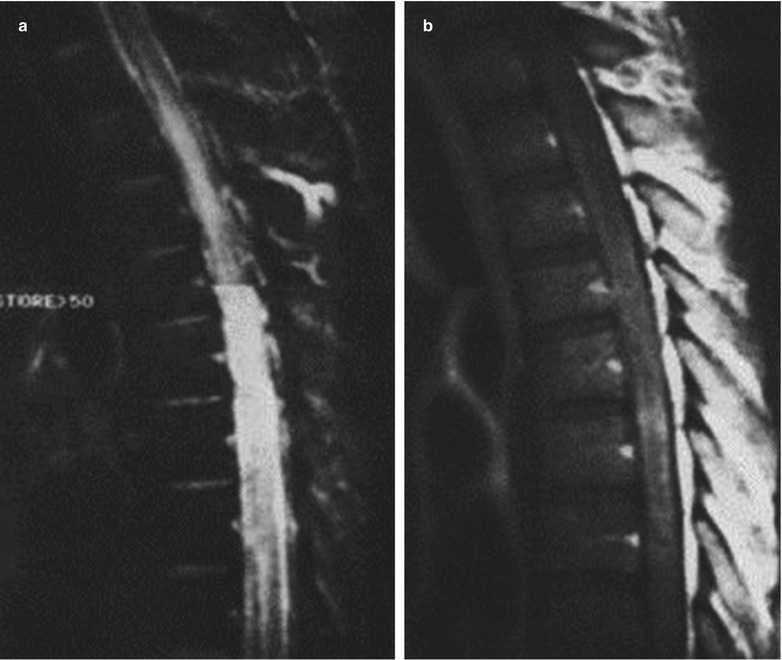
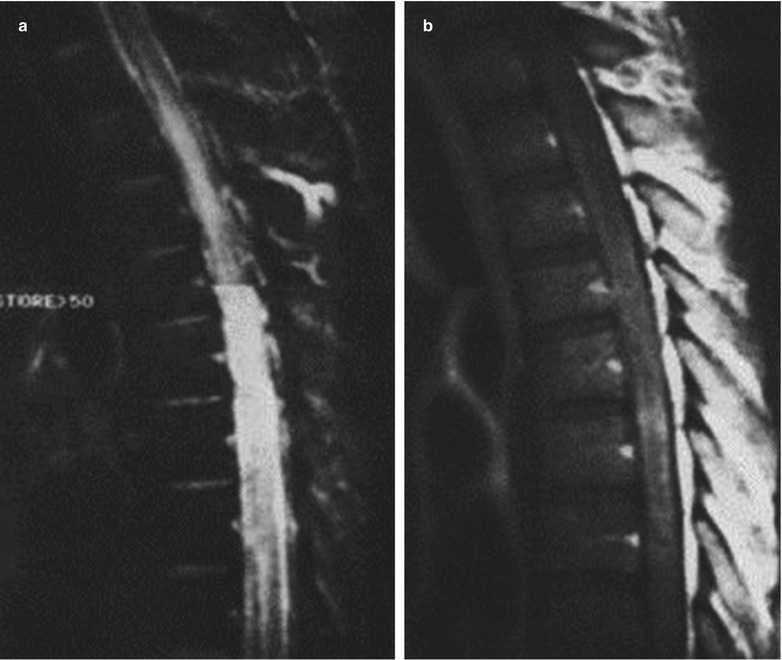
Fig. 23.6
Syphilitic myelitis. (a) Sagittal T2WI of MRI demonstrates high signal at the thoracic spinal cord. (b) Gd-DTPA contrast sagittal T1WI demonstrates uneven enhancement of the thoracic spinal cord, diffusive swelling of the spinal cord with internal low signal (Reprint with permission from H. Nabatame, et al. Neuroradiology, 1992, 34 (2): 105)
Case Study 9
A female patient aged 45 years complained of low back pain and upset with no known causes for 2 months that exacerbated for 2 weeks. The pain was especially obvious in the posture of supine at nights that affected her sleeping. In addition, she also experienced right lower-limb pain. By laboratory tests, RPR was positive, TPPA was positive, titer was 1:1,024, and HBV was positive. The pathological diagnosis was chronic inflammation with accompanying necrosis at T12-L1 spinal cord that is consistency with manifestations of syphilitic myelitis.
