Talcosis
Jud W. Gurney, MD, FACR
Key Facts
Imaging Findings
Inhalational
Diffuse fine-granular nodularity with high attenuation perihilar PMF
Aggregation of nodules into PMF (identical to silicosis)
International Labor Office “B” opacity type “p”
Pleural and diaphragmatic plaques identical to those from asbestos
Inhalational: Nodules in lymphatic distribution (centrilobular and subpleural)
Intravenous
Ground-glass opacities (probably due to nodules below resolution of scanner) usually exceeds profusion of nodules
PMF all zones
Basilar panlobular emphysema in intravenous Ritalin abusers
Intravenous: Nodules perivascular distribution (centrilobular) with occasional tree-in-bud opacity
Top Differential Diagnoses
Silicosis
Sarcoidosis
Metastatic Pulmonary Calcification
Cellulose Granulomatosis
Clinical Issues
Corticosteroids may stabilize PMF in intravenous talcosis
Slow progression even without further inhalational exposure
TERMINOLOGY
Abbreviations and Synonyms
Illicit drug use, simple pneumoconiosis, complicated pneumoconiosis, progressive massive fibrosis (PMF), IV drug abuser’s lung
Definitions
4 forms: 3 inhalational, 1 intravenous
Inhalation pure talc (talcosis)
Inhalation talc and silica (talco-silicosis)
Inhalation talc and asbestos (talco-asbestosis)
Intravenous illicit drug use
IMAGING FINDINGS
General Features
Best diagnostic clue
Diffuse fine-granular nodularity with high attenuation PMF
Basilar panlobular emphysema in intravenous abusers of methylphenidate (Ritalin)
Patient position/location
Inhalation: Nodules in upper lung zones
Progressive massive fibrosis in all zones
Intravenous: Nodules diffuse
Emphysema: Lower lobes
Progressive massive fibrosis perihilar
Size: Nodules pinpoint in size
Morphology: Ground-glass opacities usually greater in extent than definable nodules
CT Findings
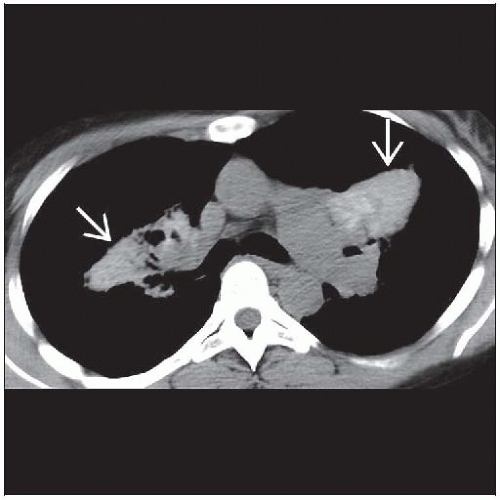
NECT: Progressive massive fibrosis typically of high attenuation, highly suggestive of talcosis
HRCT
Inhalational
Centrilobular and subpleural nodules, may calcify
International Labor Office “B” opacity type “p”
Aggregation of nodules into PMF (identical to silicosis)
Architectural distortion adjacent to PMF
PMF all zones
Pleural and diaphragmatic plaques identical to those from asbestos
Pleural thickening can sometimes be dramatic
Lymphadenopathy may be of higher attenuation
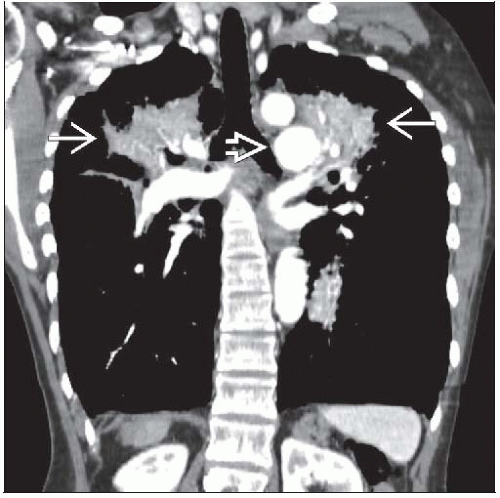
Intravenous
Centrilobular (fine granular appearance) nodules (< 1 mm diameter)
Ground-glass opacities (probably due to nodules below resolution of scanner) usually exceeds profusion of nodules
Nodules spare emphysematous lung, but otherwise uniform throughout lung
Emphysema may be upper lung zone or predominantly lower lung zone (even in absence of smoking)
Proclivity of Ritalin for severe lower lobe panacinar emphysema
Ritalin may result in severe lower lung zone panacinar emphysema alone without nodularity
PMF perihilar
Radiographic Findings
Radiography
Inhalational
Multiple tiny (pinpoint) miliary nodules
Predominantly upper lung zones
May evolve into progressive massive fibrosis
Lower zone reticular opacities and pleural changes in those with asbestos contamination
Enlarged hilar lymph nodes with eggshell calcification (especially in silico-talcosis)
Intravenous
Miliary “pinpoint” nodules
No zonal predilection
Occasionally lymphadenopathy
PMF in perihilar regions
Calcification in PMF usually not recognized on radiographs
Emphysema, either centriacinar (upper lung zones) or panacinar (lower lung zones)
Pulmonary artery hypertension in severe disease
Talc pleurodesis
Often used for pleurodesis due to intense inflammation induced by talc
Pleural thickened with irregular deposits of calcification in most dependent lung (dorsal) due to settling of talc in supine position
Imaging Recommendations
Best imaging tool: HRCT for characterization of interstitial lung disease and detection of high attenuation conglomerate masses
DIFFERENTIAL DIAGNOSIS
Sarcoidosis
No occupational exposure, PMF less likely
Nodules usually larger and tend to cluster (“galaxy” sign)
Peribronchovascular distribution of nodules
Metastatic Pulmonary Calcification
No progressive massive fibrosis
Emphysema if present admixed with ground-glass opacities or consolidation
Centrilobular nodules larger and mulberry shape and tend to cluster
Predominantly disease of upper lung zones
Silicosis
Occupational history
Nodules tend to be larger than talc
PMF usually more cephalad in upper lung zones and not high in attenuation
Talc and silica may be admixed together
Pleural plaques not seen
Cellulose Granulomatosis
Cellulose filler in oral medications
Cellulose particles trapped in arterioles leading to granulomatous reaction
HRCT: Centrilobular nodules and tree-in-bud pattern
No progressive massive fibrosis
Amyloidosis
Neurofibromatosis
Upper lobe bullae
Lower lobe reticular interstitial fibrosis
Cutaneous and skeletal stigmata of neurofibromatosis
Amiodarone Toxicity
Used to treat tachyarrhythmia
Accumulates in lung and liver
Focal areas of consolidation randomly distributed
Focal lung abnormalities and liver of high attenuation due to drug, which contains 3 iodine molecules
PATHOLOGY
General Features
General path comments
Talc: Magnesium silicate
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree