(1)
Neuroradiology, Universityhospital Würzburg, Würzburg, Germany
Pediatric brain tumors, especially embryonal and other high-grade tumor types, have the propensity to disseminate along the cerebrospinal fluid (CSF) pathway, while spread outside the central nervous system (CNS) at diagnosis is very rare. The management of pediatric brain tumors has evolved over the last three decades as a result of prospective multicentric clinical trials. Multimodal treatment including surgical resection, radiotherapy, and chemotherapy has led to improved outcomes in many entities. However, treatment-related toxicity often has a major impact on long-term quality of survival. In order to reduce sequelae, the concept of stratification into risk groups according to clinical variables (e.g., age, presence of metastases detected by imaging or cytological evaluation of CSF, and postoperative residual tumor status) has been developed in the last decades, adjusting the intensity of therapy to the risk of relapse. While the principal treatment strategies have not significantly changed over the past few years, enormous progress has been made in understanding of tumor biology, which has led and most likely will continue to lead to further refinements of risk stratification and to the development of novel therapy approaches using targeted drugs in a personalized way [1].
1.1 Postoperative Residual Tumor
The aims of surgery are a maximum resection of the primary tumor with minimal damage of neurological function in order to reduce any mass effect, to debulk vital tumor tissue, to establish the biopathological diagnosis, and, if possible, to restore CSF flow. In view of the efficacy of the adjuvant treatment, a microsurgically complete resection should only be intended in case of tolerable risk, and dependent on the effectivity and risk of adjuvant treatment modalities.
To evaluate the extent of resection precisely with a low risk of artifacts, the postoperative MRI should be performed in the best technical way and timing possible. In case of significant residual tumor, particularly in nonmetastatic disease, second-look surgery should be discussed in some entities either directly after the primary operation or in the course of further treatment.
1.2 Metastases
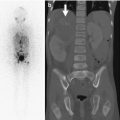
For staging, the clinical classification according to the modified Chang system [2] has been generally accepted for medulloblastoma (MB), and is used accordingly in other brain tumors. It comprises an MRI examination of the full craniospinal axis and an evaluation of lumbar CSF cytology. As immediate postoperative assessment of CSF can yield false positive results due to surgical detritus, the optimum timeframe for lumbar puncture between surgery and start of adjuvant treatment should be used. In MB, it is commonly defined by day 14 after surgery. Artifacts and clinical needs should also be considered in the timing of postoperative cranial MRI and spinal MRI. Postoperative contrast enhancement (sometimes up to a few weeks) and post-functional MRI alterations (e.g., subdural enhancement) may be difficult to distinguish from metastases or laminar meningeal disease. Therefore, spinal MRI should be performed before lumbar puncture or – in case of suspicion of MB – ideally even before tumor surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree