4 Temporal Bone Vascular Anatomy, Anomalies, and Disease, with an Emphasis on Pulsatile Tinnitus
The temporal bone is the bony framework within which a complex array of anatomic relationships exists. These anatomic relationships involve important vascular structures, including the sigmoid sinus, internal jugular bulb/vein, and petrous segment of the internal carotid artery (ICA) and the closely associated nervous structures. In this chapter, we will focus on the normal vascular anatomy of the temporal bone, including normal variants and congenital vascular anomalies, as well as acquired vascular lesions related to the temporal bone. Essential to the discussion of vascular lesions are those related to pulsatile tinnitus (PT) and vascular tympanic membranes (TMs); we will conclude with a comprehensive review of these topics.
Normal Vascular Anatomy
Knowledge of the normal appearance of the major venous, arterial, and neural structures within and adjacent to the temporal bone is critical to the correct identification of normal vascular asymmetry, vascular variants, and pathological vascular conditions.
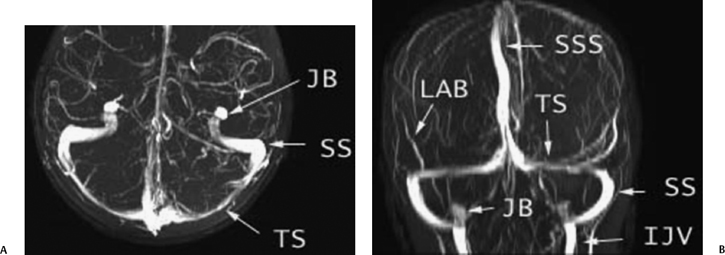
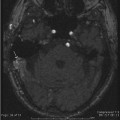
Fig. 4.1 Normal venous anatomy: magnetic resonance venography (MRV). (A) Axial MRV maximal intensity projection (MIP) image (TS, transverse sinus; SS, sigmoid sinus; JB, jugular bulb). (B) Coronal MRV MIP image (SSS, superior sagittal sinus; LAB, vein of Labbé; IJV, internal jugular vein).
Normal Venous Anatomy
The sigmoid sinus and jugular bulb/vein are the major venous structures intimately associated with the temporal bone (Fig. 4.1 to Fig. 4.10). The sigmoid sinus is the most distal dural venous sinus and serves to connect the transverse sinus to the internal jugular vein at the level of the jugular bulb (Fig. 4.1A). At its junction with the transverse sinus, the sigmoid sinus drains the vein of Labbé (Fig. 4.1B) and, slightly more distally, the superior petrosal sinus.1 From here, the sigmoid sinus courses inferiorly and medially in a gentle S-shaped curve, carving out the sigmoid sulcus along the intracranial surface of the mastoid portion of the temporal bone (Fig. 4.5 and Fig. 4.6).1,2 As the sigmoid sinus passes in the sigmoid sulcus along the medial border of the mastoid air cells, it defines a bony interface described as the sigmoid plate (Fig. 4.6). The sigmoid sinus then proceeds anteromedially to become continuous with the jugular bulb situated within the bony jugular foramen. The sigmoid sinuses may be symmetric or very asymmetric in size, such that the absence of one sinus can represent a normal anatomic variant and not a pathologic process (Fig. 4.11).
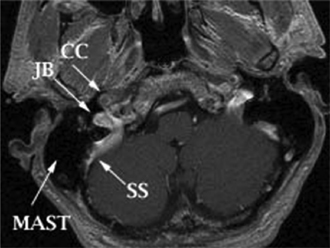
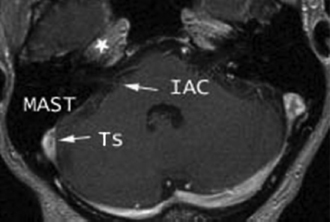
Fig. 4.3 Normal anatomy: axial postgadolinium T1-weighted magnetic resonance image. The horizontal segment of the petrous internal carotid artery (*) is at/above the level of the cochlea (IAC, internal auditory canal; TS, transverse sinus; MAST, mastoid air cells).
The jugular bulb represents the prominent cephalad dilation of the internal jugular vein in the roof of the jugular foramen (Fig. 4.1, Fig. 4.2, and Fig. 4.4). In the coronal plane, the jugular bulb is seen lying immediately beneath the vestibule in the posterior hypotympanum (Fig. 4.9).3,4
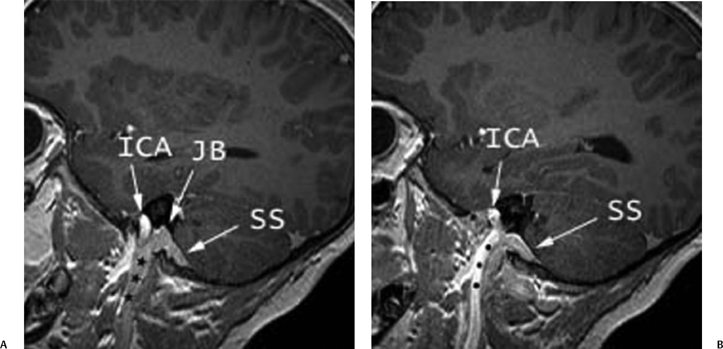
Fig. 4.4 Normal anatomy: sagittal magnetic resonance image. (A) Sagittal postgadolinium T1-weighted multiplanar reformatting (MPR) image demonstrates the normal course of the internal jugular vein (*) to its most cephalad point, the jugular bulb (JB), which drains the sigmoid sinus (SS). (B) Anterior to the internal jugular vein (*) is the internal carotid artery (ICA).
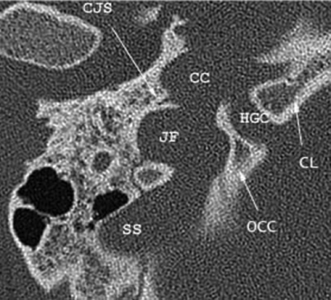

Fig. 4.6 Normal anatomy: unenhanced axial computed tomography (CT) image. At a slightly higher level, the jugular foramen is separated into the pars nervosa (PN) anteriorly and the pars vascularis (PV) posterolaterally by the jugular spine (JS) and, more commonly, a fibrous septum, not visualized on imaging. The horizontal segment of the internal carotid canal within the horizontal carotid canal (not shown) courses toward the foramen lacerum (FL) and forms part of its roof. The inferior petrosal sinus drains the cavernous sinus and travels within the petrooccipital fissure (*), then within the pars nervosa before draining into the internal jugular vein. Well depicted in this image is the course of the sigmoid sinus as it carves out the sigmoid sulcus (SS) along the medial border of the mastoid temporal bone. The sigmoid plate (SP) defines the bony border between the sigmoid sinus and the mastoid air cells. The course of the eustachian tube (ET) parallels that of the horizontal carotid canal and the horizontal segment of the facial nerve but is located more inferiorly. The vascular structures of the temporal bone are intimately associated with other important structures, including the vidian canal (VC), foramen ovale (FO) containing the mandibular segment of CN V (V3), and the foramen spinosum (FS) containing the middle meningeal artery. The descending segment of the facial nerve (DFN) travels within the mastoid temporal bone before exiting through the stylomastoid foramen.
