Chapter 15 The Mediastinum
Anatomy
THE FOUR Ds OF MEDIASTINAL MASSES
Chapters 16 and 17 address focal mediastinal masses and diffuse mediastinal abnormalities.
DETECTION: MEDIASTINAL LANDMARKS
To detect a mediastinal abnormality, the radiologist must be thoroughly familiar with the normal radiographic anatomy and with the characteristic changes produced by abnormalities within various portions of the mediastinum. The radiographic landmarks of normal mediastinal anatomy are the lines, stripes, and interfaces produced when the x-ray beam passes tangential to an edge formed between tissues of different attenuations (Box 15-1).
Lines
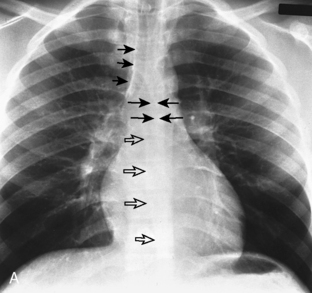
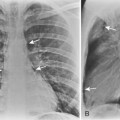
A line is a longitudinal opacity no greater than 2 mm wide. Examples include the anterior and posterior junction lines, which are formed by the close apposition of the visceral and parietal layers of pleura of both lungs as they approximate anteriorly and posteriorly to the mediastinum (Fig. 15-1). The anterior portion of the thorax begins at the thoracic inlet. The anterior junction line begins at the undersurface of the clavicles; it courses inferiorly toward the left in an oblique orientation to the level of the heart. Because the posterior portion of the thorax extends more superiorly than the anterior portion, the posterior junction line can be seen as it extends above the level of the clavicles. It frequently appears as a straight line and often projects through the tracheal air column. The anterior and posterior junction lines are not seen on all radiographic examinations. However, detection of a displaced junction line allows identification of a mediastinal abnormality and localization as anterior or posterior.
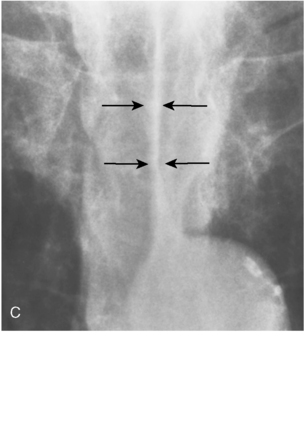
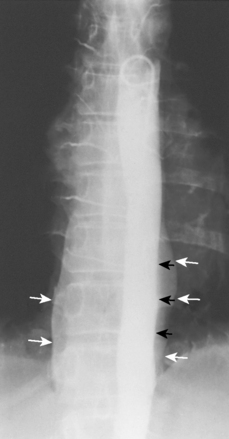
Two additional mediastinal lines are the right and left paraspinal lines, which are each about 1 mm wide. They are best seen on anteroposterior thoracic spine films. The left paraspinal line extends superiorly from the level of the aortic arch and inferiorly to the level of the diaphragm and parallels the lateral margin of the vertebral bodies. An important relationship is the one between the left paraspinal line and the descending aortic interface (see “Interfaces”). The left paraspinal line normally lies medial to the descending aortic interface. Displacement of the left paraspinal line lateral to the descending aortic interface signals the presence of a posterior mediastinal abnormality (Fig. 15-2). The right paraspinal line is less frequently visualized; when seen, it is often identified only over a portion of its course, usually between the 8th and 12th thoracic vertebral levels. Both paraspinal lines are normally straight and maintain a constant relationship with the adjacent vertebral bodies, except when displaced laterally by osteophytes. An ectatic aorta may displace the left paraspinal line laterally.
Stripes
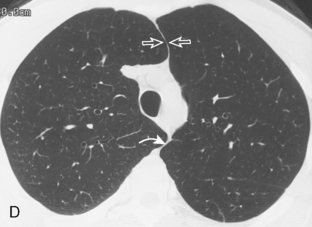
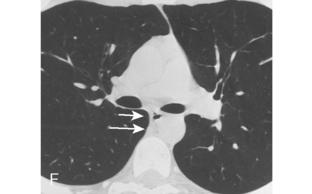
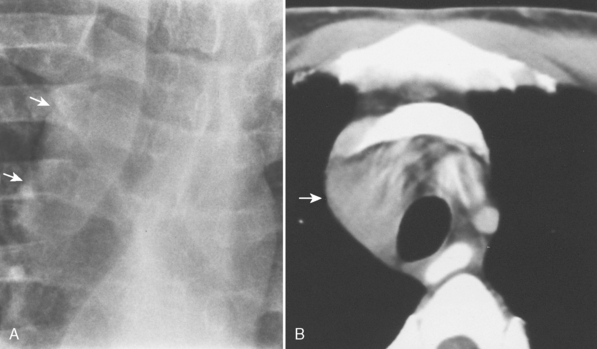
A stripe is a longitudinal composite opacity that is 2 to 5 mm wide. The right paratracheal stripe is formed by the apposition of the right upper lobe pleura and the right lateral tracheal wall. It can be identified on most chest radiographs. The normal right paratracheal stripe is identified as a smooth stripe adjacent to the right lateral border of the tracheal air column, extending inferiorly to the level of the azygous vein (see Fig. 15-1). In normal individuals, it is seen as a smooth stripe of uniform width (≤3 mm). Widening of the right paratracheal stripe is a sign of middle mediastinal pathology, such as right paratracheal lymphadenopathy (Fig. 15-3).
Interfaces
The azygoesophageal interface is formed by the juxtaposition of aerated lung within the right lower lobe or the soft tissue opacity of the right lateral margin of the azygous vein or esophagus, or both (see Fig. 15-1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree