Key Points
- •
Causes of acute scrotal pain, such as testicular torsion, epididymitis, or incarcerated hernia, can be rapidly evaluated using point-of-care ultrasound.
- •
A working knowledge of Doppler ultrasound, including color power Doppler, adds significant value to the evaluation of the testicles and the epididymis.
- •
Because testicular ultrasonography is less frequently performed by many providers, a low threshold for consultation with radiologists and urologists should be maintained.
Background
Ultrasound has emerged as a preferred modality for evaluation of acute scrotal pain owing to atypical presentations with vague symptoms and nonspecific laboratory findings. Point-of-care ultrasound can facilitate diagnosis of most testicular pathologies with particular emphasis on pathologies that immediately pose a risk to viability of the testicle. The differential diagnosis is focused on the three most common etiologies of acute scrotal pain: testicular torsion, epididymitis, and inguinal hernia.
This chapter provides basic instruction in point-of-care testicular ultrasound. These imaging techniques can help mitigate diagnostic dilemmas that arise in acute care settings and can be used to rule in certain pathologies. When bedside ultrasound findings are indeterminate, a comprehensive diagnostic testicular ultrasound should be obtained.
Normal Anatomy
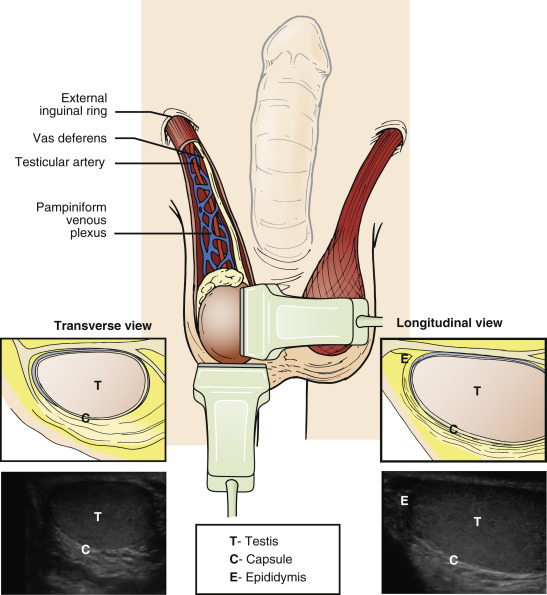
Normal male genitourinary and testicular anatomy is illustrated in Figure 25.1 .
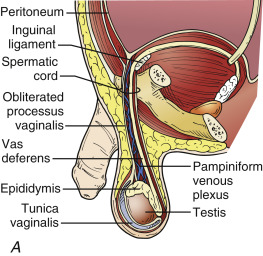
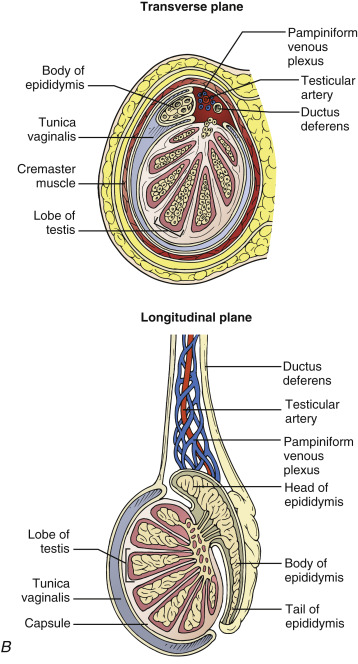
Image Acquisition
Image acquisition begins with patient comfort and proper positioning, especially in the setting of acute pain, and adequate analgesia should be provided. The patient should be brought to a private area and placed in a supine, frog-leg position. The penis should be positioned upward onto the abdomen and covered with sheets, leaving only the testicles exposed. The scrotum should be elevated with towels for comfort and to facilitate ultrasound imaging.