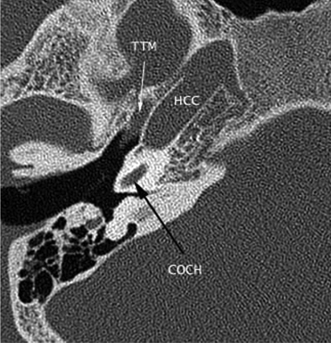
Fig. 4.7 Normal anatomy: unenhanced axial computed tomography (CT) image. The petrous internal carotid artery ascends vertically through the petrous temporal bone to the level of the cochlea (COCH), where it makes a sharp bend (posterior genu of the internal carotid artery) to course anteromedially in the horizontal carotid canal (HCC), ending just cephalad to the foramen lacerum. The tensor tympani muscle (TTM) parallels the course of the horizontal carotid canal.
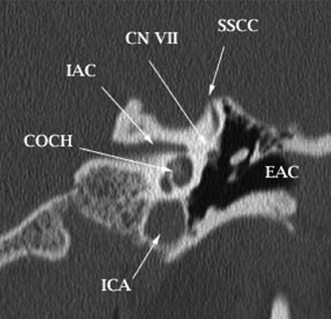
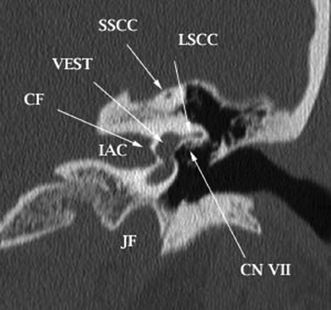
Fig. 4.9 Normal anatomy: a coronal reformatted CT image of the temporal bone. The superior and inferior divisions of the vestibular nerve course in the internal auditory canal (IAC) and are separated by the crista falciformis (CF). LSCC, lateral semicircular canal; CN VII, tympanic segment of the facial nerve; SSCC, superior semicircular canal; VEST, vestibule; JF, jugular foramen.
The jugular foramen is the bony channel in which the sigmoid sinus connects to the internal jugular vein at the level of the nasopharyngeal carotid space. This foramen courses anteriorly laterally and inferiorly as it insinuates itself between the medial petrous temporal bone and the occipital bone.3,4 The endocranial opening of the jugular foramen is usually divided by a fibrous (more common) or bony septum into two compartments, the smaller anteromedial pars nervosa and the larger posterolateral pars vascularis (Fig. 4.6 and Table 4.1). Although these names suggest otherwise, the pars nervosa and pars vascularis both contain important vascular and neural structures. The pars nervosa contains both the inferior petrosal sinus and the glossopharyngeal (IX) nerve. The inferior petrosal sinus drains the cavernous sinus and courses in the petro-occipital fissure adjacent to the clivus prior to its exit through the pars nervosa and subsequent drainage into the internal jugular vein just beneath the jugular foramen (Fig. 4.6).4,5 After emerging from the lateral aspect of the medulla as multiple rootlets, cranial nerve (CN) IX forms a single bundle that courses a short distance before making a sharp bend at its genu lodged just below the external opening of the cochlear aqueduct.6,7 At this level, the CN IX expands, forming the superior glossopharyngeal ganglion, then proceeds inferiorly along the medial aspect of the jugular bulb within the pars nervosa of the jugular foramen.6,8 Before CN IX completely exits the skull base, its tympanic branch (nerve of Jacobson) usually emerges from the inferior glossopharyngeal ganglion, also located within the jugular foramen, enters the inferior tympanic canaliculus located in the caroticojugular spine (between the ICA and internal jugular vein), and reaches the middle ear along with the inferior tympanic artery, where it ascends along the medial wall of the cochlear promontory. It supplies the main sensory fibers to the mucosa of the mesotympanum and the eustachian tube and joins the caroticotympanic nerve to form the lesser superficial petrosal nerve.6,9 The inferior tympanic canaliculus is occasionally seen on CT in cross section at the level of the caroticojugular spine.5,10
The pars vascularis of the jugular foramen contains the jugular bulb and the vagus (X) and spinal accessory (XI) cranial nerves (Fig. 4.6).4,11 Similar to CN IX, the vagus nerve also has a superior ganglion within the jugular foramen; it yields an auricular (Arnold’s) branch (cutaneous to the external ear), which travels through the mastoid canaliculus on the lateral wall of the jugular foramen to reach the descending canal of the facial nerve (Fig. 4.6 and Fig. 4.10).6 The nerves of Jacobson and Arnold contain glomus formations that can give rise to paragangliomas.5 The cranial nerves within the jugular foramen have been identified as filling defects on normal contrast-enhanced high-resolution computed tomography (CT) scans and linear structures of soft intensity on magnetic resonance imaging (MRI) when appropriate angulation and technique are utilized.11,12
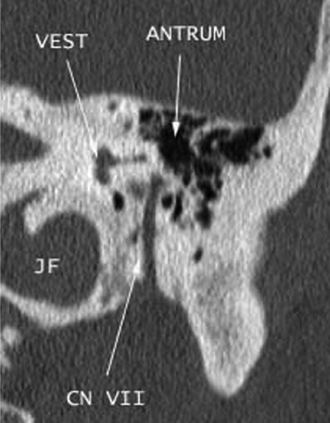
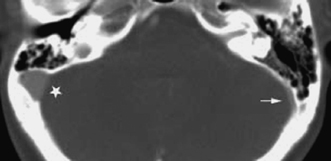
Fig. 4.11 Asymmetric sigmoid sinus. Axial enhanced computed tomography image through the temporal bones shows asymmetry in size of the venous sinuses, the right sigmoid sinus (∗) larger than the left (arrow). This is a normal variant and should not be confused with pathology, as the cortices are smooth without bony destruction. Evaluation of the remainder of the venous system (not shown) reveals that the entire right side was larger than the left.
The CT and MRI appearance of the jugular foramen depends on the level and angulation of the study. Detailed CT anatomy is best appreciated on axial sections (Fig. 4.5, Fig. 4.6, and Fig. 4.7).5,11 Vascular anatomy is best seen on MRI in the axial and sagittal planes (Fig. 4.2, Fig. 4.3, and Fig. 4.4). There is often considerable variation in the size and symmetry of the normal jugular foramen, with the right side usually larger than the left.5,13 The bony margin, not the size of the foramen, should guide diagnostic evaluation. One should not confuse an extremely large normal foramen with a pathological process, as a normal foramen will always be well corticated (Fig. 4.12). An exception to the rule may be a long-standing endocranial arteriovenous anomaly that drains by way of the jugular foramen. This may cause nonerosive well-corticated pathological enlargement. “Normal” measurements are available but are impractical in day-to-day evaluation. Irregular, jagged margins are never normal.
| Pars Nervosa (smaller anteromedial portion) |
| Inferior petrosal sinus |
| CN IX (glossopharyngeal nerve) |
| Proximal portion of the tympanic branch of IX (Jacobson’s nerve) |
| Pars Vascularis (larger posterolateral portion) |
| Jugular bulb |
| CN X (vagus nerve) |
| Auricular branch of X (Arnold’s nerve) |
| Associated posterior jugular paraganglion |
| Distal portion of Jacobson’s nerve |
| Associated posterior jugular paraganglion CN XI |
| (spinal accessory nerve) |
Normal Arterial Anatomy
The petrous portion of the ICA courses through the temporal bone in a bony tunnel termed the carotid canal (Fig. 4.5, Fig. 4.6, and Fig. 4.7). It is accompanied by the periarterial sympathetic plexus, which forms the deep petrosal nerve.
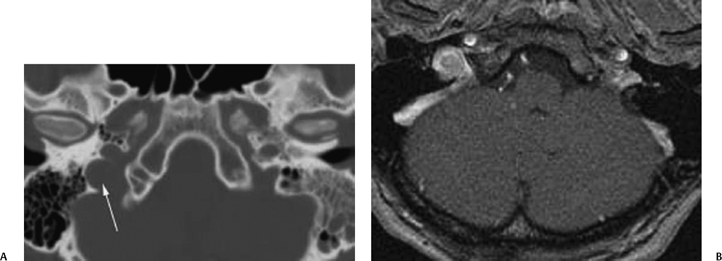
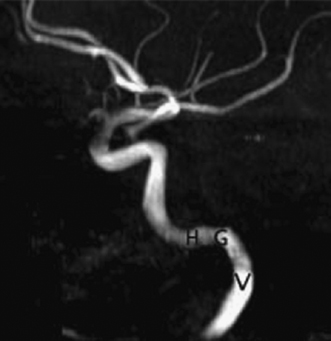
Fig. 4.13 Magnetic resonance angiography of the internal carotid artery (ICA). Maximal intensity projection image of the ICA in the lateral projection demonstrates the normal anatomy of its petrous segment. There are three segments of the petrous ICA, the vertical segment (V) that courses through the petrous temporal bone, the posterior genu (G) that bends anterolateral to the cochlea, and the horizontal segment (H).
Because of this anatomic relationship, injury to the carotid artery in this area, such as occurs in dissection, will often present as an incomplete Horner’s syndrome (miosis, ptosis, but not anhidrosis). This kind of incomplete Horner’s syndrome is also referred to as oculosympathetic palsy.14 Incomplete Horner’s syndrome occurs due to sparing of sudomotor fibers to the face that travel along the external carotid artery (ECA), whereas the pupillomotor fibers travel along the ICA after synapsing in the superior sympathetic ganglion. According to the classification system described by Bouthillier et al,15 there are three segments to the petrous ICA – a vertical or ascending segment, a genu (posterior loop of the ICA), and a horizontal segment (Fig. 4.13).16,17 The ICA enters the skull base through the carotid canal, ascending vertically in the petrous temporal bone to the level of the cochlea (Fig. 4.5, Fig. 4.6, and Fig. 4.7). At this level, the canal and artery make an anteromedial bend of ∼90 degrees, coursing horizontally in an anteromedial direction, ending at the apex of the petrous pyramid, just cephalad to the foramen lacerum (Fig. 4.6 and Fig. 4.7). A small branch, the caroticotympanic artery, arises from the petrous ICA near its genu and perforates the bony plate of the carotid canal to enter the posteromedial tympanic cavity.18 This vessel will become important in the discussion of the origins of the aberrant carotid artery.
The petrous ICA vertical segment can be identified on both axial and coronal CT and MR images. On axial section (Fig. 4.5 and Fig. 4.6), the vertical segment is located anterior to the jugular bulb, separated by the caroticojugular spine. On coronal CT images (Fig. 4.8), the vertical segment is located inferior to the cochlea and medial to the head of the malleus in the tympanic cavity.15
The petrous ICA horizontal segment is best seen on axial MR or CT sections (Fig. 4.3 and Fig. 4.7). At the genu of the horizontal and vertical portions, the canal is separated from the posterolateral middle ear cavity by a relatively thin bony plate.16 Its course then parallels the more anterolateral eustachian tube and tensor tympani muscle toward the petrous apex, forming the roof of the foramen lacerum before ascending into the cavernous sinus. Superficial and just lateral to the horizontal segment of the petrous ICA, the greater and lesser superficial petrosal nerves, respectively, course within their own distinctive grooves.15 The CT appearance of the horizontal segment of the carotid canal is relatively constant. Conventional unenhanced spin echo MRI, however, does not effectively demonstrate the petrous ICA because the low signal of flowing arterial blood next to the low signal of bone makes identification of the normal artery difficult. The combination of source images and reprojection images found in MR angiography (MRA) has vastly improved the ability of MRI to identify the normal and diseased petrous ICA (Fig. 4.13).
Pathology
Vascular Lesions of the Temporal Bone
The vascular structures of the temporal bone course between different compartments of the head and neck; hence, they can serve as conduits for the spread of disease, particularly neoplastic and infectious processes.
