The Infant Spine
Tara K. Cielma
Anjum N. Bandarkar
|
OBJECTIVES
Describe the embryological development of the spine.
Define the process for sonographic evaluation of the spine.
List the clinical indications for sonographic evaluation of the spine.
Depict the normal sonographic appearance of the neonatal spinal canal and cord.
Illustrate normal variants that may simulate pathology.
Describe open and closed spinal dysraphism.
Identify the sonographic appearance of congenital anomalies of the spine.
KEY TERMS
conus medullaris
diastematomyelia
dorsal dermal sinus
filar cyst
lipomyelocele
lipomyelomeningocele
myelocele
myelomeningocele
pilonidal sinus
sacral dimple
spinal lipoma
terminal myelocystocele
tethered cord
ventriculus terminalis
GLOSSARY
cauda equina
a collection of nerve roots at the end of the spinal column; includes lower lumbar and sacral nerve roots; Latin for horse’s tail because of its appearance
a collection of nerve roots at the end of the spinal column; includes lower lumbar and sacral nerve roots; Latin for horse’s tail because of its appearance
central echo complex
the echogenic interface of the spinal cord
the echogenic interface of the spinal cord
conus medullaris
the most caudal (terminal) portion of the spinal cord
the most caudal (terminal) portion of the spinal cord
dura
outermost layer of the covering of the spinal cord
outermost layer of the covering of the spinal cord
epidural space
space between the outermost layer of the spinal cord, the dura, and the spinal column
space between the outermost layer of the spinal cord, the dura, and the spinal column
filum terminale
tapering end of the spinal cord, caudal to the conus medullaris
tapering end of the spinal cord, caudal to the conus medullaris
hydromyelia
dilatation of the central canal of the spinal cord
dilatation of the central canal of the spinal cord
low-lying cord
conus ending below the L2 to L3 disk space
conus ending below the L2 to L3 disk space
myelomalacia
softening of the spinal cord frequently caused by a lack of blood supply
softening of the spinal cord frequently caused by a lack of blood supply
simple sacral dimple
cutaneous indentation located in the midline, close to the gluteal cleft, without additional stigmata
cutaneous indentation located in the midline, close to the gluteal cleft, without additional stigmata
syrinx
fluid-filled cavity in the spinal cord
fluid-filled cavity in the spinal cord
ventriculus terminalis
cerebrospinal fluid-filled, ependyma-lined cavity within the conus medullaris
cerebrospinal fluid-filled, ependyma-lined cavity within the conus medullaris
Sonography is a useful first-line imaging tool when evaluating the spinal canal and cord in infants with suspected spinal anomalies. It is expedient and cost-effective, with no known side effects or harmful exposure to radiation. However, owing to the obvious bony nature of the spine, the utility of sonography is generally limited to infants under the age of 6 months. Other potential uses include guidance during interoperative procedures, interventional radiology, and settings in which there is an acoustic window in an older child.
Sonography is possible in infants because the posterior spinous processes are not yet ossified, thus providing an acoustic window. Sonography of the spine becomes increasingly difficult as these bones begin to ossify. Its diagnostic value decreases at 3 months, and it is nearly nondiagnostic after 6 months unless there is delayed ossification or a posterior defect of the vertebral bodies.1 Sonography can be utilized in the surgical setting through a surgically created acoustic window. Known spinal defects where the posterior spinal elements are missing can also be used as an acoustic window to image the spinal canal.
Clinical indications for spinal sonography include evaluation of spinal dysraphism and any associated mass, including meningoceles, myelomeningoceles (MMCs), lipomyelomeningoceles, and lipomas.2 Patients with lumbosacral cutaneous stigmata, including pigmented spots, hairy nevus, dermal sinuses, dimples, and hemangiomas, may be evaluated for an associated tethered spinal cord.3, 4 and 5 Sonographic evaluation readily detects spinal tumors, masses, cysts, and syrinx. Acquired lesions, such as cord birth trauma, subarachnoid and epidural hemorrhage, and epidural abscess, can also be detected in the infant.6 Intraoperative use of spinal sonography is helpful to localize intramedullary lesions, including tumors, cysts, hydrosyrinx, and vascular malformations, which may otherwise be difficult to locate by direct visualization of the cord.
SONOGRAPHIC TECHNIQUE
High-frequency linear transducers provide detailed evaluation of the spinal cord and the nerve roots. Linear or sector transducers with frequencies ranging from 8 to 15 MHz are used routinely.1,7 High-resolution hockey stick probes may be used to evaluate dimples. Sector transducers may be useful in older patients, where the acoustic window is smaller owing to progressive ossification. Dual screen images can extend the field of view to image longer sections of the spine. Panoramic views, which are now readily available on many machines, provide an extended field of view to encompass the length of the spine.7 Panoramic imaging is especially helpful when determining the level of the conus (Fig. 22-1) and its relationship to the lumbosacral junction.
To evaluate the spine, the patient should be placed in a position such that the acoustic window is optimized. The infant patient may be placed prone over a towel or pillow. This will round out the back, creating a slight kyphosis.7 A decubitus position can also be helpful because the legs can be tucked up in front of the body, increasing the splaying of the spinous processes.7 A warm blanket, bottle, or pacifier can be helpful during this examination because it will help keep the patient still.
 FIGURE 22-1 Extended field-of-view image. This feature enables the sonographer to display the full length of the spine in one image. This image displays the thoracic spine to the sacrum. |
The examination should include longitudinal and axial images from the craniocervical junction to the coccyx. The rounded surface of a curvilinear transducer will optimize imaging of the craniocervical junction.7 For the remainder of the examination, a linear transducer is placed midline, directly over the spine. An exception is made for the older child, where a parasagittal approach may diminish shadowing from the ossified spinous process.7 The level of the conus medullaris, as well as the position of the spinal cord in the spinal canal, is documented. During the examination, cord and nerve root motion should be detected and noted. Any cutaneous lesion should be documented and evaluated for associated tracts or masses.
NORMAL ANATOMY
The spinal canal and cord can be observed from the base of the skull to the tip of the coccyx. Scanning from a posterior approach, in the sagittal plane, the canal will be anechoic. The echogenic vertebral bodies and hypoechoic intervertebral disks border the length of the spinal canal anteriorly.7 Posteriorly, the canal is bordered by the hypoechoic spinous processes and the narrow echogenic epidural space. An intense linear echo, representing the arachnoid-dural layer, is seen lining the canal both anteriorly and posteriorly. Between the echogenic dura, the hypoechoic spinal cord is situated centrally to slightly anterior and is surrounded by anechoic cerebrospinal fluid (CSF) of the subarachnoid space8 (Fig. 22-2A, B). The subarachnoid space or thecal sac extends into the sacral region.
In the sagittal plane, the cord is a hypoechoic, tubular structure bordered by two echogenic, nearly parallel lines anteriorly and posteriorly and by a linear echogenic central canal8 (Fig. 22-3A). Between 1 and 3 months of age, the cervical, thoracic, and lumbar segments of the spine are 5.3 ± 0.29, 4.4 ± 0.42, and 5.8 ± 0.66, respectively.8 The spine is larger in the cervical and lumbar regions because of the number of nerves in these areas. The spinal cord tapers to a point and terminates at the conus medullaris between L1 and L2. The conus gives way to the filum terminale, which is surrounded by the echogenic strands of the cauda equina8 (Fig. 22-3B). The filum terminale can be slightly more echogenic and thicker (≤2 mm) than the surrounding nerve roots.8,9 The roots of the cauda equina form a collection of less echogenic linear strands that move freely with changes in patient positioning and with crying. The filum terminale and nerve roots extend into the distal portion of the thecal
sac. Inferior to the thecal sac, the echogenic sacral vertebral bodies are noted coursing posteriorly toward the skin surface (Fig. 22-3C). Caudal to the sacrum are two to three hypoechoic coccygeal segments. The coccyx is hypoechoic because of its cartilaginous nature (Fig. 22-3D).
sac. Inferior to the thecal sac, the echogenic sacral vertebral bodies are noted coursing posteriorly toward the skin surface (Fig. 22-3C). Caudal to the sacrum are two to three hypoechoic coccygeal segments. The coccyx is hypoechoic because of its cartilaginous nature (Fig. 22-3D).
In the axial plane, the spinal cord appears as an oval to round hypoechoic structure located within the spinal canal, with an echogenic circumferential border and echogenic dot centrally. The cord is surrounded by CSF, which is contained by the echogenic dura surrounding the canal (Fig. 22-4A). Posteriorly, the spinous process is noted centrally as a small hypoechoic circle. The echogenic vertebral arches are seen posterior and lateral on both sides of the canal. The cord diameter is larger in the cervical region, narrows through the thoracic segment, and then enlarges again near the conus. As the spinal cord tapers to the conus, the cord diameter diminishes to a small hypoechoic circle. The filum terminale appears as a slightly thicker, round, echogenic, centrally located nerve arising from the tip of the conus (Fig. 22-4B). The nerves of the cauda equina appear as smaller echogenic dots surrounding the conus and filum (Fig. 22-4C). Because of these surrounding nerves, it can be difficult to differentiate the filum from the cauda equina.8 As the thecal sac tapers distally, the sacral vertebral bodies appear as echogenic round structures in the far field, which gives way to the hypoechoic round cartilaginous bones of the coccyx just below the skin surface.
Ascertaining the exact level of the vertebral column allows determination of normal or abnormal levels of the position of the conus medullaris and exact localization of
intraspinal abnormalities. As stated previously, the spinal cord should terminate between L1 and L2. Determination, however, can be difficult.10 In the earlier reports of sonography use in the spine, methods used to determine the exact level in the spinal cord included palpation of the end of the lower ribs (said to indicate the level of L2). Another method involves determining the supracristal line by connecting the top of the palpated iliac crest (supposed to transect the L3 to L4 space). A more objective method of determining the level of the conus is to count vertebrae up from the sacrum or down from the thoracolumbar junction. Generally, there are five sacral vertebrae and five lumbar vertebrae. Starting at S5 (the last echogenic structure in the sacrum), count cephalad five vertebrae to the lumbosacral junction (LSJ) (S1/L5) and then five more vertebrae to the thoracolumbar junction (T12/L1) (Fig. 22-5). The count could be confirmed by locating T12 by following the last rib to the junction with the spine and counting the lumbar vertebrae caudally. Another way to confirm the level of the conus is to visually identify the LSJ and count upward.7 The LSJ is identified by the transition from the relatively straight line of the lumbar vertebral bodies to the gentle kyphosis of the sacrum.10 Because there can be variants in the bony anatomy, if the level of the conus is uncertain, an X-ray may be needed to confirm the level. Using sonographic guidance, a radiopaque marker can be placed on the skin, over the tip of the conus, and an X-ray of the spine obtained.11 The X-ray will confirm any variant in the bony anatomy and the level of the conus.
intraspinal abnormalities. As stated previously, the spinal cord should terminate between L1 and L2. Determination, however, can be difficult.10 In the earlier reports of sonography use in the spine, methods used to determine the exact level in the spinal cord included palpation of the end of the lower ribs (said to indicate the level of L2). Another method involves determining the supracristal line by connecting the top of the palpated iliac crest (supposed to transect the L3 to L4 space). A more objective method of determining the level of the conus is to count vertebrae up from the sacrum or down from the thoracolumbar junction. Generally, there are five sacral vertebrae and five lumbar vertebrae. Starting at S5 (the last echogenic structure in the sacrum), count cephalad five vertebrae to the lumbosacral junction (LSJ) (S1/L5) and then five more vertebrae to the thoracolumbar junction (T12/L1) (Fig. 22-5). The count could be confirmed by locating T12 by following the last rib to the junction with the spine and counting the lumbar vertebrae caudally. Another way to confirm the level of the conus is to visually identify the LSJ and count upward.7 The LSJ is identified by the transition from the relatively straight line of the lumbar vertebral bodies to the gentle kyphosis of the sacrum.10 Because there can be variants in the bony anatomy, if the level of the conus is uncertain, an X-ray may be needed to confirm the level. Using sonographic guidance, a radiopaque marker can be placed on the skin, over the tip of the conus, and an X-ray of the spine obtained.11 The X-ray will confirm any variant in the bony anatomy and the level of the conus.
Normal Variants
There are a few normal variants that can be discovered during sonography of the spine. These variants are incidental findings and have no significant clinical implications. They should be identified and documented to prevent further unnecessary testing.11
Ventriculus Terminalis
The ventriculus terminalis is a slight widening of the distal central canal. The dilated area is linear to slightly irregular and is anechoic. The widening is thought to be caused by the
incomplete resolution of the embryonic terminal ventricle and is sometimes referred to as the fifth ventricle.11,12 Typically, it disappears after the first few months of life7 (Fig. 22-6).
incomplete resolution of the embryonic terminal ventricle and is sometimes referred to as the fifth ventricle.11,12 Typically, it disappears after the first few months of life7 (Fig. 22-6).
Filar Cyst
A filar cyst is an ovoid midline anechoic structure just inferior to the tip of the conus medullaris. It is thought to be an ependyma-lined cyst that develops during embryogenesis. Some consider this the ventriculus terminalis, whereas others define it as the fifth ventricle. This structure is 8 to 10 mm long and 2 to 4 mm in the transverse diameter7,8,11 (Fig. 22-7).
CONGENITAL ANOMALIES
Spinal dysraphism refers to an array of spinal abnormalities caused by inadequate or improper fusion of the neural tube (NT) early in fetal life.13 The incidence of spinal dysraphism is 0.5 to 0.8 per case per 1,000 births.13 Most commonly, the defect occurs in the lower spine, although any part of the spine may be affected. The spectrum of spinal dysraphism can be categorized into two major groups. An Open spinal dysraphism (OSD) is characterized by neural tissue exposed without skin covering. A closed spinal dysraphism (CSD) is a skin-covered spinal abnormality. Owing to the obvious defect, open dysraphisms, like myeloceles and MMCs, are easily classified.
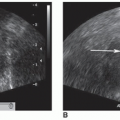
The second group, closed dysraphisms, can present with a skin-covered subcutaneous mass or various cutaneous markers. CSDs presenting with a subcutaneous mass include lipomyelocele/lipomyelomeningocele and myelocystocele. Closed dysraphisms without a subcutaneous mass-like tethered cord, spinal lipoma, diastematomyelia, or a dorsal dermal sinus (DDS) can present with various cutaneous markers that can indicate an underlying abnormality. These cutaneous markers are typically located in the midline lumbosacral region and include hair tufts, sacral dimples or pits,
pigment changes, hemangiomas, and skin tags.14, 15, 16 and 17 Nearly all of the previously mentioned anomalies are associated with a tethered cord (Fig. 22-8A-C).
pigment changes, hemangiomas, and skin tags.14, 15, 16 and 17 Nearly all of the previously mentioned anomalies are associated with a tethered cord (Fig. 22-8A-C).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree