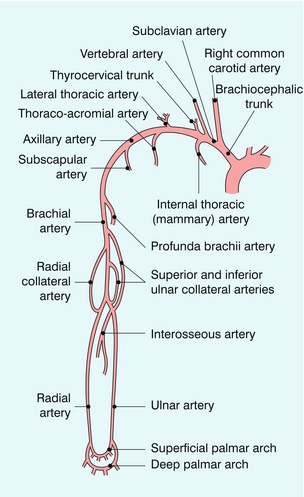
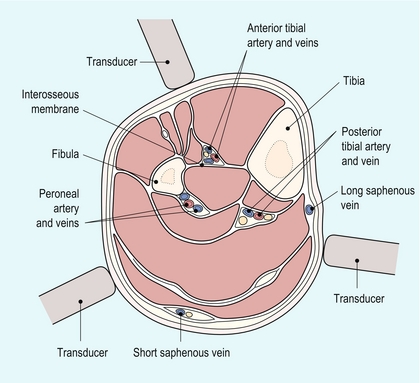
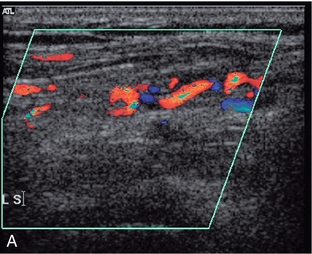
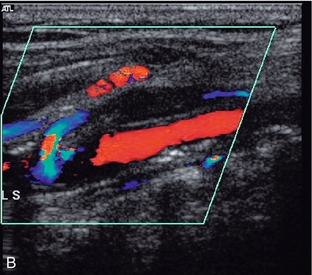
Chapter 4 Atheroma occurs to different degrees in different parts of an individual’s cardiovascular system and the lower limb arteries are particularly prone to the development of atherosclerosis. Approximately 2% of adults in late middle age in Western countries have intermittent claudication1 and each year in England and Wales around 50 000 patients are admitted to hospital with a diagnosis of peripheral arterial disease; 15 000 of these will require amputation.2 There are many factors which may influence the development of disease and, in general terms, the prevalence of peripheral vascular disease detected by non-invasive procedures is about three times greater than the prevalence of intermittent claudication.3 This chapter concentrates on the use of ultrasound in the assessment of disease in the lower limb arteries, as this is the area where most work is generated, but the value of ultrasound in the investigation of a variety of upper limb arterial disorders is also discussed. The main indications for performing Doppler ultrasound of the arteries of the upper and lower limbs are given in Box 4-1. The most common indication is the assessment of patients with ischaemic symptoms of the lower limb in order to determine if they are likely to benefit from angioplasty or a bypass graft. The ultrasound findings provide information on the extent and severity of disease; even in patients with limb-threatening ischaemia ultrasound is a useful first-line investigation that can provide the surgeon with all the information that is required for patient management. In many cases ultrasound will provide sufficient information for management decisions to be reached. In other cases, if further information is required, the subsequent magnetic resonance angiography (MRA)/computed tomography angiography (CTA)/arteriogram can be tailored appropriately. Ultrasound provides an accurate assessment of the major arteries which allows distinction between patients with significant peripheral arterial disease and those without. At the other end of the spectrum, patients with atypical symptoms that might be due to ischaemia can be examined to exclude the presence of significant arterial disease. Arteriovenous fistulae created for haemodialysis can be examined using ultrasound, allowing identification of complications associated with stenosis or occlusion, as well as estimation of blood flow through the shunt, particularly if this is thought to be inadequate or excessive (see Chapter 7). The arteries of the lower limb arise at the bifurcation of the abdominal aorta (Fig. 4-1), the common iliac arteries run down the posterior wall of the pelvis and divide into the internal and external iliac arteries in front of the sacroiliac joint. The internal iliac artery continues down into the pelvis and is difficult to demonstrate with transabdominal ultrasound, although transvaginal or transrectal scanning will show some of its branches. The external iliac artery continues around the side of the pelvis to the level of the inguinal ligament, it lies anteromedial to the psoas muscle and is normally superficial to the external iliac vein. The anterior tibial artery passes forwards through the interosseous membrane between the fibula and tibia. It then descends on the anterior margin of the membrane, deep to the extensor muscles on the anterolateral aspect of the calf (Fig. 4-2). At the ankle it passes across the front of the joint to become the dorsalis pedis artery of the foot which runs from the front of the ankle joint to the proximal end of the first intertarsal space where it gives off metatarsal branches and passes through the first intertarsal space to unite with the lateral plantar artery and form the plantar arterial arch. FIGURE 4-2 Cross-section of calf, showing major relations of calf arteries and the three main access points for demonstrating these vessels. The examination begins with the patient lying supine on the couch. The main steps in the examination are given in Box 4-2. A linear array transducer is used; usually 5–12 MHz depending on the performance of the ultrasound system and the build of the patient, lower frequencies may be required to examine the arteries in the adductor canal or in large patients. The distal external iliac/common femoral artery is located using colour Doppler as it leaves the pelvis under the inguinal ligament lateral to the femoral vein. Even if flow appears normal on colour Doppler and there is no evidence of local disease, a spectral Doppler trace should be recorded, as changes in this may indicate the presence of significant disease proximally, necessitating a careful direct examination of the iliac vessels. The bifurcation of the common femoral artery into the profunda femoris and superficial femoral arteries is then examined using colour and spectral Doppler. The profunda femoris artery should be examined over its proximal 5 cm, especially in patients with severe superficial femoral disease, in order to assess the amount of collateral flow, or its potential value as a graft origin or insertion point. 1. Colour Doppler may show the presence of collateral vessels in the muscles of the thigh (Fig. 4-3A). FIGURE 4-3 (A) Collateral vessels in the muscles of the thigh. (B) A larger collateral vessel joining the lower superficial femoral artery. 2. Collateral vessels may be seen leaving the main artery (Fig. 4-3B). 3. The character of the spectral waveform may show a change between two levels, indicating a segment of disease somewhere between the two points of measurement. The patient is then turned into a lateral decubitus position so that the medial aspect of the leg being examined is uppermost (Fig. 4-4). This position is better than the prone position as it allows access in continuity to the lower superficial femoral artery, the adductor canal area, the popliteal region and the medial calf. The region of the adductor canal must be examined with great care as it is a site where a short-segment stenosis or occlusion may be present, and this section of the vessel can be difficult to visualise as it passes deep to the thigh muscles. In some cases the use of a lower scanning frequency may help visualisation. The superficial femoral artery is examined as far down as it can be followed on the medial aspect of the thigh; the popliteal artery is then located in the popliteal fossa and followed superiorly. In difficult cases a mark can be put on the skin of the medial thigh to show the lowest segment of vessel visualised in the supine position; the popliteal artery is then followed superiorly in the decubitus position until the transducer reaches the level of the skin mark, ensuring that the vessel has been examined in continuity. The popliteal artery is then examined and followed down to the point of division into the tibioperoneal trunk and anterior tibial artery. The peroneal artery runs more deeply down the calf than the posterior tibial artery, lying closer to the posterior aspect of the tibia and the interosseous membrane. It can be examined from several approaches: firstly from a posteromedial approach similar to that used for the posterior tibial artery; secondly, it can often also be seen from the anterolateral approach used for the anterior tibial artery as it runs behind the interosseous membrane (Fig. 4-2); thirdly, a posterolateral approach may be of value in some cases. The anterior tibial artery is examined from an anterolateral approach through the extensor muscles lying between the tibia and fibula. The two bones can be identified on transverse scanning and the interosseous membrane located passing between them. The anterior tibial artery lies on the membrane and can be located using colour Doppler in either the longitudinal or transverse plane. It usually lies nearer the fibula than the tibia (Fig. 4-2). The advent of power Doppler and echo-enhancing agents has extended the role of ultrasound in the assessment of vascular disease. In the proximal lower limb and iliac vessels, the location of the vessel and confirmation of occluded segments has been made easier and, in the distal part of the leg, they make assessment of the smaller vessels of the calf and foot easier. However, more work is required to evaluate further their role.4 The subclavian arteries arise from the brachiocephalic trunk on the right (Fig. 4-5) and directly from the arch of the aorta on the left; however, there is considerable normal variation in the patterns of their origination. The origin of the right subclavian artery can be examined behind the right sternoclavicular joint, where the brachiocephalic trunk divides into the right common carotid artery and the subclavian artery. The origin of the left subclavian artery from the aortic arch cannot be demonstrated, although the more distal segments can be seen as on the right side. The subclavian artery on each side runs from its point of origin to the outer border of the first rib where it becomes the axillary artery; the subclavian vein lies in front of the artery. The main branches of the subclavian artery are the vertebral arteries, the thyrocervical trunk, the internal thoracic (mammary) artery and the costocervical trunk.
![]() The Peripheral Arteries
The Peripheral Arteries
Indications
Peripheral vascular disease
Haemodialysis Fistulae
Anatomy and Scanning Technique
ANATOMY – LOWER LIMB
SCANNING TECHNIQUE – LOWER LIMB
Common Femoral, Profunda Femoris and Superficial Femoral Arteries
The Adductor Canal and Popliteal Fossa
Calf Arteries
ANATOMY – UPPER LIMB
Radiology Key
Fastest Radiology Insight Engine