Tumors from the nasopharyngeal mucosal area (squamous cell carcinoma, non-Hodgkin’s lymphoma, minor salivary gland malignancies) and adjacent deep facial spaces will spread along paths of least resistance, following a perivascular course through the skull base along the carotid canal (Fig. 4.14). These tumors will often encase and narrow the ICA, but they rarely result in complete occlusion.
Infections of the nasopharyngeal carotid space may affect the vertical portion of the petrous ICA (Fig. 4.15), whereas apical petrositis will more commonly involve the more distal horizontal petrous ICA.
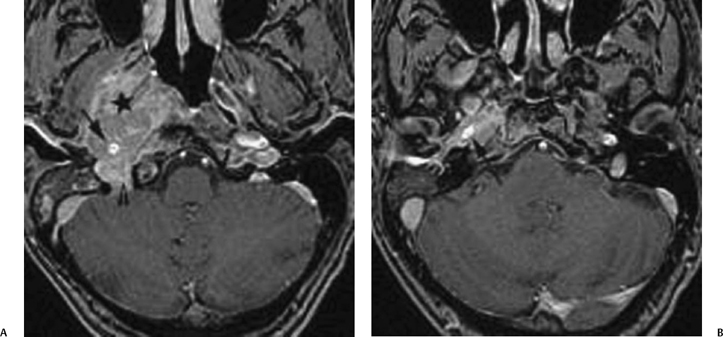
Fig. 4.14 Perivascular spread of nasopharyngeal cancer. A 53-year-old man presented with known nasopharyngeal squamous cell carcinoma for radiation treatment. (A) Axial enhanced T1-weighted MR image obtained on a 3.0 Tesla unit shows a large enhancing mass arising from the lateral wall of the right nasopharynx (*) encasing the vertical segment of the petrous internal carotid artery (arrow) and also extending into the jugular foramen (arrowhead). (B) Slightly higher level shows that the enhancing nasopharyngeal tumor travels along the carotid canal and continues to encase the horizontal segment of the right petrous internal carotid artery (arrow).
Venous Sinus Thrombosis
Venous structures of the temporal bone, including the transverse sinus, sigmoid sinus, and internal jugular bulb/ vein, are subject to thrombophlebitis and thrombosis. The proximity of the mastoid air cells makes the sigmoid sinus particularly vulnerable to inflammatory processes involving the mastoids. When infection affects these air cells, secondary thrombosis of the sigmoid sinus and adjacent transverse sinus or jugular bulb and internal jugular vein may occur (Fig. 4.16). When this occurs, severe intracerebral complications may ensue.19,20 Venous infarction of the temporal lobe is one of the more common complications seen in this setting as the vein of Labbé drains the posterolateral temporal lobe directly into the junction of the transverse and sigmoid sinuses (Fig. 4.1B).19,21
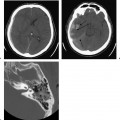
MRI and MR venography (MRV) can be very helpful in diagnosing transverse and sigmoid sinus thrombosis in its early phase, prompting therapy before more serious sequelae appear. Care must be taken with this diagnosis, however, because asymmetry in the size of the transverse/ sigmoid sinuses and jugular bulb is a common anatomic variant. Whereas the hypoplastic side may mimic sinus thrombosis due to its small size (Fig. 4.17D), the more prominent contralateral side may demonstrate slow or turbulent flow that can also mimic thrombosis on conventional MRIs (Fig. 4.17).12,22 The diagnosis of venous sinus thrombosis can be made only after studying all available MRI sequences and confirming abnormal signal within the venous sinuses on all images (Fig. 4.18).
Conventional angiography can be used to confirm diagnosis suspected on cross-sectional imaging and provide a means for endovascular thrombolysis.
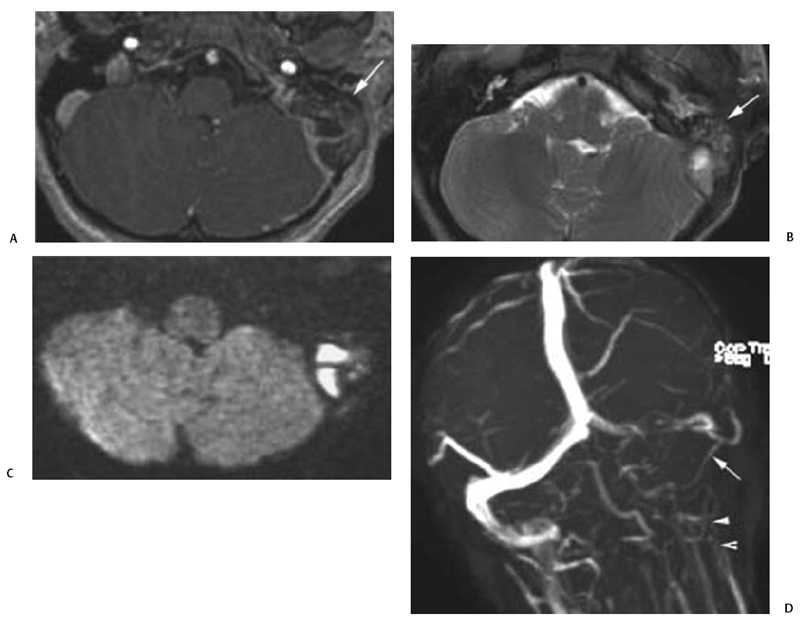
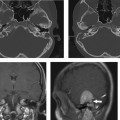
Fig. 4.16 Mastoiditis causing dural sinus thrombosis. A 12-year-old child presented with persisting fever, left ear pain, and drainage, despite completing a course of antibiotics. (A) Axial postgadolinium T1-weighted magnetic resonance image (MRI) demonstrates a filling defect in the left sigmoid sinus, indicating thrombus with enhancement within the left mastoid air cells (arrow). (B) Axial T2-weighted MRI demonstrates inflammatory debris within the left mastoid air cells with heterogeneous signal (arrow) and loss of flow void within the left sigmoid sinus. (C) Axial diffusion weighted MRI shows restricted diffusion within the left mastoid air cells and sigmoid sinus compatible with abscess formation. (D) MR venography reformatted in the coronal plane demonstrates nonvisualization of the sigmoid sinus (arrow) and internal jugular vein (arrowheads), confirming extensive thrombosis. Filling defect in the left transverse sinus is compatible with partial thrombus. (Images courtesy of Michael Jay, MD.)
