The History and Philosophy of Emergency Ultrasound
Stephen R. Hoffenberg
INTRODUCTION
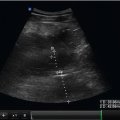
Emergency ultrasound is a standard emergency physician skill (1,2). It is taught in emergency medicine residencies (3,4), tested on board examinations (5,6), and is endorsed by emergency medicine professional societies (1,2,7). The use of ultrasound performed by the treating emergency physician, interpreted as images are displayed and immediately used for diagnosis or for procedural assistance, differs significantly from the traditional approach of consultative imaging services. Bedside emergency ultrasound has proven to be an appropriate use of technology demonstrated to speed care (8, 9, 10), enhance patient safety (11,12), and save lives (13).
THE HISTORY OF EMERGENCY ULTRASOUND
Ultrasound became available for clinical use in the 1960s following more than a decade of investigation. The technology was initially found only in specialized imaging laboratories; however, by the 1970s, ultrasound was being adopted in diverse settings by a variety of clinical specialties. Ultrasound technology and devices improved rapidly, and real-time ultrasound was developed in the early 1980s that allowed the viewing of ultrasounds without an appreciable delay between signal generation and display of the image. In addition, sufficient images were generated by real-time ultrasound to allow the visualization of continuous motion. Prior to the development of real-time ultrasound the complexity of acquiring images prevented the practical application of ultrasound for most emergency patients and was an absolute barrier to use at the bedside. Real-time scanning changed how ultrasound would be used, who would use ultrasound, and where studies would be performed.
Ultrasound devices continued to improve, and during the 1980s and 1990s, smaller, faster, and more portable ultrasound equipment was developed in accompaniment with other enhancements, such as the transvaginal transducer, multi-frequency probes, and color Doppler. These improvements accelerated the movement of technology from the ultrasound suite to the bedside for immediate use in emergency patients.
The growth in clinical applications paralleled technological advancements. As early as 1970, surgeons in Germany were the first to experiment with ultrasound for the detection of free fluid in the abdomen (14,15). In 1976, an American surgeon used ultrasound to describe and grade splenic injuries (16). Emergency physicians began investigating the clinical use of ultrasound in the late 1980s,
while the first emergency ultrasound publication appeared in 1988, which addressed the utility of echocardiography performed by emergency physicians (17). From the late 1980s through the mid 1990s significant investigation was done in both the United States and Germany on the detection of hemoperitoneum and hemopericardium in trauma victims. This research ultimately led to the description of the Focused Assessment with Sonography for Trauma or the FAST examination (13,18, 19, 20, 21, 22). The FAST examination has essentially replaced diagnostic peritoneal lavage in all but a handful of patients, and has been fully integrated into Advanced Trauma Life Support (ATLS) teaching. This examination remains the standard initial ultrasound examination for trauma victims by emergency physicians and trauma surgeons, and is often equated with “emergency ultrasonography.”
while the first emergency ultrasound publication appeared in 1988, which addressed the utility of echocardiography performed by emergency physicians (17). From the late 1980s through the mid 1990s significant investigation was done in both the United States and Germany on the detection of hemoperitoneum and hemopericardium in trauma victims. This research ultimately led to the description of the Focused Assessment with Sonography for Trauma or the FAST examination (13,18, 19, 20, 21, 22). The FAST examination has essentially replaced diagnostic peritoneal lavage in all but a handful of patients, and has been fully integrated into Advanced Trauma Life Support (ATLS) teaching. This examination remains the standard initial ultrasound examination for trauma victims by emergency physicians and trauma surgeons, and is often equated with “emergency ultrasonography.”
The American College of Emergency Physicians (ACEP) offered its initial course in the emergency applications of ultrasound in 1990. In 1991, both ACEP and the Society of Academic Emergency Medicine (SAEM) published position papers recognizing the utility of ultrasound for emergency patients (1,7). These documents endorsed not only the clinical use of ultrasound, but also ongoing research and education. The SAEM policy added that resident physicians should receive training leading to the performance and interpretation of emergency ultrasound examinations. In 1994, SAEM published the Model Curriculum for Physician Training in Emergency Ultrasonography outlining recommended training standards for emergency medicine residents (23). Shortly following the development of this curriculum, the first textbook dedicated to emergency ultrasound was published in 1995 (24).
In 2001, ACEP published the Emergency Ultrasound Guidelines more clearly defining the scope of practice and clinical indications for emergency ultrasonography (2). This policy statement advanced recommendations for credentialing, quality assurance, and the documentation of emergency ultrasounds, as well as representing current best practices and standards for ultrasound provided by emergency physicians. These guidelines were updated in 2008, reflecting the broader adoption, maturation, and expanded use of emergency ultrasound. A comprehensive approach to training, quality, documentation, and credentialing is provided in this document, as well as evidence-based additions to the list of core applications.
Over the past two decades, results of emergency physician-performed ultrasound have been examined for a wide spectrum of clinical conditions and applications, including trauma (13,18, 19, 20, 21, 22,25,26), intrauterine pregnancy (8,27, 28, 29, 30, 31), abdominal aortic aneurysm (AAA) (32, 33, 34), cardiac (13,35, 36, 37, 38, 39), biliary disease (40, 41, 42, 43), urinary tract (44, 45, 46), deep venous thrombosis (DVT) (10,47,48), soft-tissue/musculoskeletal (49, 50, 51, 52, 53, 54, 55, 56, 57, 58), thoracic (59), ocular (60, 61, 62, 63) and procedure guidance (11,12,64, 65, 66, 67, 68, 69, 70, 71, 72). Each of these is now considered a primary indication for emergency ultrasound. Ongoing research will likely establish the efficacy of additional emergency applications (Table 1.1).
GROWTH OF EMERGENCY ULTRASOUND
A number of factors have driven the development of emergency ultrasound. They include a growing recognition of the utility of ultrasound information, a need for timely access to diagnostic imaging, declining access to consultative services, improved ultrasound technology, and the endorsement of immediate ultrasound by the specialty of emergency medicine.
TABLE 1.1 Core Emergency Ultrasound Applications | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
Recognition of Ultrasound’s Value
A key factor contributing to the growth of emergency ultrasound is an increased recognition of ultrasound’s clinical utility. The primary indications for diagnostic emergency ultrasound are now well established. Where immediate ultrasound is available, it has essentially replaced invasive techniques such as peritoneal lavage and culdocentesis, as well as obviating the need for blind pericardiocentesis. Use for procedure guidance, such as central venous access, has become a standard of care in many practice settings. Interestingly, the management of cardiac arrest assisted by diagnostic ultrasound (36,39) or the evaluation of patients with nontraumatic hypotension (73,74) are examples of ultrasound usage not contemplated prior to the growth of emergency ultrasound.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree