Embryology and Development of Temporal Bone
The ear consists of three major components, the external, middle, and internal ear. Embryologically the ear has a dual development with development of the inner ear structures (internal auditory canal [IAC], cochlea, vestibule, and semicircular canals [SCC]) independent of the middle and external ear structures (ossicles, middle ear air spaces, mastoid antrum, tympanic membrane [TM], external auditory canal [EAC], and temporomandibular joint [TMJ]). The neural sound-perceiving apparatus of the inner ear develops from a thickened ectodermal placode. The mechanical sound-collecting and sound-transmitting structures of the external and middle ear, respectively, develop from the first and second pharyngeal (branchial) arches and the intervening first pharyngeal cleft and pharyngeal pouch. Adjacent mesenchyme contributes to the development of the inner, middle, and external ear. This explains why developmental abnormalities of the inner ear are usually not seen with deformities of the external and middle ear, and vice versa.
The endolymphatic (membranous), perilymphatic (periotic), and bony labyrinths of the inner ear all develop from the ectodermal otic placode that invaginates to form the otocyst or otic vesicle. The otic vesicle elongates, forming a dorsal vestibular region and a ventral cochlear region. The endolymphatic duct also develops as a short projection from the dorsomedial surface of the otic vesicle. The perilymphatic labyrinth develops as mesenchyme surrounding the membranous labyrinth resorbs. The bony labyrinth (otic capsule) also develops from mesenchyme around the membranous labyrinth. This begins between 4 and 8 weeks’ gestation, continues to grow between 8 and 16 weeks’ gestation, and ossifies by week 24 of gestation.
The external and middle ear develop from the pharyngeal apparatus. The first pharyngeal groove deepens to become the primitive EAC and over time contributes to the development of the mature EAC, the outer layer of the TM, and the tympanic ring. The auricle or pinna develops around the first pharyngeal groove from six nodular mesenchymal masses or hillocks arising from the first and second pharyngeal arches. The first pharyngeal pouch expands to form a tubotympanic recess. This tubotympanic recess gives rise to the eustachian tube, the tympanic cavity, the mastoid antrum, and their epithelial lining. Just dorsal to the end of the tubotympanic recess, a condensation of mesenchyme from the first and second pharyngeal arches appears, which develops into the ossicles. The head and neck of the malleus and body and short process of the incus arise from the first arch. The second arch forms Reichert’s cartilage, from which the remainder of the malleus and incus and the stapes superstructure develop. The stapes footplate is a bilaminar structure, with an outer portion developing from Reichert’s cartilage and an inner portion developing from the ectodermal otocyst.
The middle ear cavity and mastoid antrum are fluid filled until birth. The neonate’s initial crying and breathing fill the eustachian tube system and the middle ear with air. The mastoid air cells develop as saclike extensions from the mastoid antrum, commencing around the time of birth and continuing for several years.
Normal Temporal Bone Anatomy
External Auditory Canal
The EAC consists of a funnel-shaped, undulating, cartilaginous lateral portion and an osseous medial segment ( Figs. 21-1 through 21-5 ; see Figs. 21-1B, 21-2C, 21-3A, 21-5A ). The cartilaginous portion is continuous with the auricle, flexible and surrounded by fat. The osseous portion, surrounded by the tympanic portion of the temporal bone, constitutes two thirds of the length of the EAC and is covered by skin and periosteum only. The EAC extends medially to the TM. The TM attaches to an annular ridge of bone termed the tympanic anulus.
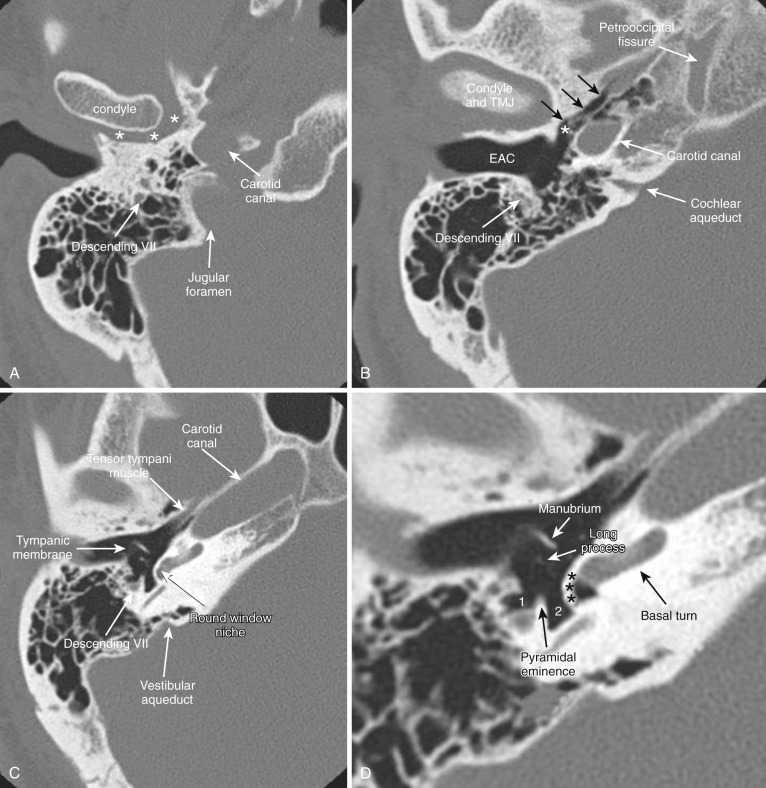






Middle Ear Cavity and Mastoid
The tympanic cavity, or middle ear, is the air space within the petrous portion of the temporal bone between the eustachian canal anteriorly and the mastoid air cells posteriorly that contains the ossicles (see Figs. 21-1D-G, 21-2C-F, 21-3B, 21-4D ). Its other borders consist of the TM laterally, otic capsule and cochlear promontory medially, tegmen tympani superiorly, and jugular floor inferiorly. The middle ear cavity can be subdivided into three spaces—hypotympanum, mesotympanum, and epitympanum—based on the relationship to the TM (see Fig. 21-2C ). The hypotympanum is the most inferior portion of the tympanic cavity, inferior to the level of the TM, and connects anteromedially to the opening of the eustachian tube. The semicanal for the tensor tympani muscle is parallel and superior to the eustachian tube (see Fig. 21-2A ). This muscle arises from the superior surface of the cartilaginous eustachian tube and courses posteriorly in the medial portion of the middle ear, turning sharply laterally at the level of the neck of the malleus, to which it attaches. The thin plate of bone separating these two semicanals is termed the cochleariform process (see Figs. 21-1F and 21-2B-C ).
The mesotympanum, the central portion of the tympanic cavity, is medial to the TM. It is bordered laterally by the scutum (or spur) and TM and medially by the otic capsule. The scutum is a bony crest separating the EAC from the epitympanic space (see Fig. 21-2C-D ). The TM attaches to the scutum superiorly and to the limbus inferiorly. The mesotympanum contains the majority of the ossicles.
The triangular epitympanum forms the superior portion of the middle ear, superior to the level of the TM. It contains the head of the malleus and the body and short process of the incus (see Fig. 21-1G ).
The posterior wall of the cavity is irregular and contains the facial nerve recess laterally and the sinus tympani medially, separated by the pyramidal eminence. The pyramidal eminence overlies the stapedius muscle, which inserts onto the head of the stapes (see Figs. 21-1D and 21-2G ).
Prussak’s space is another important area of the middle ear cavity bounded by the scutum and pars flaccid of the TM laterally, the neck of the malleus medially, and the lateral malleal ligament superiorly (see Fig. 21-2D ).
The cone-shaped antrum is located in the anterosuperior part of the mastoid portion of the temporal bone and communicates with the epitympanum via a narrow channel termed the aditus ad antrum. The antrum is surrounded by smaller variable-sized mastoid air cells (see Fig. 21-1K ). The size of the antrum varies considerably as a result of the alterations in pneumatization of the air cells that drain into it. The antrum is bordered superiorly by the tegmen tympani. The medial margin of the antrum is the promontory formed by the otic capsule of the lateral SCC. The mastoid air cells are divided by Koerner’s septum, a thin bony structure formed by the petrosquamous suture that extends posteriorly from the epitympanum, into medial and lateral components.
Ossicles
The ossicles are suspended by the TM, the ossicular ligaments to the epitympanic walls, and the oval window. The manubrium (or handle) and lateral process of the malleus attach to the TM. The neck of the malleus is connected to the tensor tympani tendon (see Fig. 21-2C ). The anterior malleal ligament attaches the head of the malleus to the anterior epitympanic wall; the superior malleal ligament attaches the head to the roof of the middle ear cavity. The lateral malleal ligament attaches the head or neck of the malleus to the tympanic notch, a defect in the superior portion of the tympanic anulus.
