The Paranasal Sinuses
Lindell R. Gentry
L.R. Gentry: Department of Radiology, University of Wisconsin Hospital and Clinics, Madison, Wisconsin 53792-3252.
Considerable progress in paranasal sinus imaging has occurred during the past decade as a result of refinements in computed tomography (CT) and magnetic resonance imaging (MRI). CT scanning has the ability to obtain thin-slice, high-resolution sectional images. CT has a higher intrinsic image contrast, whereas conventional radiography has very limited image contrast. CT scanning provides three-dimensional information, whereas conventional radiography produces two-dimensional images. For these reasons, CT scanning has largely supplanted conventional radiography for evaluation of the paranasal sinuses. This chapter attempts to incorporate all appropriate current imaging methods, emphasizing those that provide optimal information regarding a particular diagnostic problem.
CONVENTIONAL RADIOGRAPHY
Conventional (plain-film) radiography is no longer viewed as the primary diagnostic test for imaging of the paranasal sinuses. It can be helpful, however, in situations where CT scanning is not available. Conventional radiographs should be obtained with the use of close x-ray beam collimation, a suitable grid to eliminate scatter, and an appropriate film-screen combination. Ideally, the area of interest should be closest to the film to reduce unsharpness caused by magnification, and all views should be taken with the patient erect to demonstrate fluid levels. In the critically ill patient some compromises in positioning may be necessary, including the use of the supine cross-table lateral view for detection of fluid levels.1
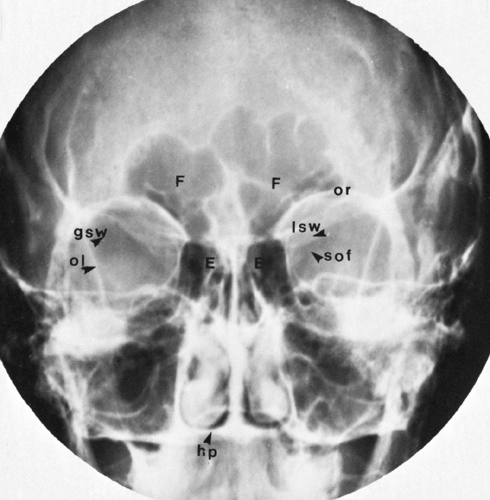
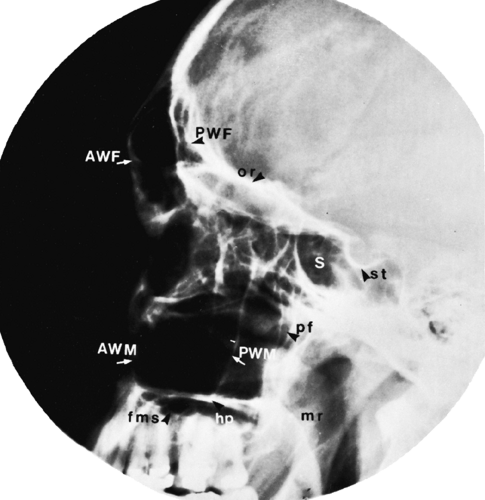
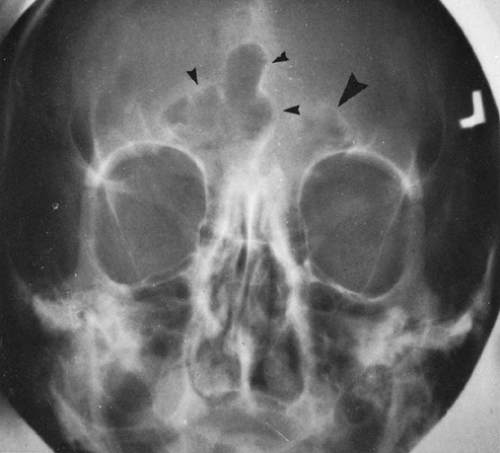
The conventional paranasal sinus examination should consist of a minimum of three views: the Caldwell (posteroanterior), Waters (occipitomental), and lateral views (Figs. 36-1, 36-2, and 36-3). The primary purpose of the Caldwell view is to visualize the frontal and ethmoid sinuses, whereas the maxillary sinuses are best demonstrated with the Waters view. In the lateral view the anterior and posterior walls of the frontal and maxillary sinuses are demonstrated, and there is a moderately unobstructed view of the sphenoid sinus.
 FIG. 36-2. Waters view. M, maxillary sinus; lwm, lateral wall of maxillary sinus; ior, inferior orbital rim; of, orbital floor; z, zygoma; za, zygomatic arch; f, frontal sinus; n, nasal bones. |
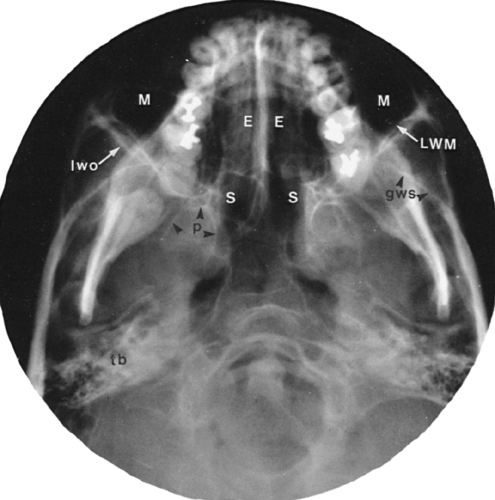
If CT is not available, additional information may be gained in problem cases with additional views, such as the submentovertical (base) view (Fig. 36-4) and the Rheese (optic foramen) views. The submentovertical view visualizes the bones of the skull base and portions of the ethmoid and sphenoid sinuses and provides an axial view of the maxillary sinuses. The Rheese view is the only conventional projection in which the posterior ethmoid cells may be seen without the superimposition of extraneous osseous structures.1
COMPUTED TOMOGRAPHY
The usual parameters for CT examination of the paranasal sinuses include a slice thickness of 3 mm, a 12- to 15-cm display field of view, 250 mA, a 1-second slice acquisition time, 120 kVp, bone and soft-tissue algorithms, and both axial and coronal sections through the entire sinuses. In some cases where the likelihood of pathology is low, only coronal scans are obtained.1
EMBRYOLOGY AND ANATOMY
The paranasal sinuses are derived from ectoderm and originate as outpouchings from the nasal cavity. All are normally paired, except for the ethmoid air cells, which are multiple.
The maxillary sinuses are the first to appear embryologically, with recognizable development evident during the fourth month of gestation. They are located inframedially with respect to the orbits in the newborn, but extend laterally and inferiorly as they pneumatize the maxillary and zygomatic bones. Maximum pneumatization is not reached until the adult configuration is achieved, at approximately 12 years of age. They reach their adult size when the last of the molar teeth erupts. The mature maxillary sinus consists of a roof, floor, and three walls: the medial, anterior, and
posterolateral. The roof and medial walls are shared with the orbit and nasal cavity, respectively, forming the orbital floor and lateral wall of the nose. Occasionally the normal maxillary sinus is compartmentalized by membranous or bony septations.
posterolateral. The roof and medial walls are shared with the orbit and nasal cavity, respectively, forming the orbital floor and lateral wall of the nose. Occasionally the normal maxillary sinus is compartmentalized by membranous or bony septations.
The ethmoid sinuses do not begin to form until the fifth month of gestation, are extremely small at birth, and do not approach adult size until puberty. Bilateral, paired ethmoid cells may range from a few to 18 or more. Ethmoid cells are anatomically divided into anterior, middle, and posterior groups according to the location of the draining ostia. Two types of ethmoid air cells may be present. The intramural types are those that remain confined to the ethmoid bone; those that invade the adjacent bones of the cranial vault or face are called the extramural type.
The frontal sinuses originate as extensions of the anterior ethmoid cells and usually are not recognizable at birth. Development accelerates after infancy but may not be complete until adulthood. Septation, hypoplasia, and aplasia are common.
The sphenoid sinuses begin to develop during the fourth intrauterine month but usually do not exceed 2 mm in diameter at birth. Pneumatization is slow until puberty but usually is completed in the young adult. Pneumatization of other portions of the sphenoid bone, especially the pterygoid processes, is common. Failure of pneumatization, resulting in a permanent infantile appearance, occurs occasionally.
All of the paranasal sinuses drain into the superior or lateral aspect of the nose. The ostia of the frontal sinuses, the maxillary sinuses, and the anterior and middle ethmoid cells drain into a depression called the hiatus semilunaris. It is located between the tip of the uncinate process and the ethmoid bulla cell in the anterior aspect of the middle meatus. The sphenoid sinuses drain into the sphenoethmoidal recess, which lies above the superior nasal concha, and the posterior ethmoid cells drain into the superior meatus. Some anatomic variability does exist. Occasionally, for example, the frontal sinuses may drain into the anterior ethmoid air cells. Certain ostia, notably the maxillary and sphenoid, appear to be poorly located physiologically. In the absence of normal mucociliary clearance, drainage of these sinuses may be incomplete, leading to accumulation of secretions and bacteria, particularly with the head in the erect or supine position.
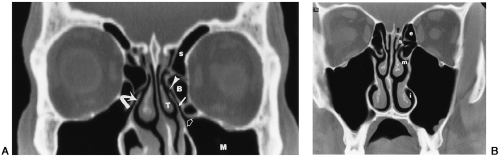
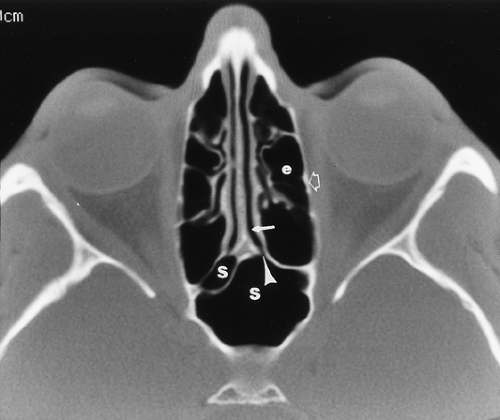
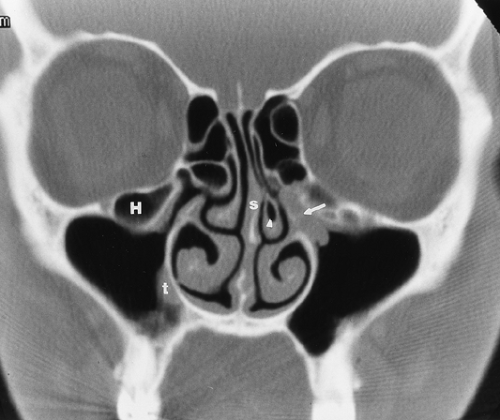
Recently, there has been a change in the concepts regarding the treatment of sinus inflammatory disease. This has resulted in a change in methods of surgery, from an open external approach to functional endoscopic sinus surgery (FESS). This approach attempts to retain the normal patterns of mucociliary clearance. FESS has led to a new anatomic concept regarding the anatomy of the frontal, maxillary, and anterior ethmoid sinus drainage. This concept is that of the osteomeatal unit (OMU). The OMU consists of the ostia of the maxillary sinus, ethmoid infundibulum, frontal recess, uncinate process, middle turbinate, and middle meatus (Figs. 36-5 and 36-6). Obstruction of the maxillary, frontal, and anterior ethmoid sinuses is usually caused by abnormalities around the OMU. These include inflammatory mucosal disease in the OMU or obstruction of the OMU by common anatomic variants such as concha bullosa, deviated nasal septum, paradoxically curved middle turbinates, and enlarged agger nasi cells.1, 4
INFLAMMATORY DISEASE
Acute inflammation of the paranasal sinuses usually is caused by a rhinovirus and commonly occurs as an accompaniment of upper respiratory tract infection. Bacterial superinfection is most often caused by Hemophilus or Streptococcus. Chronic sinusitis often develops as an aftermath of acute or recurrent sinusitis that has proved refractory to treatment; cultures most frequently yield anaerobic organisms.
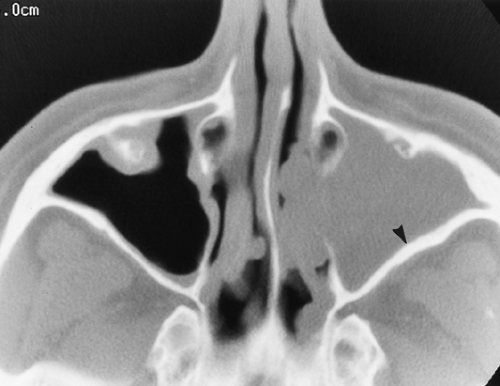
Axial and coronal CT scans usually confirm the diagnosis of sinusitis. Fluid levels, mucosal thickening, and opacification of the normally aerated sinus lumen establish the diagnosis (Fig. 36-7). Air-fluid levels with intermixed air bubbles are most often the result of accumulated secretions in patients with acute sinusitis (Fig. 36-7). Fluid levels may also occur as a result of antral lavage or bleeding after acute trauma. Prone coronal CT scans or supine axial CT scans are required for detection of air-fluid levels. Acute sinusitis may result from obstruction of the OMU by mucosal thickening (Fig. 36-8) or from anatomic obstruction by Haller cells, paradoxically curved middle turbinates, or large pneumatized middle turbinate air cells (concha bullosa) (Fig. 36-9).2,3,5,6
Mucosal thickening produces a soft-tissue opacity of variable width that follows the inner contours of the sinus walls (Fig. 36-8). An opaque sinus is an airless sinus that is filled with fluid, thickened mucosa, or a combination of both (Figs. 36-10 and 36-11).
A decrease in density of the bony sinus walls may accompany sinusitis. This usually is most apparent in the frontal sinuses when the sharp white boundary of the mucoperiosteal line is diminished (see Figs. 36-10). On plain films the thin, bony walls of the ethmoid air cells are indistinguishable in the presence of ethmoid opacification. The density of the osseous walls of the remaining sinuses may more closely approximate that of the soft-tissue contents when mucosal thickening, fluid, or opacification is present. Although these changes may indicate demineralization, they also may be artifactually produced as a result of the loss of the normal air-bone interface.
In the presence of chronic infection, the early osseous changes of demineralization may be followed by sclerosis with an apparent increase in density and an actual increase
in thickness of the sinus walls, presumably as a result of stimulation of the periosteum by the irritant effect of the sinus infection. This usually is seen in the maxillary sinuses (Fig. 36-11) but may also be apparent in the other sinuses.
in thickness of the sinus walls, presumably as a result of stimulation of the periosteum by the irritant effect of the sinus infection. This usually is seen in the maxillary sinuses (Fig. 36-11) but may also be apparent in the other sinuses.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree