Physiologic |
Distention of esophagus during deglutition. |
Due to swallowing of air or belching. In contrast to adults, gas in the esophagus is a frequent finding in children. |
Hypotonia
Fig. 2.48 |
Generalized esophagus distention. |
Secondary to inflammation and gastroesophageal reflux (GER). |
GER (incompetent lower esophageal sphincter)
Fig. 2.49
Fig. 2.50 |
US or contrast examination show passage of gastric content to the esophagus. |
Physiologic up to 18 mo of age. Endoscopic Ph-measure is the gold standard for diagnosis. Imaging is essential to rule out GER secondary to gastric outlet obstruction. Is the most frequent cause of aspiration pneumonia. Roviralta syndrome: hiatal hernia secondary to hypertrophic pyloric stenosis (HPS). |
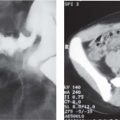
Hiatal hernia
Fig. 2.51 |
Anteroposterior X-ray: basal lucency within the outline of the cardiac silhouette.
Confirmation with contrast examination: to demonstrate GER and its sequelae (esophagitis and reflux stricture). |
Mostly congenital. Sliding hernias varying in size. DD: small epiphrenic ampulla. |
Reflux esophagitis
Fig. 2.52 |
Contrast examination: irregular and gross mucosal folds in distal esophagus with ulcerations. |
The most important cause is hiatal hernia. Endoscopy for diagnosis. |
Caustic injury |
The mucosa is initially edematous and thickened.
Later, atonic dilatation occurs, as well as irregular mucosal pattern due to necrosis.
Nonionic contrast medium for diagnosis at early stage due to perforation risk. Late sequelae: long stenosis. |
Most often with alkalis. |
Other esophagitis (mycotic, viral, bacterial) |
Spasm, pseudodiverticula ulcerations, edema, cobblestone pattern, stenosis. |
Can affect the esophagus at any level.
Usually diffuse. Immunocompromised patients. |
Foreign bodies
Fig. 2.53 |
Contrast examination: filling defects.
Foreign body impaction often at stenotic areas. |
Barium or nonionic contrast medium in cases of perforation suspicion.
Endoscopic extraction. |
Achalasia |
Atonic esophagus dilatation (megaesophagus).
Heterogeneous air-fluid level due to air and retained food. The stomach bubble is small or absent. Contrast examination: characteristic beak deformity at the distal esophagus. |
Rare in infants. Unknown cause.
Clinically: swallowing diffculty and retrosternal pain. DD: distal esophageal strictures. |
Congenital esophageal stricture |
Membranous-, hour-glass–, or tubular-shaped. |
Associated with tracheoesophageal fistula or isolated as a cartilaginous ring in bronchial remnant syndromes. |
Secondary esophageal stricture
Fig. 2.52, p. 175 |
Narrowed lumen with possible prestenotic dilatation. The contracture and scarring are more often in the middle and lower esophagus. |
Causes: Most often due to reflux esophagitis. After operative repair for esophageal atresia, at the level of the anastomosis, after caustic esophagitis (alkalis, acids), with epidermolysis bullosa; postirradiation; with vascular anomalies. |
Radiation damage |
Mural scar formation and distortion with loss of motility. The lumen is narrowed. |
Extent of the damage depends on the size of the radiation field. |
Leukemic infiltration |
Narrowing of the lumen, mostly in the distal esophagus. |
Other tumors are rare. |
Epidermolysis bullosa dystrophica |
Circumferential constriction can occur, as well as long segment strictures. |
Hereditary. Presents in infancy. Minimal trauma can result in blister production. |
Scleroderma, dermatomyositis, lupus erythematosus |
Dilatation. Absent peristalsis. |
Hiatus hernia and reflux esophagitis may develop distal stenosis. |