Lesions of the Jugular Foramen
The jugular foramen as a distinct anatomic site in the inferomedial temporal bone, like the petrous apex, commands its own site-specific differential diagnosis list (Table 4.2). Because of the complex surgical issues for a lesion of the jugular foramen, both axial and coronal CT (using soft tissue and bone algorithm) and enhanced MR imaging are usually employed for presurgical planning. Although it is not always possible to suggest the histological diagnosis from CT and/or MR images, many of the lesions that involve the jugular foramen either primarily or secondarily have distinctive radiological features.
When confronted by an abnormality of the jugular foramen on CT or MRI, the radiologist must first decide if the lesion is real or one of the “do not touch” lesions found in this area (Table 4.2). As described previously, the bony jugular foramen and the jugular bulb may be normally quite asymmetric in size (Fig. 4.12). Flow-related artifacts on MRI (Fig. 4.17A) can occasionally mimic, and thus must be differentiated from venous thrombosis (Fig. 4.18A) or schwannoma (Fig. 4.22). Once these “do not touch” lesions have been excluded, the radiologist may proceed with an attempt to differentiate the group of real mass lesions of the jugular foramen.
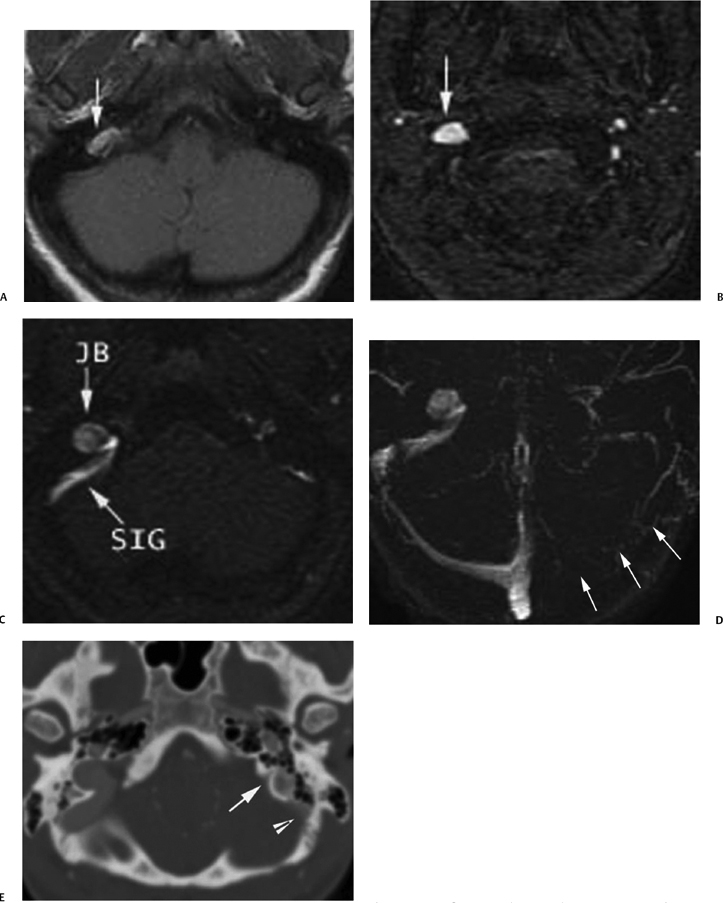
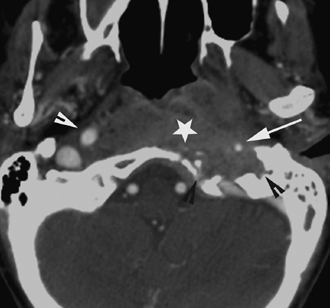
Fig. 4.17 Asymmetric dural sinuses mimicking thrombus. (A) Unen-hanced axial T1-weighted magnetic resonance image demonstrates a hyperintense focus (arrow) in the region of the right jugular bulb, which may mimic a mass or venous thrombus. (B) Axial two-dimesional (2D) time-of- flight magnetic resonance venogram (2D TOF MRV) source image shows flow-related enhancement in the area of question, confirming normal flow through this area. (C) More superiorly, axial 2D TOF MRV shows that the hyperintense focus is contiguous with the sigmoid sinus (SIG), consistent with a normal jugular bulb (JB) relative to the hypoplastic left venous system. T1-weighted hyperintensity in Fig. 4.18Awas likely related to flow alterations in the enlarged jugular bulb. (D) Axial MRV maximal intensity projection (MIP) image demonstrates apparently complete absence of the left transverse and sigmoid sinuses and jugular bulb (arrows). The imager must be diligent in reviewing all images to ensure that this appearance is not due to a hypoplastic venous system, as in this case, in which the entire ipsilateral venous system is small. Note the nearly identical appearance of this image with the ones of pathologic thrombosis (Fig. 4.16D and Fig. 4.18B). (E) Enhanced computed tomography (CT) image of the head in bone window can better define bony anatomy. This CT image shows that the left jugular foramen is very small (arrow) compared with the right, consistent with developmental hypoplasia. The sigmoid sinus (arrowhead), as expected, is also hypoplastic.
Although multiple potential lesions of the jugular foramen are listed in Table 4.2, statistically speaking paraganglioma, schwannoma, and meningioma make up the vast majority of the tumors found within this structure. Of these three, paraganglioma (glomus jugulare or glomus jugulotympanicum) is the most common and will be discussed in detail in the Pulsatile Tinnitus section of this chapter.