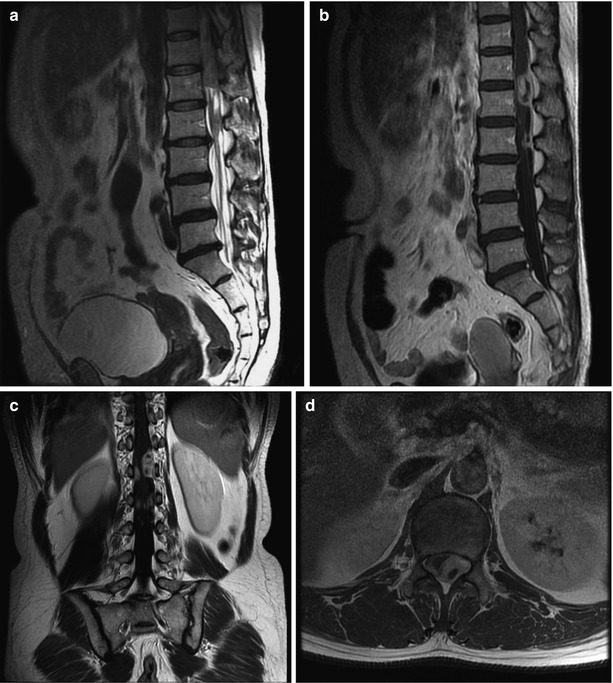
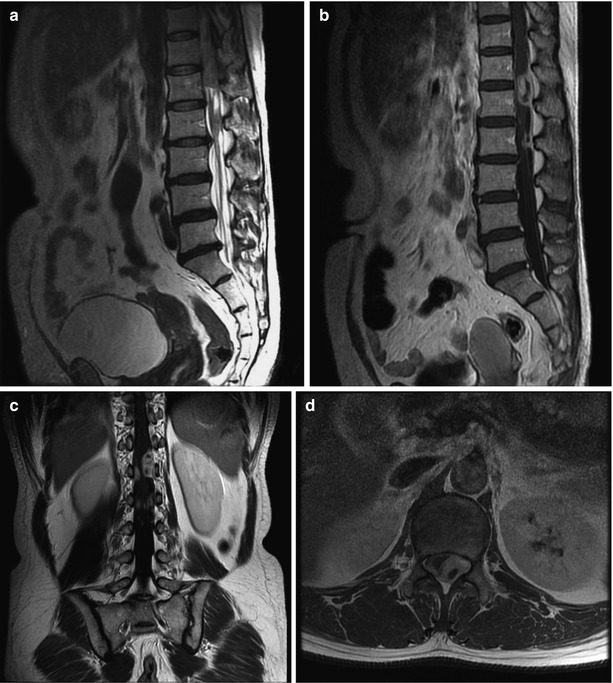
Fig. 23.7
Syphilitic myelitis. (a) T2WI demonstrates heterogeneous signal shadows at the T12-L1 spinal cords. (b–d) Contrast imaging demonstrates the posterior wall of T12-L1 horizontal spinal canal with multiple lumps of ring-shaped enhancement, which adhere to dura mater at the posterior wall of spinal canal. The adjacent dura mater is also demonstrated with enhancement
(The case and figures were provided by Tang YH at Ruijin Hospital, Shanghai, China)
Case Study 10
A male patient aged 49 years experienced unclear language expressions, loss of memory, emotional instability, tremor of upper limbs, poor orientation, uncoordinated gait, hypermyotonia of the four limbs, and tendon hyperreflexia. By laboratory tests, serological test for TP antigen was positive; VDRL of the cerebrospinal fluid was qualitatively positive and quantitatively 1:8. The clinical diagnosis was paralytic dementia.
For case detail and figures, please refer to Peng FH et al. Chinese Journal of Radiology, 2005, 39 (9): 957 (In Chinese).
Case Study 11
A male patient aged 44 years was detected syphilis positive more than 1 month ago. He had histories of unhealthy sexual life and drug abuse. And he experienced psychiatric disorder, loss of memory, and intelligence decline. By laboratory tests, TPPA was positive and RPR was 1:32.
Fig. 23.8
Brain parenchymal syphilis. Transverse T2WI demonstrates multiple spots and strips of long T1 long T2 signals at the bilateral basal ganglia. (b) Atrophy of bilateral hippocampus and parahippocampal gyri is demonstrated. (a, c) Dilation of the bilateral lateral ventricle and the third ventricle is demonstrated
Case Study 12
A female patient aged 40 years complained of blurry vision for 1 month, with defects of bilateral lower right vision.
Fig. 23.9
Gumma neurosyphilis. (a, b) Transverse MR imaging demonstrates round-like long T2 signal at the right mesencephalon and cerebral peduncle, with internal uneven and mixed signals. The center of the lesion is demonstrated with slightly low signal. And the lesion is demonstrated with surrounding large flakes of high-signal edema. And the midline structure is demonstrated to shift slightly leftward. (c–f) Contrast imaging demonstrates obvious enhancement of the lesion, with well-defined boundary, and slight enhancement of the adjacent meninges
(Note: the case and figures were provided by Xia S at the Department of Radiology, the First Central Hospital, Tianjin, China.)
Case Study 13
A male patient aged 56 years experienced IV degree myodynamia of the left lower limb and hyperalgesia of the left lower limb. He had a history of unhealthy sexual life. By laboratory tests, RPR was negative and TPPA was 1:640 to be positive.
For case detail and figures, please refer to Liu H et al. Journal of Clinical Radiology, 2008, 27 (9): 1275 (In Chinese).
23.7.3 Cardiovascular Syphilis
23.7.3.1 Syphilitic Aortitis
Syphilitic aortitis is commonly complicated by incomplete closure of aortic valve, stenosis of coronary orifice, and other conditions. Ultrasonocardiography demonstrates dilated aorta, aortic regurgitation, and enlarged left ventricle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree