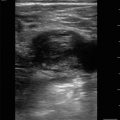
Figure 13.1
Normal testicle. Longitudinal view of normal testicle using linear probe showing homogenous testicular architecture

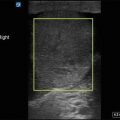
Figure 13.2
Color Doppler. Longitudinal view of normal testicle showing normal blood flow with color Doppler

Figure 13.3
Appendix testis. Testicular appendix (arrow), which represents a developmental remnant, is typically found on the upper pole of the testis near the epididymal head

Figure 13.4
Normal epididymis. Normal epididymis (arrow) seen adjacent to the testicle
Testicular Pathology
- 1.
Hydrocele
- (a)
Hydrocele is a collection of fluid between the visceral and parietal layers of the tunica vaginalis.
- (b)
Congenital hydrocele is common and occurs due to a direct communication with the peritoneum [1].
- (c)
Acquired hydroceles are typically associated with infection, tumor, trauma, torsion, or radiation therapy [1].
- (d)
- (e)
A complex hydrocele, such as hematocele or pyocele, will contain internal echoes with septations or loculations.
- (a)
- 2.
Varicocele
- (a)
Varicocele is an abnormal enlargement of the pampiniform venous plexus within the spermatic cord [1]:
Usually idiopathic which is caused by valvular incompetence of the internal spermatic vein resulting in retrograde flow into the pampiniform plexus [1]:
Ninety-nine percent of idiopathic varicoceles occur on the left [1] due to anatomical differences in between the right and left spermatic veins:
Secondary causes are usually due to compression of the spermatic vein due to various pathology such as a mass, hydronephrosis, or hepatomegaly [1]. Malignancy should also be considered.
- (b)
Varicoceles appear as a cluster of hypoechoic vascular structures adjacent to the testicle:
Figure 13.7—Varicocele
Video 13.5—Varicocele
- (c)
Color Doppler will demonstrate pronounced vascular flow to these hypoechoic areas:
Figure 13.8—Varicocele with color Doppler
Video 13.6—Varicocele with color Doppler
- (d)
Valsalva maneuver can increase size and flow pattern of varicoceles.
- (a)
- 3.
Testicular Torsion
- (a)
- (b)
Severity of torsion ranges from 180 to 720°, and complete occlusion of blood flow is thought to occur after 450° of torsion [2].
- (c)
B-mode (2D) imaging:
The affected testicle will appear enlarged and hypoechoic with less homogeneity compared with the unaffected testicle.
The epididymis may appear hypoechoic and enlarged, similar to how it appears in epididymitis.
- (d)
Get Clinical Tree app for offline access
Color Doppler:
Decreased color Doppler signal will be seen or, in cases of complete torsion, the absence of color Doppler signal:
Figure 13.11—Color Doppler of a normal testicle.
Figure 13.12—Color Doppler testicular torsion.
Video 13.8—Color Doppler testicular torsion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



- (a)