The circular head of the malleus articulates with the triangular body of the incus (see Figs. 21-1G and 21-3B ). The short process of the incus projects posteriorly and is suspended within the epitympanic space, pointing toward the aditus ad antrum. The posterior incudal ligament attaches the short process to the fossa incudis, a small depression in the posteroinferior part of the epitympanic recess. The long process of the incus projects inferiorly, parallel to and behind the manubrium of the malleus (see Fig. 21-2D ). The tip of the long process bends medially to end in the lenticular process, which articulates with the head of the stapes (see Fig. 21-2E ).
The stapes consists of the head, two crura, and a footplate (see Figs. 21-1E and F ). The footplate of the stapes attaches to the oval window of the vestibule and is secured by the annular ligament (see Fig. 21-2F ).
Inner Ear
The inner ear is located within the petrous portion of the temporal bone and comprises the osseous labyrinth, which consists of the cochlea, vestibule, and SCCs. The osseous labyrinth encapsulates the membranous labyrinth, which contains endolymph and is surrounded by perilymph.
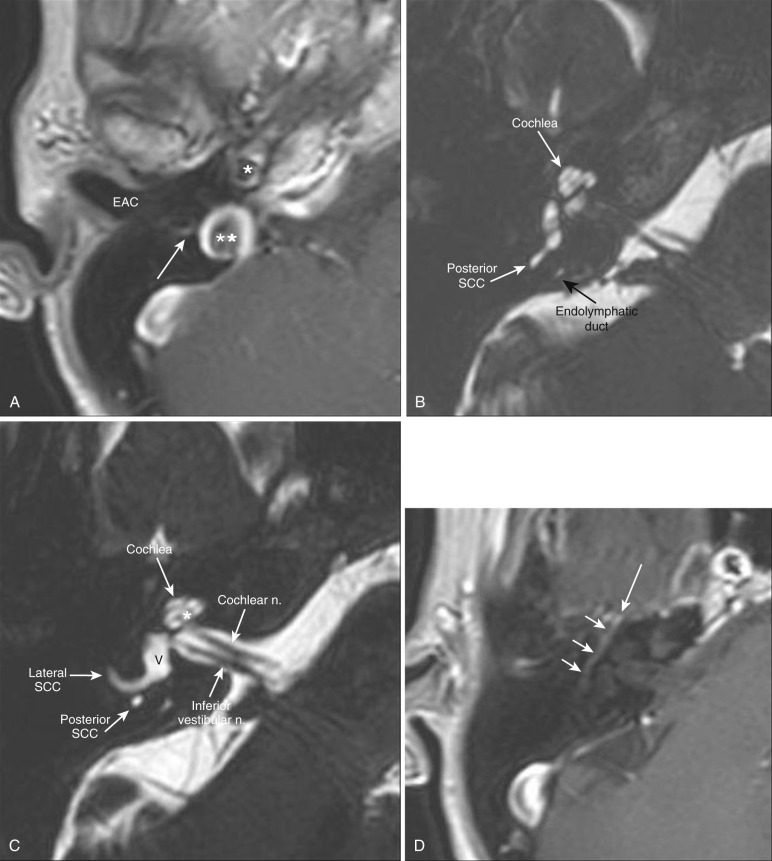
The vestibular cavity is the central portion of the membranous labyrinth that communicates with the SCCs and cochlea ( Fig. 21-6 ; see Figs. 21-1G, 21-1I, 21-2F, 21-3C, 21-5C, 21-6A ). The vestibule lies immediately lateral to the fundus of the IAC, and the oval window of the middle ear forms its lateral margin. The vestibular aqueduct is a narrow bony canal that contains the small endolymphatic duct and sac (see Figs. 21-1C, 21-3C, 21-5B ). The endolymphatic duct originates from the posteromedial aspect of the vestibule, courses past the common crus, and assumes a hockey-stick shape. The endolymphatic sac, an extension of the endolymphatic duct, is a dead-end fluid space arising from the vestibule that lies beneath the dura of the posterior temporal bone. The bony vestibular aqueduct surrounds the endolymphatic duct. The SCCs are three orthogonally arranged circular structures of the membranous labyrinth arising from the vestibule. The lateral SCC approximates the horizontal plane (see Fig. 21-1I ). The posterior and superior SCCs share a crus posteriorly, formed by a fusion of the posterior crus of the superior SCC and the anterior crus of the posterior SCC (see Figs. 21-1K, 21-2F, 21-3C, 21-4B ). The vestibule and SCCs are responsible for balance and equilibrium.

The oval window of the vestibule is the interface between the mechanical and neural elements of the ear (see Fig. 21-2F ). It lies just inferior to the horizontal facial nerve canal and the lateral SCC. It is covered by the annular ligament, which surrounds the footplate of the stapes.
The spiral cochlear apparatus contains the membranous labyrinth components for hearing. The cochlea lies anterior to the vestibule and has 2.5 to 2.75 turns (basal, middle, and apical) around its modiolus, the central bony spiral axis. The turns of the cochlea are separated by interscalar septae (see Figs. 21-1E and H, 21-2C, 21-4C, 21-5B and C ). The most lateral portion of the basal turn of the cochlea projects into the tympanic cavity, forming a promontory of bone (see Figs. 21-1D , 21-2E ). The round window is the bony opening of the basal turn of the cochlea into the middle ear, lying inferior and slightly posterior to the oval window and covered by a fibrous membrane (see Figs. 21-1C, 21-2G, 21-3C ). The cochlear nerve passes from the IAC through the bony canal for the cochlear nerve into the modiolus (see Figs. 21-1H , 21-5C ).
The cochlear aqueduct, a channel that connects the cochlea near the round window with the subarachnoid space just superior to the jugular tubercle, lies inferior to the IAC (see Fig. 21-1B ).
Internal Auditory Canal
The IAC is a bony conduit within the petrous portion of the temporal bone that transmits cranial nerves VII (facial) and VIII (vestibulocochlear) from the pontomedullary junction of the brainstem across the cerebellopontine angle (CPA) cistern to the inner ear ( Fig. 21-7 ; see Figs. 21-1G, 21-2F, 21-5C, 21-6A and B ). Its medial orifice is the porus acusticus. The IAC is partially divided by a transverse bony crest called the crista falciformis (see Fig. 21-2F ), which runs parallel to the long axis of the canal and divides it into a superior and inferior portion. A vertical crest termed Bill’s bar divides the superior component into anterior and posterior parts. The facial nerve is located in anterosuperior compartment, the cochlear nerve in the anteroinferior compartment, and the superior and inferior vestibular nerves in the posterosuperior and posteroinferior compartments, respectively (see Fig. 21-7 ). The lateral portion of the canal or fundus is perforated by the cranial nerves where they enter the cochlea, vestibule, and facial nerve canal (see Fig. 21-1H-J ). The IACs should be nearly symmetric. Although there is wide variation in the exact shape and size of the canals, asymmetry of greater than 2 mm suggests pathology.

Facial Nerve and Facial Nerve Canal
The facial nerve has a highly tortuous course and comes in close contact with almost every other important component of the temporal bone. It may be described as having six segments: cisternal, intracanalicular, labyrinthine, tympanic, mastoid, and extracranial. The facial nerve departs the brainstem at the lower border of the pons at the pontomedullary junction. Within the CPA cistern, the cisternal facial nerve is the most anterior and the vestibulocochlear nerve is the most posterior, with the nervus intermedius between the two. The facial nerve then enters the porus acusticus of the IAC and traverses the IAC in its intracanalicular segment (see Fig. 21-7 ). The labyrinthine portion of the facial nerve exits the superior anterior portion of the IAC fundus and follows an anterolaterally curving course in the fallopian canal to the geniculate ganglion. The greater superficial petrosal nerve also arises from the geniculate ganglion (see Figs. 21-1J, 21-2B and C, 21-5D ).
At the geniculate ganglion, an acute reverse (inverted V) angle of the nerve and canal is seen. The distal limb of the facial nerve doubles back posteriorly to become the tympanic segment in the medial wall of the tympanic cavity (see Figs. 21-1C, 21-2D-F, 21-5D ). This portion of the facial nerve canal has a thin inferior bony covering that may be dehiscent. The tympanic portion of the facial nerve runs horizontally directly inferior to the lateral SCC. The facial nerve then abruptly turns inferiorly (at an angle of 95 to 125 degrees) to form the posterior genu near the sinus tympani and the pyramidal eminence (see Fig. 21-3B ).
The vertical, or descending, facial nerve in the mastoid portion of the facial nerve canal runs vertically just posterior to the EAC. In this vertical portion, the nerve to the stapedius muscle and the chorda tympani (the first and second branches, respectively, of the facial nerve distal to the geniculate ganglion) arise (see Figs. 21-1A-C, 21-2H, 21-5A ). The facial nerve then exits the mastoid portion of the temporal bone via the funnel-shaped fat-filled stylomastoid foramen. The extracranial portion of the facial nerve delivers branches to the muscles and pierces the parotid gland to form the parotid plexus.
Carotid Canal
The carotid canal enters the base of the skull, ascends vertically, then turns horizontally and medially toward the petrous apex (see Figs. 21-1A-C, 21-2A and B, 21-3D, 21-5A ). This canal lies anterior and inferior to the cochlea and is separated from the middle ear cavity by a thin bony plate.
Jugular Foramen and Fossa
The jugular foramen is divided into a smaller anteromedial neural compartment (pars nervosa) containing cranial nerves IX, X, and XI, and a larger posterolateral vascular compartment (the pars vascularis) containing the jugular vein. The floor of the tympanic cavity normally forms the roof of the jugular fossa. The jugular bulbs are frequently asymmetric, and there may be a small diverticulum from their apices (see Figs. 21-1A, 21-2H, 21-3D, 21-5A ).
Temporal Bone Imaging Techniques
Computed tomography (CT) and magnetic resonance imaging (MRI) are currently the most widely used techniques for imaging the temporal bone, having largely replaced the former modalities. CT and MRI studies are complementary. Each technique has advantages and disadvantages, and often more than one examination is necessary for a complete temporal bone evaluation. CT is excellent for assessing the osseous structures of the temporal bone but not ideal for evaluating the soft tissue contents of the otic capsule, brain, or vessels. In contrast, MRI is superior to CT in characterizing the cerebrospinal fluid (CSF), brain, and cranial nerves. CT and MR angiography can be used to assess vascular structures.
Computed Tomography
The temporal bone has a high inherent contrast resolution, having both the densest bone in the body and air-filled spaces. High-spatial-resolution CT scanning is the best method for evaluating bone and air space anatomy and disorders. A major advance in CT technology was achieved with the introduction of multidetector-row helical CT. Compared to earlier CT techniques, multidetector CT provides improved quality of the axial source images as well as two- and three-dimensional (2D and 3D) reconstructions; this is due to a reduction in partial volume and motion artifacts and higher resolution along the z-axis with nearly isotropic voxel size. Multiplanar CT reformations can display the complex anatomy of the temporal bone in all planes while exposing the patient to radiation only once.
High-resolution CT images are usually acquired with thin sections (0.5-1 mm) and special bone algorithms for high detail. At the authors’ institution, scans are acquired in the axial plane in the helical mode with a slice thickness of 0.625 mm. The image data set is reconstructed into magnified axial, sagittal, and coronal images with 0.625-mm thickness at an interval of 0.312 mm. Contrast enhancement is not essential for evaluation of pathology isolated to bone or air spaces. For some clinical indications, additional reconstructed images are obtained in the planes of Stenvers and Pöschl (see Fig. 21-4A-F ). Stenvers’ plane is perpendicular to the superior SCC. Pöschl’s plane is parallel to the superior SCC. Oblique reformatted images can be obtained in virtually any other plane to highlight specific structures of the temporal bone.
The high contrast between the bony structures and the air spaces allows for virtual endoscopy of the middle ear by using surface-rendering technique. Axial images and 2D reformatted images remain the main modality for evaluating temporal bone structures and pathology. 3D reformatted virtual endoscopy (VE) images may serve as an adjunct in assessing the temporal bone, particularly in assessing the ossicular chain and possibly the round window; however, the overall sensitivity and specificity of this technique for detecting middle ear abnormalities is 59% and 25%, respectively. VE images may be of additional benefit to surgeons because they are more similar to their visual view in the operating room. VE images may also be helpful in teaching and in ear surgery simulators.
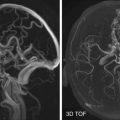
Magnetic Resonance Imaging
MRI also has revolutionized the temporal bone examination and expanded the range of pathology that can be accurately evaluated, because it can image many soft tissue entities. It is much better than CT in characterizing the CSF, brain, and cranial nerves, and it can be useful in the evaluation of blood vessel–related disorders of the temporal bone.
Many different techniques can be used to acquire MRIs, depending on the suspected abnormality and the equipment available. T2-weighted (repetition time [TR] = 3000 milliseconds or longer; echo time [TE] = 80 milliseconds or longer) axial spin echo images display the CSF and endolymphatic spaces and many disease processes as high-signal-intensity regions. Submillimeter images can be obtained using a 3D turbo-spin echo (TSE)/fast-spin echo (FSE) sequences. These sequences display the otic capsule structures as high-signal-intensity regions surrounded by signal void. The facial nerve and the three branches of the vestibulocochlear nerve can be distinguished inside the IAC. This type of sequence is often used as a screening technique for vestibular schwannomas.
T1-weighted (TR = 600 milliseconds, TE = 20 milliseconds) spin echo coronal or axial images are often acquired before and after administration of gadolinium-based contrast agent. The fat spaces have high signal intensity, and the brain has intermediate signal intensity. CSF demonstrates low signal intensity, and air and bone spaces appear as voids. Postcontrast T1-weighted images are particularly sensitive for evaluating abnormalities that alter the blood-brain barrier or are vascular. The sensitivity of contrast-enhanced T1-weighted images to detect these lesions can be exaggerated by using fat-saturation techniques.
Normal Temporal Bone Images
Axial Images: Caudal to Cranial
Axial jugular foramen level (see Figs. 21-1A , 21-5A ).
CT: The carotid canal lies just anterior to the jugular fossa, forming a “snowman”-like configuration. Both demonstrate sharp cortical margins. Inferiorly only a small spine, the caroticojugular spine, separates the two as they converge to enter the carotid sheath. The descending facial nerve canal is lateral to the jugular foramen, seen as a rounded well-corticated lucency. The mandibular condyle and TMJ can also be seen.
MRI: The descending portion of the facial nerve can be seen just lateral to the jugular bulb on T1- and T2-weighted images as an intermediate- to high-signal rounded structure. The blood vessels generally demonstrate signal void due to flow but may be seen as areas of intermediate to high signal if slow or turbulent flow is present.
Axial inferior tympanic level (see Fig. 21-1B ).
CT: The opening of the eustachian canal is triangular, with the apex extending parallel to the carotid canal and communicating with the anterior hypotympanum. The anterior and posterior walls of the bony EAC demonstrate dense, sharp cortical margins without soft tissue covering. The anterior margin of the EAC forms the posterior lip of the TMJ. The medial funnel-shaped opening of the cochlear aqueduct can be seen as a triangular lucency facing the CPA, progressively enlarging from lateral to medial. The opening of the aqueduct may be large and mimic the IAC. The descending facial nerve canal is easily identified posterior to the EAC. The petrooccipital fissure separates the temporal bone from the occiput.
MRI: The facial nerve is seen as an intermediate- to high-signal-intensity circular structure surrounded by a large area of signal void of the temporal bone and mastoid air spaces. The cochlear aqueduct is not well seen on MRI studies, possibly because of the combination of its small diameter and CSF motion artifacts.
Axial midtympanic level (see Figs. 21-1C-E, 21-5B ).
CT: The carotid canal can be seen early in its anteromedial course through the skull base, parallel and medial to the semicanal of the tensor tympani muscle at this level. The normally thin TM may be visible. The manubrium of the malleus parallels the TM. The manubrium of the malleus lies parallel and anterior to the long process of the incus. The stapedial superstructure (head, crura, and tympanic portion of the footplate) is often seen, forming an arch over the oval window. The cochlear promontory can be seen along the complex medial wall of the middle ear. Along the posterior wall of the middle ear is the pyramidal eminence, with the facial nerve recess lateral and the sinus tympani medial to the eminence. The descending facial nerve canal can be seen just posterior to the pyramidal eminence. The apical, middle, and basal cochlear turns are seen at this level along with the round window niche at the basal turn. The vestibular aqueduct is seen as a thin bony lucency along the posterior margin of the temporal bone, near its opening to the posterior cranial fossa.
MRI: The cochlea is seen as a high-signal-intensity structure on T2-weighted images. The endolymphatic duct and sac may be seen as a tubular, thin, high-signal-intensity structure along the posterior margin of the temporal bone. The middle ear and its contents are not well seen unless filled with fluid.
Axial epitympanic–internal auditory canal level (see Figs. 21-1F-J, 21-5C and D ).
CT: The crura of the stapes can be seen extending toward the oval window, and the tensor tympani tendon can be seen making a 90-degree turn and attaching to the neck of the malleus. At the level of the incudomalleolar articulation, the round head of the malleus and the triangular body and short process of the incus are seen in their characteristic “ice cream cone” configuration. The lateral SCC is seen protruding into the middle ear. The modiolus and interscalar septae of the cochlea are visualized, as is the vestibule, posterolateral to the cochlea. The IAC is slightly funnel-shaped and ends in an ovoid fundus. The canals for the facial nerve, cochlear nerve, superior vestibular nerve, and inferior vestibular nerve (singular canal) can be seen leaving the fundus of the IAC. The labyrinthine segment of the facial nerve canal (fallopian canal) can be seen extending to the anterior genu, and the tympanic segment is seen coursing along the medial wall of the tympanic cavity.
MRI: MRI studies demonstrate CSF in the IAC, and with high-resolution images the individual nerves are seen as low-signal filling defects within the CSF. The fluid contents of the cochlea, vestibule, and SCCs are seen as high signal on T2-weighted images. The modiolus and interscalar septae are seen as areas of low signal within the otherwise bright cochlea. The geniculate ganglion and horizontal segment of the facial nerve are seen as intermediate-signal-intensity structures surrounded by the signal void resulting from their bony walls on T1-weighted images.
Axial mastoid antrum level (see Fig. 21-1K and L ).
CT: The aditus ad antrum is situated between the epitympanum and mastoid antrum. The mastoid antrum lies posterior and lateral to the aditus ad antrum and opens into many mastoid air cells. On CT scans, the posterior SCC and common crus of the posterior and superior SCCs can be seen. More superiorly the superior SCC is present.
MR: Portions of the SCCs are seen as areas of high signal on T2-weighted images.
Coronal Images: Anterior to Posterior
Coronal temporomandibular joint level (see Fig. 21-2A ).
CT: The horizontal carotid canal is seen as an oval structure just lateral to petrooccipital suture. The semicanal for the tensor tympani muscle is seen as a small lucency lateral to the carotid canal. The air-filled eustachian tube is inferior to the tensor tympani, and the TMJ is seen laterally.
Coronal geniculate ganglion level (see Fig. 21-2B ).
CT: The tensor tympani muscle is seen along the medial wall of the middle ear, with the cochleariform process separating it from the eustachian tube below. The anteriormost part of the cochlea is medial to the tensor tympani. The geniculate ganglion is seen as a small lucency superior to the cochlea.
MRI: The geniculate ganglion is seen as a punctate focus of intermediate signal on T1-weighted images.
Coronal anterior tympanic level (see Fig. 21-2C ).
CT: The superior and inferior walls of the EAC are seen well. The TM may be identified as a thin filamentous structure extending from the scutum superiorly and coursing parallel to the plane of the long process of the malleus to attach to the limbus inferiorly. The head and neck of the malleus can be seen in the epitympanic space, with the tendon of the tensor tympani muscle attaching to neck. The basal and second turn of the cochlea are visualized. The labyrinthine and tympanic segments of the facial nerve are seen as two lucencies superior to the cochlea. The floor and roof (tegmen) of the middle ear are well visualized.
MRI: The cochlea is of high signal on T2-weighted images.
Coronal midtympanic level (see Fig. 21-2D and E ).
CT: This level shows the long process and lenticular process of the incus and the incudostapedial articulation as an L-shaped configuration. The stapes projects medially and superiorly from the lenticular process of the incus toward the oval window, located above the cochlear promontory. Prussak’s space is seen between the incus and scutum. The tympanic segment of the facial nerve canal is seen along the medial wall of the middle ear just superior and lateral to the cochlea.
Coronal oval window level (see Figs. 21-2F, 21-6A and B ).
CT: The full extent of the IAC is well visualized at this level, with the central crista falciformis dividing the canal into two portions. On CT scans, the oval window is seen as a bony defect in the lateral portion of the vestibule. The stapes is oriented slightly superiorly toward the oval window, just inferior to the lateral SCC. Also, beneath the lateral SCC, the horizontal portion of the facial nerve canal appears as a small circular structure. The anterior limb of the superior SCC can be seen. The epitympanic space lies just lateral to the lateral SCC. The floor and roof (tegmen) of the middle ear are well visualized on CT scans.
MRI: On T2-weighted images the facial and vestibulocochlear nerves can be seen as linear low-signal-intensity structures surrounded by the high-signal fluid in the IAC. The inner ear structures are of high signal on T2-weighted images. On T1-weighted images the IAC and its contents are of intermediate signal.
Coronal posterior tympanic level (see Fig. 21-2G ).
CT: The vestibule and round window niche are seen at this level. The sinus tympani—which extends between the labyrinthine wall and the pyramidal eminence—is seen, as is the facial nerve recess, which is lateral to the pyramidal eminence.
Coronal jugular foramen level (see Fig. 21-2H ).
CT: The jugular foramen frequently has a dome-shaped outline. The mastoid segment of the facial nerve canal can be identified lateral to the jugular foramen, running nearly vertical and extending toward the stylomastoid foramen. The mastoid antrum is seen superiorly and laterally. Portions of the lateral and superior SCCs can be seen.
MRI: Variable signal can be seen in the jugular bulb within the jugular foramen, depending on the sequence, flow, and presence of contrast. The mastoid segment of the facial nerve is seen as a linear intermediate signal structure lateral to the jugular bulb.
Sagittal Images: Lateral to Medial
Sagittal external auditory canal level (see Fig. 21-3A ).
CT: The EAC is seen in cross section just posterior to the TMJ. The relationship of the mandibular condyle to the glenoid fossa and EAC is well visualized.
Sagittal descending facial nerve canal level (see Fig. 21-3B ).
CT: The descending facial nerve and posterior genu form an upside-down hockey-stick shape. The head and manubrium of the malleus and the body and long process of the incus can be seen in a “molar tooth” configuration. The lateralmost part of the lateral SCC is visualized.
Sagittal vestibule level (see Fig. 21-3C ).
CT: The vestibule is seen as a central lucency. The common crus of the superior and posterior SCCs can be seen just posterior and superior to the vestibule. The round window is visualized, with the basal turn of the cochlea just anterior to the round window. The vestibular aqueduct appears as a thin linear structure underlying a flange of the posterior petrous bone.
MRI: The vestibule and portions of the cochlea and SCCs are seen as areas of high signal on T2-weighted images. The contained endolymphatic duct and sac are seen as areas of high signal underlying a flange of the petrous bone.
Sagittal internal auditory canal level (see Figs. 21-3D , 21-7 ).
CT: The IAC is seen in cross section as an oval lucency. A portion of the cochlea can be seen anterior to the IAC. The carotid canal is anterior and the jugular fossa inferior to the otic capsule structures.
MRI: MRI studies can demonstrate the individual nerves in the IAC, with the facial nerve superior and anterior, the cochlear nerve inferior and anterior, and the vestibular nerves posterior.
Stenvers’ and Pöschl’s Views
Stenvers’ view (see Fig. 21-4A-D ).
This plane is perpendicular to that of the superior SCC, which is seen in cross section, and parallel to that of the posterior SCC, which is well seen, as is the common crus. The turns of the cochlea are well seen on this view, as are the round window, descending facial nerve canal, and incudomalleolar joint. This view is perpendicular to the labyrinthine segment and parallels the tympanic segment of the facial nerve canal. It is also parallel to the tensor tympani muscle.
Pöschl’s view (see Fig. 21-4E and F ).
This plane is parallel to the plane of the superior SCC, which can be seen throughout its course appearing as a ring, and the bone separating it from the middle cranial fossa is clearly defined. This plane is perpendicular to the posterior SCC. This plane is also perpendicular to the tympanic segment of the facial nerve canal, which is seen in cross section on this view. This plane is parallel to the plane of the axis (modiolus) of the cochlea and the labyrinthine segment of the facial nerve canal.
Abnormal Temporal Bone
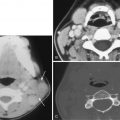
Middle Ear and External Ear Malformations
Congenital aural atresia is failure of development of the EAC. It is often associated with abnormalities of the auricle (microtia), ossicles, and middle ear. The inner ear is usually normal. The external ear, EAC, size of middle ear, ossicles, mastoid air cells, oval window, round window, and facial nerve course can potentially be dysplastic or absent and must be assessed along with possible presence of a cholesteatoma. EAC atresia can be complete or stenotic. The EAC is considered narrowed if its diameter is less than 4 mm. Canal stenosis may be from a web or band of soft tissue, a bony plate at the level of the TM, or both.
Many ossicular anomalies can occur with EAC maldevelopment. The ossicles may be fused, rotated, hypoplastic, or absent. The most common anomaly is fusion of the malleus and incus. The fused ossicles may also be fused to the atretic plate, usually at the region of the neck of malleus.
The facial nerve canal must be carefully evaluated in all cases of suspected external and middle ear anomalies. Anomalous development of the middle ear and temporal bone may alter the course of the facial nerve, with the tympanic and mastoid segments most commonly affected. The tympanic segment is usually displaced inferiorly as low as the round window and may be medially displaced and cross the oval window. The mastoid segment is displaced anterolaterally and may exit the temporal bone at the level of the round window or into the TMJ ( Fig. 21-8 ). Various grading systems and classifications have been developed for EAC atresia.