Fig. 24.1
(a, b) Anteroposterior (AP) and lateral elbow radiographs show posterior and anterior osteophytes as well as a loose body anteriorly. Relative preservation of the articular space is noted on the AP view
Treatment
Treatment options including nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy, steroid injections, and surgery were discussed with the patient. He elected to proceed initially with conservative management including NSAIDs, an intra-articular corticosteroid injection, and an organized elbow exercise and range-of-motion program. However, the patient continued to experience significant symptoms after 3 months and did not have significant improvement in elbow range of motion.
Therefore, surgery was discussed with the patient. Surgical options considered included arthroscopic or open elbow capsular release and osteophyte excision, interposition arthroplasty, and implant arthroplasty. In this 58-year-old laborer with pain predominantly in terminal elbow flexion and extension, we felt that arthroscopic debridement and capsular release were promising surgical options.
We find advanced imaging helpful in formulating a surgical plan for osteophyte and loose-body removal. An MRI and a 3D CT scan were obtained for preoperative planning. In this case, imaging demonstrated a loose body in the coronoid fossa as well as prominent osteophytes in the coronoid process and olecranon tip. The prominent olecranon osteophytes seen in Fig. 24.2c exhibit the “Mickey Mouse ears” deformity, with osteophyte “ears” protruding from the posteromedial and posterolateral olecranon (Fig. 24.2a–c).
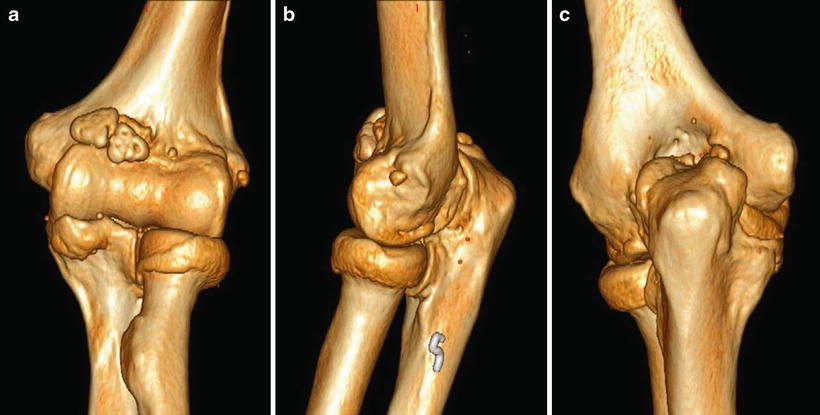
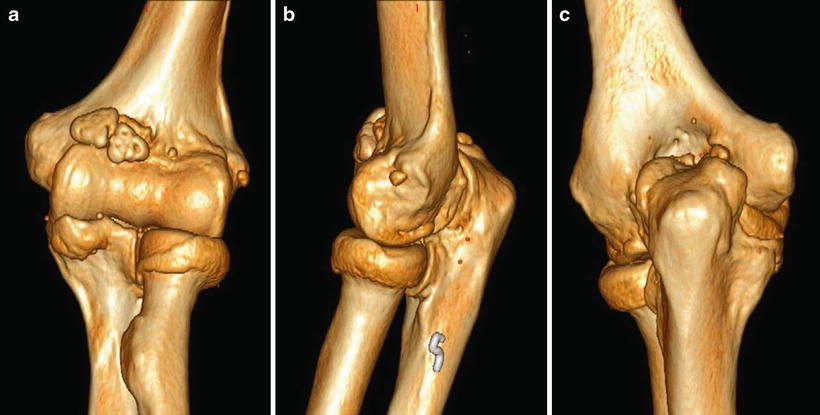
Fig. 24.2
(a, b) Three-dimensional CT images show coronoid and olecranon osteophytes as well as a loose body in the coronoid fossa. (c) Prominent posteromedial and posterolateral olecranon osteophytes create a “Mickey Mouse ears” deformity
Surgery
The patient was taken to the operating room. A general anesthetic was provided, and the patient was placed in prone position with his operative arm in an arm holder. Bony landmarks and the course of the ulnar nerve were identified and localized on the skin with a marker. The joint was insufflated with saline via the lateral soft spot portal. The standard proximal anteromedial and anterolateral portals were created. A loose body was seen in the coronoid fossa and was removed using an arthroscopic grabber via the proximal anterolateral portal. Prominent coronoid osteophytes were removed using a combination of the shaver and a small osteotome inserted through the arthroscopic cannulae.
Given the patient’s marked elbow stiffness, anterior capsular release was performed using an arthroscopic biter. The plane between the brachialis and anterior capsule was carefully developed, allowing the brachialis to protect the anterior neurovascular structures. When performing the lateral portion of the anterior capsular release, care was taken to stay proximal to the radiocapitellar joint and anterior to the radial head to avoid iatrogenic injury to the radial nerve or lateral ulnar collateral ligament.
After work in the anterior compartment was completed, standard posterolateral viewing and posterior working portals were then created. As expected from preoperative imaging, large olecranon osteophytes were visualized. These were removed using an arthroscopic shaver and a small osteotome as demonstrated in the images below. After using the osteotome, a shaver was used to gently contour the olecranon tip and to resect posteromedial and posterolateral osteophytes as well as recontour the olecranon fossa to restore its normal anatomic architecture (Figs. 24.3a, b and 24.4a–c).
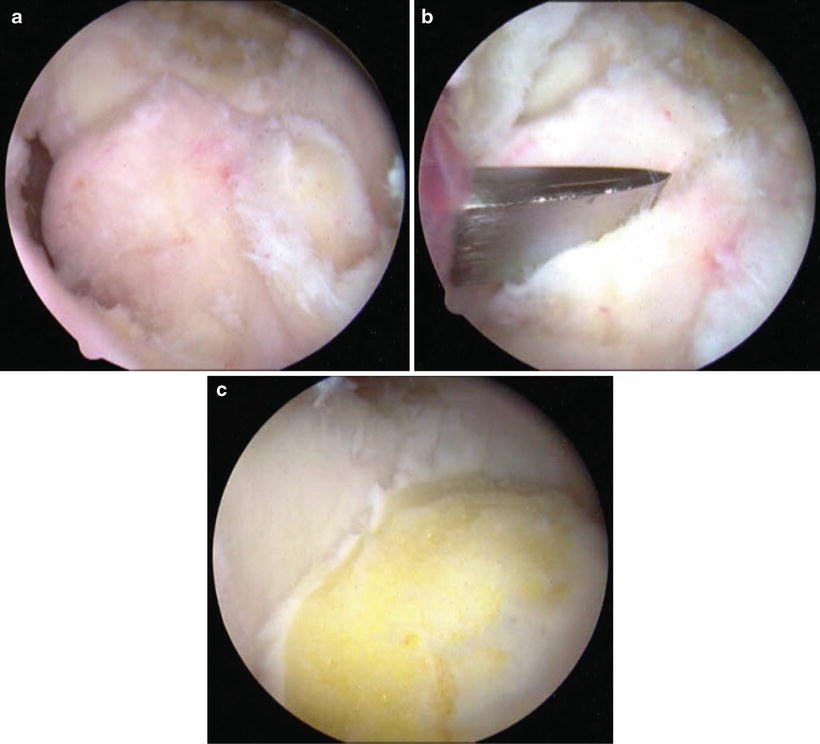
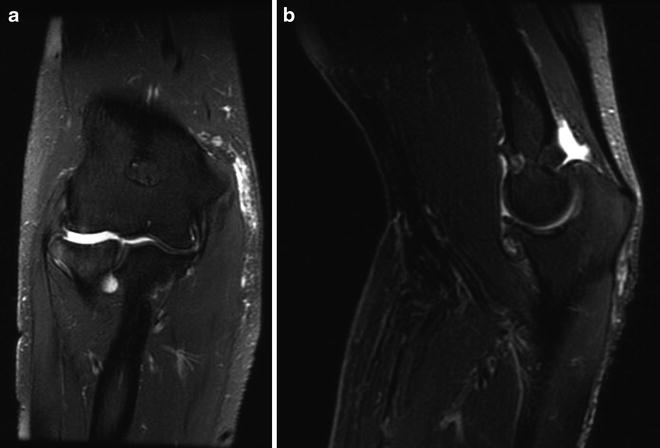
Fig. 24.3
(a) Coronal MRI demonstrating articular cartilage loss and subchondral edema. (b) Sagittal MRI demonstrating prominent coronoid and olecranon osteophytes. Hypertrophic degenerative changes in the coronoid and olecranon fossae are also noted
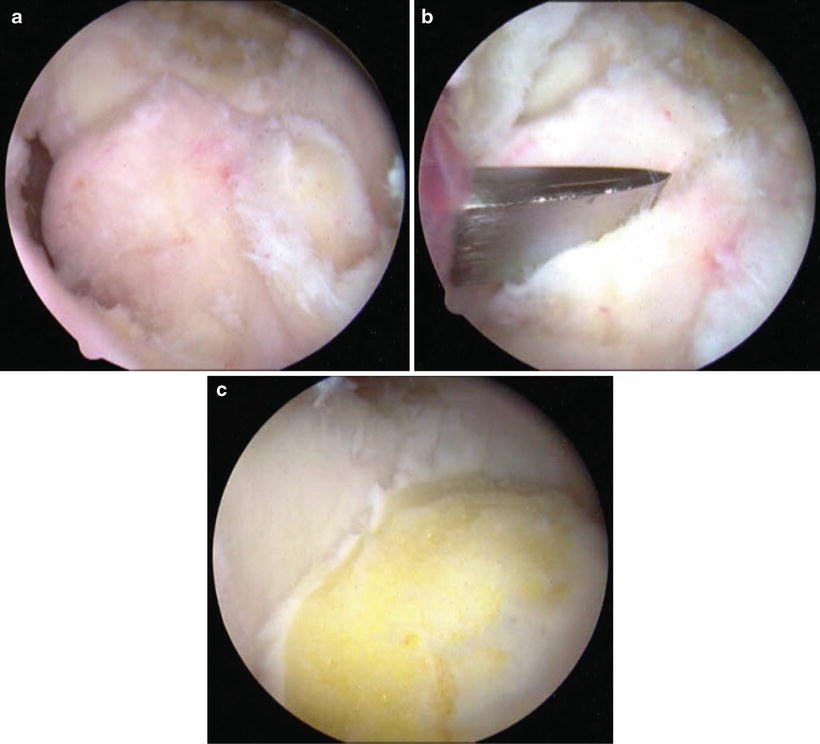
Fig. 24.4
(a) Corresponding arthroscopic view of posterior olecranon osteophytes. (b) Arthroscopic view of olecranon osteophyte removal with an osteotome. (c) Arthroscopic view of the smooth residual olecranon after osteophyte resection and final contouring
The elbow joint was then ranged while viewing the joint arthroscopically to demonstrate complete removal of all impinging osteophytes. While the elbow range of motion was improved after osteophyte resection and anterior capsular release, significant stiffness in elbow flexion remained. Therefore, arthroscopic posterior capsular release was also performed. Great care was taken posteromedially to avoid iatrogenic ulnar nerve injury. Passive elbow range of motion improved to 5–125° after the completion of posterior osteophytectomy and capsular release.
Additional procedures considered at the time of arthroscopy included radial head resection and ulnar nerve decompression and/or transposition. The patient did not have pain with forearm rotation preoperatively, and excellent outcomes after arthroscopic debridement without radial head resection have been reported [8]. Therefore, radial head resection was not performed in this case.
We did elect to decompress the ulnar nerve at the time of surgery. Ulnar nerve decompression was indicated in this case because of the patient’s preoperative posteromedial elbow pain with flexion as well as the significant improvement in elbow flexion obtained at the time of surgery after osteophyte resection and capsular release (preoperative 95° flexion improved to 125° intraoperatively). As the patient did not have evidence of ulnar nerve subluxation and had no prior ulnar nerve surgery, we performed a simple ulnar nerve decompression without transposition. This was performed at the conclusion of the surgical case by making a 3 cm incision directly over the cubital tunnel and decompressing the ulnar nerve under direct visualization.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree