Pleiomorphic adenoma |
US: solid, well-defined, homogeneous, hypoechoic mass ± echogenic foci, with calcification.
CT: If small, well-marginated homogeneously enhancing ovoid mass. If large, enhances inhomogeneously with foci necrosis/hemorrhage ± calcification.
MRI: depending on size, homogeneous or heterogenous low signal on T1 and high signal on T2 with mild to moderate enhancement.
NM: cold lesion. |
Third most common benign salivary gland tumor in children.
Sixty to ninety percent occur in parotid gland. Hard painless mass. |
Hemangioma
Fig. 4.166 |
US: focal/diffuse, heterogenous, hypoechoic soft-tissue mass with prominent vascular flow.
CT/MRI with contrast: diffuse CE of well-defined mass. |
Most common benign tumor of salivary gland in children.
Capillary/cavernous/hemangioendothelioma.
Identify shortly after birth with rapid growth then slow spontaneous involution. |
Lymphangioma |
US: cystic mass with thin septa ± solid elements; ± fluid-fluid levels; ± vascularization in septa or solid portions.
CT: Low-density, poorly circumscribed cystic mass that may be unior multilocular, ± fluid-fluid levels. No enhancement.
MRI: T1 hypoisointense, T2 hyperintense, no CE (unless mixed vascular component). |
Second most common salivary gland tumor in children.
Involve adjacent structures commonly (i.e., trans-spatial).
Sixty-five percent present at birth. |
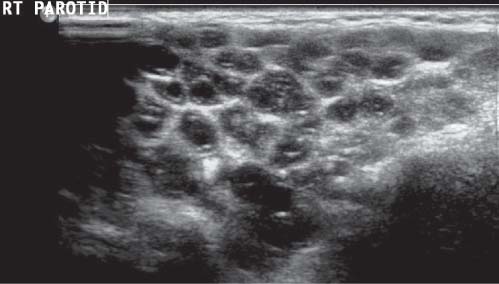
Warthin tumor (papillary cystadenoma lymphomatosum) |
US: well-defined, hypoechoic, cystic mass or masses.
CT: Solitary well-circumscribed ovoid mass with poor enhancement. Thirty percent have cystic component. No calcification.
MRI: solid/cystic lesions with minimal enhancement.
NM: hot lesion. |
Occurs only in parotid gland: superficial lobe.
Twenty percent are multiple lesions.
Ten percent are bilateral.
Most common multifocal salivary tumor. |
Mucoepidermoid carcinoma
Fig. 4.167 |
US: unifocal, heterogenous, ill-defined margins.
CT: enhancing inhomogenous mass.
MRI: heterogenous signal and heterogenous enhancement. |
Sixty percent of malignant salivary tumors are mucoepidermoid or acinic cell carcinoma.
Majority arise in parotids.
Associated with rapid growth, facial nerve paralysis, and lymphadenopathy
Low-grade: well-defined.
High-grade: ill-defined shaggy margins, invasive. |
Rhabdomyosarcoma |
Extension into glands from other sites. |
(see Tables 4.39 and 4.49 ) |
Sialectasis
Fig. 4.168
Fig. 4.169 |
US: calculi are echogenic foci with posterior shadowing. ± ductal dilatation, ± inflammation.
Sialogram: punctuate dilatation of the salivary ducts.
T2 MRI: foci of high signal intensity throughout the gland. |
Ninety percent involve submandibular gland. Majority of calculi are radiopaque and may be ductal/intraglandular. |
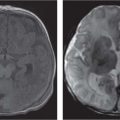
Abscess (Staphylococcus aureus)
Fig. 4.170 |
US: well-defined hypoechoic mass with surrounding edema/induration.
CECT: rim-enhancing, thick-walled cystic mass.
MRI: rim enhancement of abscess, high signal on T2. |
Local tenderness and fever. |
Ranula
Fig. 4.159, p. 392 |
US: cystic mass in floor or mouth, ± echoes and septa.
CT: thin-walled unilocular hypodense lesion with thin enhancing wall.
MRI: low signal on T1 and high signal on T2 with wall enhancement. |
Specific type of mucocele that originates in the sublingual gland—may be simple (i.e., within gland and lined by epithelium or diving ranula when simple cyst becomes large and ruptures into submandibular space creating a pseudocyst). |