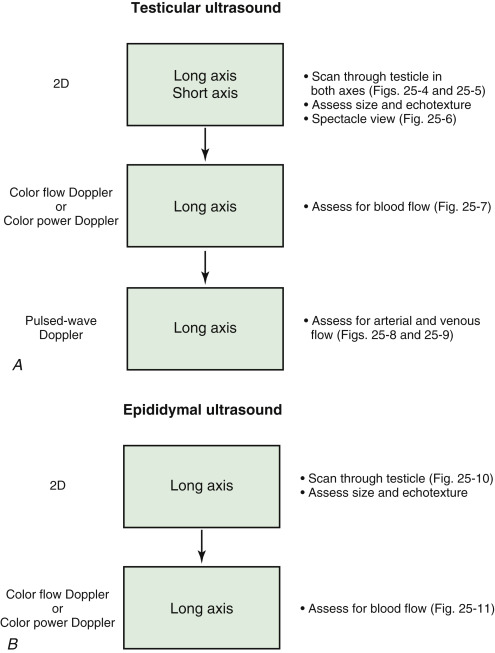
An ultrasound machine with a high-frequency transducer should be brought to the patient’s bedside and cleaned with antiseptic wipes before use. Anatomic symmetry allows providers to start by imaging the unaffected side to first gain familiarity with the patient’s normal findings. Depth, gain, and Doppler settings should always be adjusted while imaging the unaffected testicle, and the same settings are used when starting to image the symptomatic testicle. Examination of the testicles with ultrasound should be approached systematically ( Figure 25.2 ) because there are several elements to evaluate in this infrequently imaged organ.
Normal Findings
Testicles
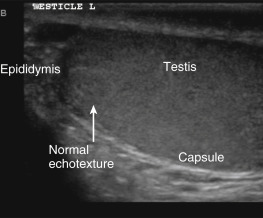
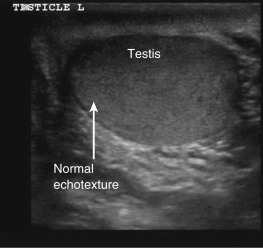
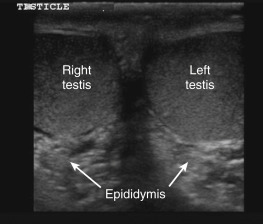
The testicles lie in the scrotum and can easily be identified with ultrasound ( Figure 25.3 ). A normal two-dimensional image of the testicle in a longitudinal plane demonstrates an oval structure with homogeneous echotexture and smooth rounded edges ( Figure 25.4 ). In a transverse plane, the short-axis view shows a circular structure ( Figure 25.5 ). A spectacle view ( Figure 25.6 ) is obtained by centering the transducer over the midline to visualize both testicles in single short-axis view, allowing side-by-side comparison of both testicles. The mediastinum testis is the confluence of septa and appears as a hyperechoic linear structure in long axis. The rete testis can be identified adjacent to the mediastinum and appears as a structure with small anechoic areas. The testicular appendage is a remnant of the mullerian duct and can occasionally be seen at the superior pole of the testicle.
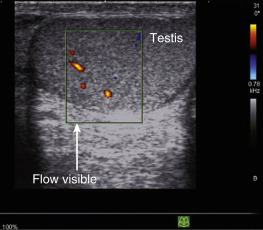
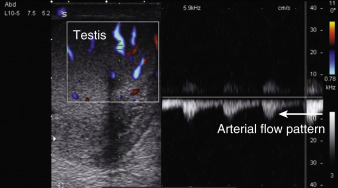
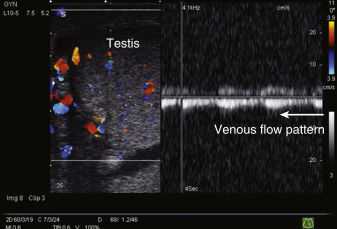
Color flow Doppler normally shows blood flow throughout the testicle ( Figure 25.7 ). Color power Doppler (CPD) has higher sensitivity for low-flow areas than color flow Doppler. Pulsed-wave Doppler (PWD) can be applied to individual vessels to differentiate arteries from veins. Arterial waveforms have a higher-velocity, pulsatile pattern ( Figure 25.8 ), and veins have a low-velocity, nonpulsatile pattern ( Figure 25.9 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree