The History of Dynamic Susceptibility Contrast Imaging: An Interview with Roland Bammer
Bruce R. Rosen
Roland: Bruce, thank you for taking the time to take this interview. What were you working on at the time when you discovered the “bolus perfusion” method?
Bruce: When you say “bolus perfusion,” I prefer to say “dynamic susceptibility contrast” or DSC, if that’s what you mean. That’s what radiologists understand by this terminology. Because some people try to measure flow from DCE [dynamic contrast enhanced] measurements and we have to give other people credit for that technology.
Roland: That’s correct. When you were working on DSC, what was your position and at what institution were you at this time?
Bruce: I had just finished my PhD and was just about to start my residency. I was a clinical and research fellow at the Massachusetts General Hospital [MGH].
Roland: Can you tell me a little bit more about how you actually got to the idea to use gadolinum or just any susceptibility agent for perfusion imaging?
Bruce: Sure. We had a new colleague in the lab, Randy Lauffer. Randy was a young chemist with expertise in the area of metal chelates that Tom Brady had hired to work in what was then the MGH NMR Center—now it is the Martinos Center—on gadolinium chelates.
My own exposure to paramagnetic ions goes back even before Randy—to work I did in my PhD thesis. My thesis was in the domain of chemical shift imaging. With my advisor, Ian Pykett, we actually did the first proton chemical shift images1,2 and amongst other things, during these early experiments, I was looking for phantoms where I could control the chemical shift of various peaks that we were seeing. Of course, sometimes I used phantom material like Miracle Whip, which was mixtures of fat and water, and you would see spectral peaks, the lipid peak and water peak, but for other experiments, based on my own physics background, I actually used materials of copper or manganese chloride solution to measure the bulk susceptibility shifts as a function of concentration. Using a cylindrical model—I had in the inner bore the metal ion and in the outerbore pure water—I could precisely control the chemical shift between the inner and outer bore by controlling the bulk susceptibility of the material. So I was using various metal ions of different concentration and bulk susceptibilities to control the chemical shift. I guess this was the first thing that taught me the notion of bulk susceptibility shifts as a function of metal ion concentration in cylindrical tubes. I was actually using them for my chemical shift experiments.
When Randy joined the lab, he was developing metal chelates as contrast agents. At that time, he was focused on gadolinium chelates for their relaxivity effects. In particular, he was interested in developing a hepatobiliary agent. The standard gadolinium DTPA was already documented.3 It wasn’t clinically approved, but it was in the literature and was a classic interstitial contrast agent. Randy was interested in developing a hepatobiliary agent and developed some compounds he thought would likely work. He was starting a series of experiments with another colleague, Sanjay Saini, who was a liver radiologist, to try to see if these contrast agents would enhance the liver selectively.
So Randy and Sanjay were doing their experiments. They were using a 1.5 Tesla small bore animal system, which, it should be noted, was a “high field” magnet for biological experiments at that time, and they came across an interesting phenomenon after they injected their agent and took a time series to watch the contrast uptake. Note that they didn’t have the rapid gradient echoes. They were taking short spin-echo images but they couldn’t get the echo times very short in those days. They had probably a 30 millisecond echo time. So the sequence was “T1 weighted” but it still had a substantial echo time. I am guessing the imaging time was approximately 1 minute.
Coming back now to the phenomenon that they discovered: while indeed their agent was a hepatobiliary agent, i.e., it did enhance the liver on subsequent images and the liver came out relatively bright, the very first image they took came out relatively darker than the original liver. So they were scratching their heads and saying, “What was going on?” The first image looked darker and then they got the brightening and T1 enhancement they were expecting. They were happy about the T1 enhancement but they were also a little confused. Puzzled by this finding, Randy presented this phenomenon to me because back then I was the only MR physicist in the lab. My thesis advisor, Ian Pykett, had at that time already left the lab to start “Advanced NMR [nuclear magnetic resonance]” (ANMR). ANMR played a role in this story and I will get to this part a little bit later in more detail. Ian started this company and developed the first human scale echo-planar imaging machine. He was a student of Sir Peter Mansfield and my thesis advisor on the chemical shift imaging project, and had the first proton chemical shift imaging paper in Radiology.1
Roland: Really, you were the only physicist in the lab at this time?
Bruce: Yes, I was the only guy who could run the MR machine and fix it, with a book. Probably, this is the only reason why I was accepted into the MGH residency program. Otherwise, they would have probably picked somebody with better medical skills, but I was at the right place at the right time.
So I was hanging around in the lab doing various experiments at that time. I was doing water and lipid saturation experiments—various things related to chemical shift imaging—and Randy brought me this interesting problem: his agent was working, except this first image was anomalously dark. He was curious if I had any thoughts and—to be honest—I don’t know what it was that put the thought in my mind that this could be a susceptibility effect, other than the fact that I have seen these images from my phantoms—the chemical shift dispersion—depending on the orientation of my phantom—between the outer water of the phantom and the air—my phantoms would show different local chemical shifts. Something about these phantom experiments from my thesis just rang a bell and I began to wonder, rather than a relaxivity effect, whether this could be a susceptibility effect from the gadolinium agent. [N.B., now we know that the darkening Bruce and Randy were seeing back then was the T2/T2* capillary blush before the contrast leaked out into the tissue where it causes T1 enhancement. It is also worth noting that the first pass susceptibility effect in tissue is much stronger than the T1 effect. This contributed to the adoption of DSC for first pass studies.]
Roland: If you say susceptibility effect, are your referring to just T2* or are you talking to—what we now call—dynamic dephasing?
Bruce: I am referring in this case to a T2 effect, but it is basically a susceptibility rather than a relaxivity effect of the contrast.
Roland: You mean you have water molecules diffusing within the microgradients of the vasculature enhanced by the susceptibility difference from the intravascular agent.
Bruce: Exactly.
Roland: Was the T2* effect that gadolinium-based contrast agents produce known at this time?
Bruce: At that time, we weren’t really doing gradient echo imaging. We were at a different station between T2* and T2. Gradient echoes came shortly thereafter but we weren’t really focused on T2* per se. We were really understanding the effect on the signal as more of a heterogenous, microscopic magnetic field rather than dipole–dipole interactions. Randy used to study relaxivity effects and dipole–dipole interaction, and what is described as outer-sphere effects. However, I thought of it as a more long-range effect, i.e., an intra/extravascular, bulk susceptibility effect rather than a molecular scale effect. This spawned the discussions I had with Randy, back and forth. He was teaching me about inner and outer sphere effects. I was teaching him about bulk susceptibility effects. It was more likely to be a bulk susceptibility effect but of course at that time it was not so clear from those initial liver scans what exactly we were seeing. So we set out to think about what the right experiments would be to try to better sort out what this phenomenon was.
This is where we had another stroke of good fortune. I had a young fellow at that time working for me by the name of Arno Villringer. You recognize his name because he is the first author on the first dynamic susceptibility paper. Arno came to the lab to work on his habilitation research from Germany. He was actually recruited to work with me on lactate imaging. At that time, I had developed—as part of my thesis—a water-suppressed proton imaging sequence and had done some initial experiments with ischemia models showing the ability to measure the elevation of lactate in ischemic brains. As you can imagine, in the early days of these experiments at 1.5T, with very early equipment, it took a lot for these experiments to work. We were making some progress, but rather slowly.
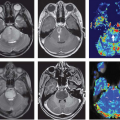
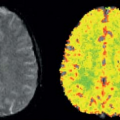
Arno was therefore looking around for other things that could also fill out his time. He was a neurologist and he was teaching me a lot about the brain. We were doing these ischemia experiments and I mentioned to him the phenomenon Randy had observed in the liver. Arno said, “Maybe we should look at the brain because the intact brain barrier is likely an interesting model.” Since we were doing these stroke models, the notion of looking at the brain seemed like a good switch. We needed a lot of time to differentiate this idea of a susceptibility effect from a relaxivity effect. So I started working with Arno to see if we could replicate this phenomenon that Sanjay and Randy had seen in the liver. That is, whether we could see the same things with injections of paramagnetic chelates also in the brain. So I picture our first experiments were in rats, normal rats. I can’t honestly recall whether we did a full 2D image experiment first. The very early experiments might be lost by now. Shortly thereafter, I knew that, I must have known because we must have done some early experiments where we saw a single image that showed a darkening, and I said, “We need higher temporal resolution.” At that time, we didn’t have gradient echo imaging and for sure we didn’t have EPI [echo-planar imaging]. I developed therefore a 1D imaging sequence where two crossing selective saturation pulses would generate what I would call spears: basically, a 1D image. I could localize my spear by selecting my cross plane through the brain (Fig. 81.1). This approach gave me a temporal resolution of 1 second and I could watch dynamic effects. Sure enough, when we did that experiment, we saw that initial bolus. At first, it was gadolinium DTPA—that’s what Randy used and provided to us; later, we used other rare earth chelates. We saw the signal drop but interestingly [because of the intact blood–brain barrier] rather than enhancing like in the liver, we
saw the signal return to the baseline (Fig. 81.2). [In the original abstract4 and paper,5 it was called bi-phasic. In fact, what Bruce and Arno observed was the recirculation.] All in the course of 10 to 12 seconds. This transient effect would have been hard to see if we had just taken a minute long image, but because we switched to this 1D imaging technique, we could image very rapidly and could actually see the entire time course and the transient toward the brain. However, we were still left with the question of whether we were showing that it was actually a susceptibility and not a relaxivity effect.
saw the signal return to the baseline (Fig. 81.2). [In the original abstract4 and paper,5 it was called bi-phasic. In fact, what Bruce and Arno observed was the recirculation.] All in the course of 10 to 12 seconds. This transient effect would have been hard to see if we had just taken a minute long image, but because we switched to this 1D imaging technique, we could image very rapidly and could actually see the entire time course and the transient toward the brain. However, we were still left with the question of whether we were showing that it was actually a susceptibility and not a relaxivity effect.
Roland: Is it correct to say that the initial signal dip was more or less discovered by chance?
Bruce: The initial dip was seen serendipitously by Randy Lauffer and Sanjay Sitai when looking at the liver. By the time we did the brain experiment, we were of course looking for it, but it was an unexpected finding by Randy and Sanjay. What I think was an important part of the story was—for the young scientists—that it did not fit the model they were looking for. Randy and Sanjay subsequently saw what they were looking for (i.e., the subsequent images in the time series showed the enhancement), but they could have just ignored that initial signal dip and declared success. However, they took the time to ask the question, “What is this?” It was not what they were interested in and they could have easily dismissed it and said, “Look, the rest of our data look great. Let’s focus on that!” Instead, they asked the question and that’s where they brought me into it. I was not interested in the liver but it was an interesting physics problem they presented to me. Randy and Sanjay were not so interested in this phenomenon because they were interested in the T1 uptake, but they were willing to teach me what they were doing and helped me understand what they observed.
Roland: When you worked with Arno Villringer on this project, you discovered that the contrast agent stays in the capillary and for the first time you observed the first pass of the contrast bolus with DSC. Was it at this stage pretty obvious to say, “Hey, let’s use indicator dilution theory to quantify perfusion!”?
Bruce: No. Definitely not. We would be jumping over an important part of the story, so I’ll slow it down just a little bit, because at that point in time we still hadn’t shown that this was a susceptibility effect. This is where Randy Lauffer comes back into the story. When I described to Randy what I thought the phenomenon was, we started talking about how we could actually prove that it was a susceptibility effect. He then began to teach me about the different lanthanide chelates and their different properties of susceptibility versus relaxivity.
I asked him, “Why gadolinium [Gd]?” and he said, “Well, very high relaxivity effects.” High relaxivity was of course what Randy was looking for, but gadolinium also has a high susceptibility effect. Then I asked, “Are there any other choices?” and he said, “Dysprosium [Dy] has an even higher susceptibility effect but a significantly smaller relaxivity effect.” of course, Randy described to me the physics behind that. Then he mentioned to me praseodymium [Pr], which had low relaxivity but also low susceptibility. Ultimately, it seemed that with the variety of the lanthanide chelates we could independently measure the changes we were seeing and see whether they scale with the known relaxivity effects (i.e.,
the dipolar relaxation) or whether they scale with the number of susceptibility effects.
the dipolar relaxation) or whether they scale with the number of susceptibility effects.
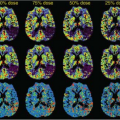
 FIGURE 81.3. The effect of different lanthanide chelates on rat brain signal intensities. An integrated signal intensity plot of a rat brain perfusion experiment is given for each agent. In each case, 1 mmol/kg of the respective agent was injected after 4 minutes of data acquisition and signal changes in time were followed for another 30 minutes. Agents used were Dy(DTPA)2−, Gd(DTPA)2−, and Pr(DTPA)2−. The same volume (1 mL) of 0.9% NaCl was injected as control. (Modified from Villringer A, Rosen BR, Belliveau JW, et al. Dynamic imaging with lanthanide chelates in normal brain: contrast due to magnetic susceptibility effects. Magn Reson Med. 1988;6:164–174.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|