The Female Pediatric Pelvis
Teresa Chapman, MD
LEARNING OBJECTIVES
1. Recognize differences in uterine morphology in the newborn, young child, and pubescent female.
2. Differentiate between didelphys uterus and bicornuate uterus.
3. Provide a single reliable diagnostic feature of ovarian torsion by pelvic ultrasound.
4. Apply a reasonable imaging protocol to the newly diagnosed simple ovarian cyst.
5. List three features that are suspicious for ovarian malignant neoplasm.
6. Describe two pelvic ultrasound findings of polycystic ovarian syndrome (PCOS).
INTRODUCTION
Abnormalities of the uterus and adnexa in the child may present with acute pain or abnormal vaginal bleeding, although congenital and acquired findings may also be identified incidentally on imaging studies of the pelvis performed for other reasons. An understanding of the normal appearance of the female reproductive organs from infancy through puberty is essential to avoid misdiagnosis. This chapter discusses the normal appearances of the pediatric uterus and ovaries as well as congenital and acquired anomalies, primarily focusing on anatomic assessment by sonography and MR imaging.
EMBRYOLOGY AND NORMAL DEVELOPMENT OF THE FEMALE REPRODUCTIVE ORGANS
Very early in embryologic development, primitive germ cells migrate from the endoderm of the yolk sac into the gonadal regions and induce mesodermal tissue to form the primitive sex cords. The germ cells together with the sex cords constitute the primitive gonads, which will begin to differentiate at 7 weeks along either a female or a male pathway. This is dependent on whether the sex-determining region of a Y chromosome (SRY) is present for expression of the male-differentiating hormones; the default pathway is female differentiation.1,2
In the absence of male hormones, the primitive gonad will develop into a fully organized ovary by 20 weeks gestational age.1 The other female reproductive organs arise from the müllerian ducts, which primitively begin as embryonic infoldings lateral to the mesonephric (wolffian) ducts. In the absence of testes and male hormones, the paired parasagittal müllerian ducts will mature further and approach each other in the midline to fuse and form the fallopian tubes, uterus, and upper two-thirds of the vagina; the distal third of the vagina develops from the urogenital sinus. In the normal female, the uterine body and uterine cervix differentiate and the uterine wall thickens by 12 weeks of gestational age.1,2
In the newborn, the uterine cervix is at least twice the length of the corpus. During the neonatal period, the uterus and ovaries are prominent in size because of maternal hormonal stimulation. The normal uterus in the newborn appears tubular, with the anteroposterior diameter of the cervix matching that of the fundus. Gradually over a period of months, the thickness of the uterus diminishes (Fig. 22.1). Neonatal ovaries may show several small follicles that gradually disappear. The uterus grows slowly until puberty; thereafter, in the postpubertal female, the corpus is approximately twice the length of the cervix.3,4
MÜLLERIAN DUCT ANOMALIES
In adult patients, müllerian duct anomalies (MDAs) may be suspected in the setting of infertility, whereas MDAs in children are more often suspected in the context of primary amenorrhea or discovered incidentally. In younger patients, US is the preferred diagnostic imaging modality because it is readily available and rapidly done without the need for general anesthesia. Field-of-view restrictions with US, patient body habitus, and artifact from bowel gas may limit sonographic assessment, however. MR imaging can provide detailed anatomy of both the uterine cavity and external contours and has shown excellent agreement with clinical müllerian duct subtype diagnosis.5 Renal anomalies are associated with MDAs in up to 30% of cases,6 and therefore, it is important to include assessment of the kidneys in these cases. Renal abnormalities include agenesis, hydronephrosis, collecting system duplication, and renal cystic diseases.2,6, 7 and 8
Agenesis of the uterus and vagina (Mayer-Rokitansky-Kuster-Hauser syndrome)
Failure of the müllerian ducts to develop results in congenital absence of the uterus and vagina. The incidence of this disorder among newborn females is approximately 1 per 4,000 to 10,000.7,8
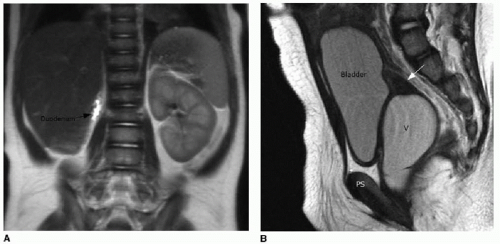
Females with müllerian agenesis have normal external genitalia, and therefore, the diagnosis is rarely made in infancy. Girls with this disorder will present with primary amenorrhea around or after the expected time of puberty. Because the ovaries develop independently of the müllerian ducts, these individuals have normal secondary sex characteristics. The vagina, however, is either completely absent or a small dimple representing the urogenital sinus origin of the distal vagina is present. Although not usually palpable on clinical exam, rudimentary uterine horns connected to small fallopian tubes are often present and are usually located on the pelvic sidewall adjacent to the ovary. These small structures may be seen on MR imaging (Fig. 22.2). In a small percentage of cases, the endometrium in this rudimentary horn may be functional.6
Females with müllerian agenesis have normal external genitalia, and therefore, the diagnosis is rarely made in infancy. Girls with this disorder will present with primary amenorrhea around or after the expected time of puberty. Because the ovaries develop independently of the müllerian ducts, these individuals have normal secondary sex characteristics. The vagina, however, is either completely absent or a small dimple representing the urogenital sinus origin of the distal vagina is present. Although not usually palpable on clinical exam, rudimentary uterine horns connected to small fallopian tubes are often present and are usually located on the pelvic sidewall adjacent to the ovary. These small structures may be seen on MR imaging (Fig. 22.2). In a small percentage of cases, the endometrium in this rudimentary horn may be functional.6
Müllerian agenesis is associated with abnormalities of the upper urinary tract, as well as with spine and skeletal abnormalities. The incidence of major urinary tract anomalies such as unilateral renal agenesis, unilateral or bilateral pelvic kidney, or horseshoe kidney is approximately 15% in patients with müllerian agenesis.1,2,8 Anomalies of the skeletal system primarily affect vertebral body development and occur in approximately 5% to 10% of women with müllerian agenesis.8,9
Unicornuate uterus
A single uterine horn, or unicornuate uterus, develops if one of the primitive müllerian ducts fails to elongate caudally and does not reach the urogenital sinus. The side that does elongate properly will have a uterine cavity that normally communicates with the vagina. In approximately one-third of cases, there will be a rudimentary horn present with functioning endometrium; it is these cases that present with symptoms of dysmenorrhea or hematometra, due to obstruction of the functioning rudimentary horn. In another third of cases, there will be a rudimentary horn without functioning endometrium. Finally, a third of cases have no demonstrable rudimentary horn.2,6,10
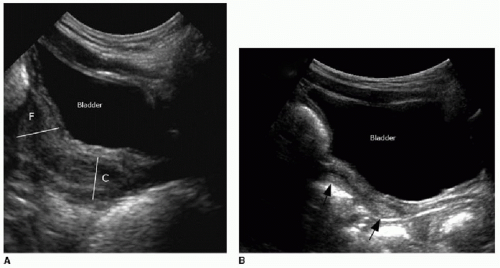
Ultrasound of a unicornuate uterus shows an asymmetric ellipsoid-shaped uterus (Fig. 22.3A). Improved characterization by MR imaging is possible. A unicornuate uterus appears curved and elongated, and the cervix and vagina will be visualized (Fig. 22.3B). Any rudimentary horn should be evaluated for presence of functioning endometrium, and this may be obvious in the postpubertal individual based on distention of the cavity with hyperintense blood products, indicating hematometra. Nonfunctioning endometrium will simply appear dark on T2-weighted imaging.11,12
Uterus didelphys
Uterus didelphys describes two completely separated uterine horns with two distinct cervices, an anomaly resulting from failure of the müllerian ducts to fuse in the midline by the 9th week of gestation. A complete or partial vaginal septum is present in approximately three-quarters of cases.6,11 Some patients will have a unilateral hemivaginal septum that can obstruct and cause hematometrocolpos. Interestingly, the majority of these cases are associated with renal agenesis on the same side of the obstruction.13
Bicornuate uterus
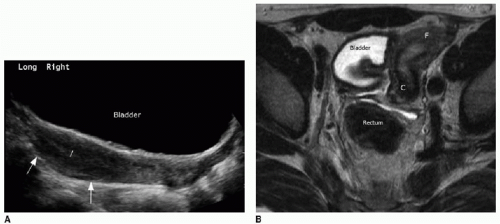
When some degree of fusion of the müllerian ducts occurs, but only partially, the result is a bicornuate uterus. The degree of separation of two distinct horns is variable and may involve complete separation through the cervical external os (referred to as bicornuate bicollis uterus) or partial separation with a septation at the uterine fundus only (termed partial bicornuate uterus). The hallmark of this disorder is communication of the two uterine cavities, even with bicornuate bicollis uterus, which distinguishes this from the didelphys uterus.6,11 On ultrasound, the anomaly can be recognized by a cleft in the external uterine fundal contour with divergent uterine horns and endometrial cavities in each horn. Using either 3D ultrasound or MR imaging, the external margins of the uterus can be readily assessed. By definition, the fundal longitudinal cleft dividing the two horns must be at least 1 cm in depth (Fig. 22.4). The depth of this cleft is an important observation, to distinguish bicornuate uterus from the septate uterus.
Septate uterus
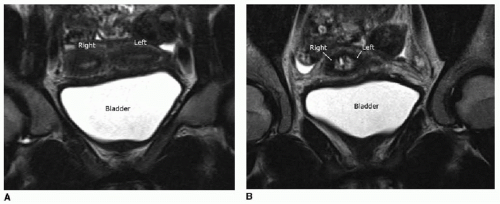
A septate uterus results from failure of the midline tissue between the two fused müllerian ducts to resorb normally by the 12th week of gestation, leaving a longitudinal midline, poorly vascularized fibrous septum through the endometrial cavity. A complete septum extends to the cervical os, whereas a partial septum does not. The external margin of the uterine fundus will be convex outward, as
with a normal uterus (Fig. 22.5). However, the endometrial cavity may appear small, and the fibrous septation may be visualized. This diagnosis predominantly impacts the adult female, as there is a high association with spontaneous abortion and preterm delivery. In the pediatric patient, this diagnosis may present clinically with signs of obstruction of one side of the uterine cavity.5,6
with a normal uterus (Fig. 22.5). However, the endometrial cavity may appear small, and the fibrous septation may be visualized. This diagnosis predominantly impacts the adult female, as there is a high association with spontaneous abortion and preterm delivery. In the pediatric patient, this diagnosis may present clinically with signs of obstruction of one side of the uterine cavity.5,6
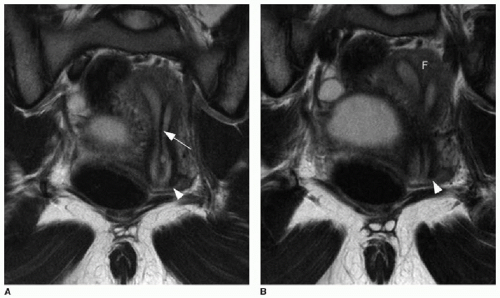 FIG. 22.5 • Septate uterus. Coronal T2-weighted images through the uterus of a 16-year-old show a septation (arrow in A) through the midline endometrial cavity to the cervix (arrowhead in A, B
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|