Paragangliomas, schwannomas, and meningiomas have specific characteristics, including different growth patterns and effects on the surrounding bone, that can be helpful in differentiating them on imaging. Paragangliomas typically extend from the jugular foramen in a superolateral direction to involve the medial hypotympanum.23 CT shows a permeative destructive pattern with erosion of the jugular spine and foramen (Fig. 4.19). The combination of extreme tumor vascularity and permeative margins is highly suggestive of the diagnosis of paraganglioma.24,25 On T1-weighted images (T1WI), MRI most commonly demonstrates hypointense flow voids within the tumor (pepper) parenchyma, whereas hyperintense foci of methemoglobin within the tumor interstices (salt) is seen far less commonly (Fig. 4.20).26
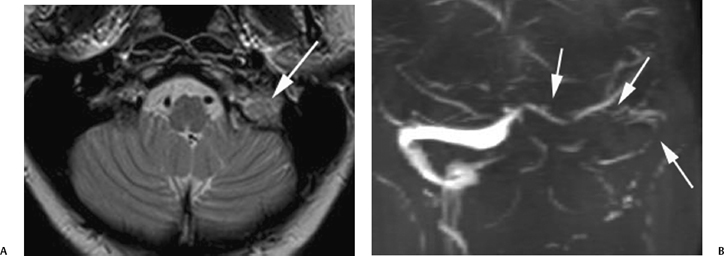
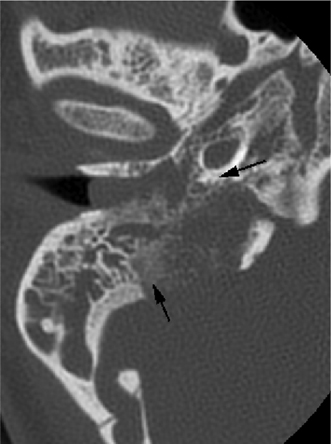
Fig. 4.19 Permeative destruction of glomus jugulotympanicum. Axial unenhanced computed tomography image through the right temporal bone demonstrates permeative destruction of the right jugular foramen with loss of normal cortex (arrows). A soft tissue mass is seen extending into the middle ear cavity and external auditory canal. This appearance is typical of paragangliomas.
| “Do Not Touch” Lesions |
| Asymmetrically enlarged jugular bulb (MRI)* |
| Asymmetrically enlarged jugular foramen (CT)* |
| Slow or turbulent flow in large or high jugular bulb (MRI)* |
| Vascular Lesions |
| Sigmoid sinus, jugular bulb, internal jugular vein thrombosis* |
| Arteriovenous fistula or malformation (enlarged jugular bulb) |
| Tumors |
| Glomus jugulare or jugulotympanicum paraganglioma* |
| Schwannoma (CN IX, X, XI)* |
| Neurofibroma (CN IX, X, XI) |
| Meningioma |
| Lateral clival chordoma |
| Metastasis |
| Chondrosarcoma (petro-occipital synchondrosis) |
| Invasive nasopharyngeal carcinoma |
| *Most common lesions |
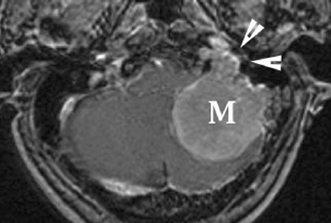
Schwannomas of the jugular foramen usually originate from CN IX. CN IX deficits, however, are unusual unless a significant portion of the schwannoma is below the skull base.27 Most patients present with decreased hearing and, less often, vertigo and ataxia likely related to compressive effects of the mass on CN VIII.27,28 Schwannomas follow the course of CN IX and typically demonstrate a superomedial vector of growth toward the lateral aspect of the brainstem.23 As schwannomas rarely grow into the middle ear cavity, otoscopic evaluation is most commonly negative in these patients.29 On CT, these lesions are usually isodense to brain parenchyma and cause enlargement of the jugular foramen with sharp, rounded, and thin sclerotic rims (Fig. 4.21 ).23,27,29 When the lesion projects downward into the nasopharyngeal carotid space or upward into the basal cisterns, it becomes characteristically dumbbell-shaped (Fig. 4.22).30 MRI typically demonstrates low T1- and high T2-weighted signal with uniform enhancement, but cystic components may be seen, particularly in larger lesions (Fig. 4.23).29 Unlike paragangliomas, flow voids within the lesion are conspicuously absent. Schwannomas are also less likely to infiltrate and insinuate into surrounding structures and are thus technically easier to remove surgically, but they are less responsive to radiation than paragangliomas. They are also slower growing and are less likely to exhibit malignant behavior.30,31
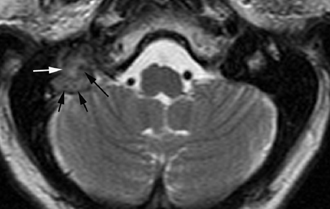
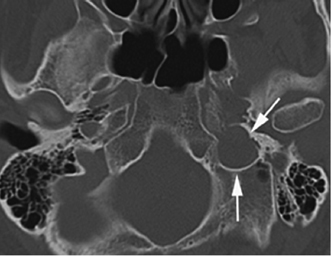
Fig. 4.21 Smooth remodeling of schwannoma. Axial unenhanced computed tomography image demonstrates a mass causing smooth expansion of the left jugular foramen (arrows). Note the bony margins remain sharp with thin sclerotic rims.
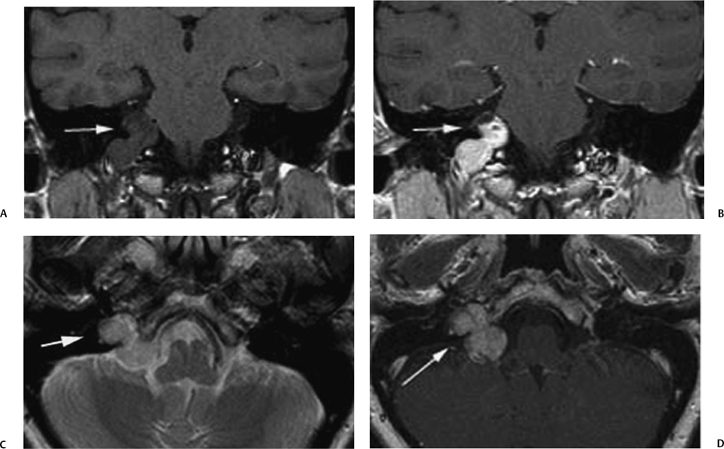
Fig. 4.22 Dumbbell-shaped schwannoma. A 48-year-old woman presented with dizziness. (A) Coronal unenhanced and (B) postgadolinium T1-weighted magnetic resonance images demonstrate a diffusely enhancing, dumbbell-shaped mass (arrow) that extends through the jugular foramen into the basilar cisterns. (C) The mass is hypointense relative to CSF (arrow) on this T2-weighted MR image, and has no flow voids, a finding that can be helpful in distinguishing a schwannoma from a paraganglioma. (D) Axial postgadolinium T1-weighted MR image shows the enhancing mass in the right jugular foramen and cerebello-medullary angle (arrows).
The jugular foramen is a rare location for meningioma, accounting for 4% of posterior fossa meningiomas in the largest neurosurgery series.32,33 These tumors arise from arachnoidal cells of the meninges and usually occur in adults between the ages of 20 and 60 years. Although they are most commonly found in a parafalcine location or over the cerebral convexity, -33% arise from the meninges associated with the skull base.34 Because the arachnoidal cells may be found anywhere along the meninges, meningiomas can be found on any of the meningeal-lined surfaces of the temporal bone. Clinical presentation is similar to schwannomas with hearing loss and cranial neuropathies (CN V through XII) being common. Unlike schwannomas, however, meningiomas can present as a vascular tympanic mass, as they may secondarily extend into the middle ear cavity.35 Meningiomas of the jugular foramen can be either primary or secondary.36 Posterior fossa meningiomas with secondary extension into the jugular foramen have imaging characteristics similar to meningiomas elsewhere. They are solid, well-circumscribed, extraaxial, dural-based masses often showing an en plaque pattern of growth (Fig. 4.24). Strong uniform enhancement is seen, often with a dural tail at its margin. Primary jugular foramen meningiomas, on the other hand, are characterized by extensive skull base infiltration and a “centrifugal” pattern of growth.23 This includes growth into the middle ear cavity laterally, the jugular tubercle, hypoglossal canal, occipital condyle, and clivus medially, and the nasopharyngeal carotid space inferiorly. The skull base infiltration has a “permeative-sclerotic” appearance on CT; the margins of the jugular foramen are irregular with a combination of erosive and sclerotic changes. The hyperostotic bony response characteristic of meningiomas in other locations is not typical for primary jugular foramen meningiomas. Treatment of jugular foramen meningiomas is surgical resection, but these lesions have the highest likelihood of recurrence after surgery compared with paragangliomas and schwannomas.
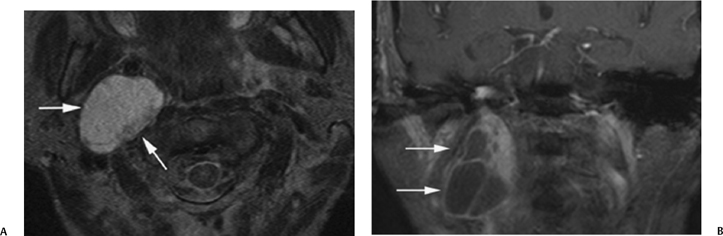
Fig. 4.23 Schwannoma with cystic changes. (A) Axial T2-weighted magnetic resonance image demonstrates a large mass hyperintense relative to CSF in the right carotid space (arrows) between the anteriorly displaced internal carotid artery and posteriorly displaced internal jugular vein. (B) Coronal postcontrast magnetic resonance image shows peripheral areas of enhancement and nonenhancing cystic portions (arrows). Larger schwannomas, such as depicted here, can undergo cystic degeneration.
Primary cholesteatoma (epidermoid) is a benign congenital neoplasm made of epithelial rests of exfoliated keratin that can produce a smoothly marginated lesion of the jugular foramen on CT. Locally aggressive features are usually not seen unless large. These lesions occur in the immediate vicinity of the jugular foramen, usually emanating from the petrous apex or middle ear cavity. On MRI, primary cholesteatomas are hypointense to isointense on T1WIs with occasional peripheral enhancement.
Other tumors that have infiltrating, destructive margins that involve the jugular foramen seen on CT are chordoma, chondrosarcoma, hematogenous metastases, and direct invasion from aggressive regional malignancies, particularly, squamous cell carcinoma of the nasopharynx.30,39 Metastases may be much more aggressive and destructive than paragangliomas (Fig. 4.25), although in their earlier stages they may be indistinguishable. There is often a rapid onset of clinical symptoms, especially cranial nerve palsies, as well as pain, which is usually not seen with schwannomas and paragangliomas. The spread of these lesions is indiscriminate with respect to the characteristic routes often followed by paragangliomas. Many metastases are vascular and may produce similar angiographic findings to those of paragangliomas. Renal and thyroid metastases are notorious in this regard.
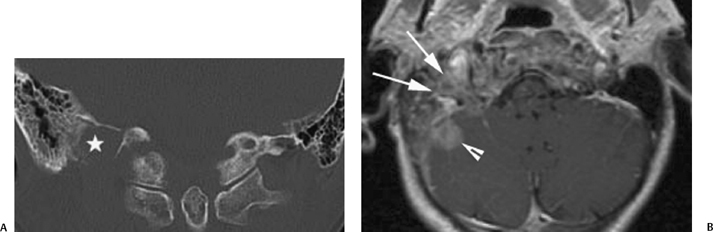
Fig. 4.25 Breast cancer metastatic to the jugular foramen. Forty-seven-year-old woman with known breast cancer presented with new pain in the right occipital region. Bone scan demonstrated increased activity at the right posterior base of skull concerning for metastatic disease. (A) Coronal unenhanced computed tomography image in bone algorithm demonstrates permeative bony destruction of the jugular foramen (∗), indicating an aggressive process. Biopsy revealed metastatic disease. (B) Corresponding axial postgadolinium magnetic resonance image demonstrates an ill-defined, heterogeneously enhancing mass extending through the jugular foramen (arrows) and involving the right cerebellar hemisphere and surrounding dura (arrowhead).
Patient Evaluation of Pulsatile Tinnitus and/or Vascular Retrotympanic Mass
One of the major indications for radiologic evaluation of the temporal bone in adults is for further assessment of tinnitus and/or a vascular retrotympanic mass.37,39 Tinnitus can be characterized as nonpulsatile or pulsatile. The term pulsatile tinnitus (PT) refers to the patient who perceives a rhythmic sound thought to be pulse-synchronous. PT may be further subcategorized into arterial and venous types. Arterial PT rises in systole and does not disappear with light pressure on the ipsilateral jugular vein. Venous PT is heard as a continuous bruit around the ear accentuated in systole but is abolished by light pressure on the ipsilateral jugular vein.40,42 When PT is perceived only by the patient, it is referred to as subjective PT; when audible to the examining physician as well, it is objective PT. PT may be associated with both normal vascular variants of the temporal bone and a wide variety of pathologic processes affecting this area (Table 4.3 ).25,37,38,43
Normal Vascular Variants Venous variants
Tumors Paraganglioma
Meningioma Endolymphatic sac adenomatous tumors Vascular metastasis (renal, thyroid, etc.) Acquired Vascular Lesions Dural arteriovenous fistula* Extracranial direct arteriovenous fistula Atherosclerotic carotid artery stenosis Fibromuscular dysplasia Internal carotid artery dissection Petrous internal carotid aneurysm Transverse sinus stenosis Large vessel arteritis Miscellaneous Causes Otomastoiditis Paget’s disease of the temporal bone Osteolytic phase of otosclerosis Idiopathic or benign intracranial hypertension (pseudotumor cerebri) |
*More common lesions
Arterial Causes Congenital
Acquired
Arteriovenous High-Flow Causes Vascular
Tumor
Miscellaneous
Venous Causes Congenital
Acquired
|
Another way of grouping the causes of PT is to consider the three underlying mechanisms for the creation of a pulse-synchronous sound: arterial jetting, arteriovenous shunting, and venous turbulent flow (Table 4.4).42 Vascular tympanic membrane is the term used to describe the red or blue appearance of the TM on otoscopic examination as a result of a vascular retrotympanic mass.37,39 A vascular TM can be seen with normal vascular variants, paragangliomas, and certain chronic inflammatory conditions of the middle ear (Table 4.5). It is often impossible for the clinician to distinguish between these entities on otoscopic examination.39,44 Because misidentification of normal vascular variants as pathological lesions may lead to serious complications if biopsy is attempted, pretreatment radiological evaluation and diagnosis is essential.
Given the anatomic complexity of the temporal bone and the varying imaging modalities and protocols available, the radiologist’s task of ruling out a vascular temporal bone lesion may be quite formidable. Radiological evaluation can be simplified and made more cost-effective if the type of tinnitus (objective versus subjective, arterial versus venous) and the appearance of the TM are known prior to radiological evaluation. Utilizing this information, an algorithmic approach can be used to direct the choice of initial study (Fig. 4.26).37,39 Contrast-enhanced high-resolution CT of the temporal bone has become the study of choice for the initial evaluation of both objective and subjective types of PT, particularly in the presence of a retrotympanic mass.40 Because the most common causes of PT are vascular abnormalities within the middle ear and otic capsule, CT offers an advantage over MRI in evaluating temporal bone anatomy, structures embedded within bone, and the effects of a lesion on its bony surroundings (i.e., erosion, remodeling, hyperostosis).40 Whereas CT is used as the first line of diagnostic problem-solving, MRI has a complementary role in further delineating the soft tissue characteristics and extent of a lesion.
In the setting of objective PT and normal CT and MRI examinations, angiography is recommended as the next imaging study to exclude the presence of dural arteriovenous fistulas (DAVFs), as these lesions are notoriously difficult to appreciate on cross-sectional imaging. To ensure a complete evaluation, it is imperative that both the anterior (external and internal carotid artery) and posterior (vertebral artery) circulations are studied.
Arterial Causes Aberrant internal carotid artery* Lateralized internal carotid artery Petrous internal carotid artery aneurysm (with dehiscent carotid plate) Venous Causes Dehiscent jugular bulb* Infectious Inflammatory Causes Cholesterol granuloma* Otomastoiditis with hemorrhage Tumors Glomus tympanicum paraganglioma* Glomus jugulotympanicum paraganglioma* Large meningioma |
*Most common lesions
If atherosclerotic disease is the suspected etiology, CTA of the head and neck can be performed primarily or secondarily.45 Recently, Krishnan et al46 proposed that employing CTA and CTV as the single initial study for evaluating patients with PT but no retrotympanic mass may obviate the need for multiple examinations for diagnosing and planning treatment for PT, as this examination can accurately diagnose the bony, neoplastic, and vascular etiologies of PT. In their study, the CTA and CTV were performed simultaneously with a single acquisition of images after a fixed delay that allowed imaging of both the arterial and venous structures. The images were also reviewed in bone windows, allowing excellent evaluation of the temporal bones in multiple planes. If a dural AVF was suspected, however, conventional angiography remained the gold standard for the evaluation of this entity.
The four broad categories for PT and retrotympanic masses are vascular variants and congenital anomalies, acquired vascular lesions, neoplasms, and chronic inflammatory lesions of the middle ear cavity. Table 4.3 lists the processes that generally cause subjective and objective tinnitus. The causes of a vascular-appearing TM are listed in Table 4.5.
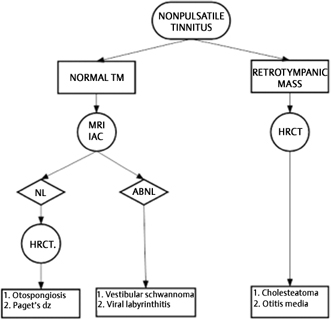
Fig. 4.26 Imaging algorithm for the work-up of a patient with non-PT. MRV, magnetic resonance venography; MRA, magnetic resonance angiography; CTA, computed tomography angiography; ICA, internal carotid artery; DAVF, dural arteriovenous fistula; gad, gadolinium. (Adapted from Weissman JL, Hirsch BE. Imaging of tinnitus: a review. Radiology 2000;216(2):342-349. Reprinted with permission.)
Etiology
Vascular Variants and Congenital Anomalies
Particular variations and anomalies in vascular anatomy in the temporal bone are a frequent cause of PT and a vascular-appearing TM. These include the jugular bulb variants/anomalies (high jugular bulb, dehiscent jugular bulb, and jugular bulb diverticulum), aberrant ICA, and the rare persistent stapedial artery.4,47–49 When these vascular anomalies present with PT and a vascular TM, differentiation from neoplasms becomes crucial prior to biopsy. Contrast-enhanced high-resolution CT of the temporal bone is the principal imaging tool used to diagnose these normal vascular variants and congenital anomalies, as bony detail is better delineated on CT than on MRI.
Jugular Bulb Variants
When a patient presents with venous PT or a vascular retrotympanic mass, jugular bulb variants may frequently be difficult to clinically differentiate from paragangliomas.44 Just as often, however, these normal venous variants can be seen on CT and MRI performed for other reasons as completely incidental findings. Recognition of these normal variants prevents misdiagnosis and unnecessary intervention.
The major jugular bulb variants include the asymmetrically large jugular bulb, high-riding jugular bulb without or with dehiscence, and jugular bulb diverticulum. The first of these, the asymmetrically large jugular bulb, is a common normal vascular variant, which only becomes an imaging problem when the radiologist discovers it in the search for a cause of PT. By itself, the asymmetrically large jugular bulb is generally not felt to be a cause of venous PT.
The jugular bulb is asymmetrically larger on the right side twice as often as it is on the left side.13,40,41 CT demonstrates asymmetry in the size of the jugular foramen with preservation of the jugular spine and all cortical margins (Fig. 4.12A
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree