Fig. 8.1
A PD FS COR MRI indicating the presence of a PFL tear (white arrow) and an avulsion of the biceps femoris (yellow arrow)

Fig. 8.2
A PD FS COR MRI indicating a popliteus tendon (yellow arrow) and FCL tear (white arrow)

Fig. 8.3
A PD FS sagittal MRI indicating the presence of a posterior horn lateral meniscus vertical tear (yellow arrow)
After discussing all treatment options, the patient elected to proceed with surgery immediately, including an ACL reconstruction and an anatomic-based PLC reconstruction. She also consented to undergo any additional repairs or reconstructions that were deemed necessary during the exam under anesthesia and arthroscopic evaluation.
Arthroscopy
The patient was induced under anesthesia. A preoperative Doppler ultrasound showed some mild superficial blood clots, so surgery proceeded without a tourniquet. During the examination under anesthesia, a side-to-side difference of 4 cm of increased heel height in her right lower extremity was found. There was mild stiffness in her right knee, but it could be flexed back to full flexion. The Lachman and pivot shift tests were both grades 2+. The varus stress test revealed grade 3+ varus gapping at 0° and 30° of flexion. Her posterolateral drawer was positive for posterolateral instability, and the dial test showed approximately 15° of increased external tibial rotation at 30° and 90° of knee flexion. Together, the exam under anesthesia was consistent with the diagnosis made on clinical exam and diagnostic imaging.
The posterolateral surgical approach was created by making a standard laterally based hockey stick incision that extended down to the iliotibial band. After dissection over the iliotibial band and the short and long heads of the biceps femoris, the lateral capsule, distal aspect of the iliotibial band, and biceps femoris were noted all to be completely torn off of their attachments to the tibia and fibula. Careful dissection was then performed to complete a peroneal nerve neurolysis. After the neurolysis was completed, the biceps femoris was released from its scarred-in position proximally. The fibular head and the location of the normal FCL attachment to the fibula were identified. The fibular head reconstruction tunnel was reamed and a passing stitch was placed. A periosteal elevator was used to locate the popliteal sulcus. The tibial tunnel was reamed to pass the popliteus tendon and popliteofibular ligament grafts anteriorly, and a passing stitch was placed through this tunnel.
Next, the iliotibial band was split and an incision was made through the lateral capsule. The popliteus tendon (Fig. 8.4a, b) and FCL were torn at their femoral attachment sites. Guide pins were placed beginning at the native anatomic footprints and directed proximomedially to avoid passing through the intercondylar notch. After verifying correct pin placement, tunnels were reamed over the guide pins to a diameter of 9 mm and a depth of 20 mm. A split Achilles tendon graft was prepared, and 9 × 20-mm bone plugs were passed into the tunnels using two passing sutures.
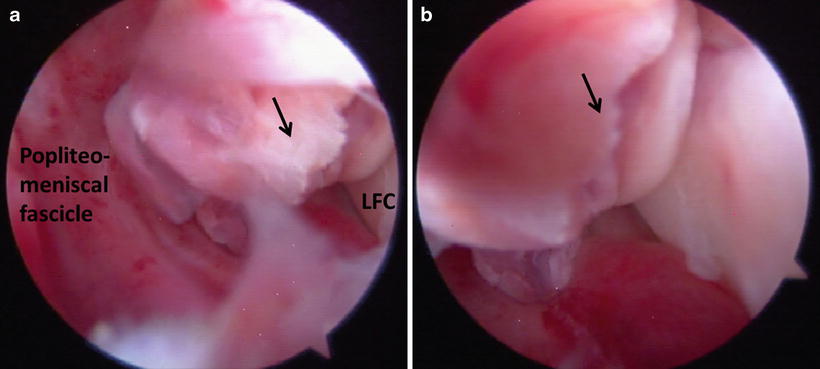
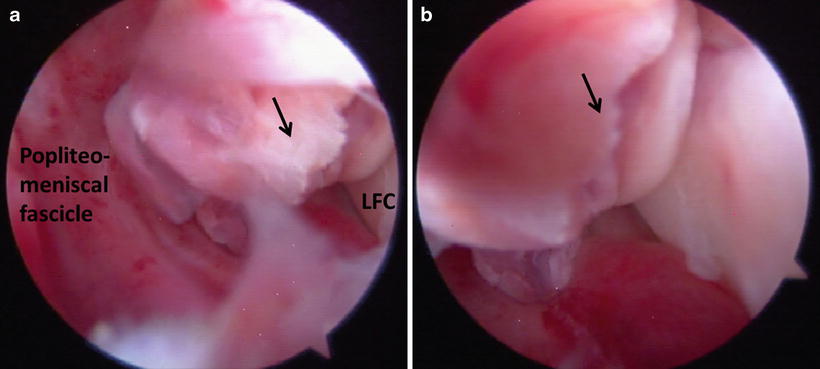
Fig. 8.4
(a, b) Arthroscopic images demonstrating the presence of a popliteus tendon tear, black arrow (right knee). LFC lateral femoral condyle
Next, the arthroscopic portion of the procedure was initiated by creating medial and lateral parapatellar arthroscopic portals. The patient’s suprapatellar pouch was hemorrhaged and removed. While the patellar articular cartilage was normal, the medial aspect of the trochlea had a large full-thickness articular cartilage defect, which was not apparent on MRI. The lesion was 10 mm medial to lateral and approximately 20 mm proximal to distal. After trimming the edges with a curette, a microfracture procedure was performed.
The medial compartment was inspected next. There was no medial compartment “drive-through” sign. The medial meniscus and tibiofemoral articular cartilage were normal. The ACL was completely torn. A 10-mm closed socket tunnel was created between the native attachment of the anteromedial and posterolateral ACL bundles on the femur. The tibial ACL attachment site was identified and outlined.
Next, the lateral compartment was inspected. The lateral meniscus was torn at its attachment to the ligament of Wrisberg and separated away from its tibial attachment (Fig. 8.5a–c). The popliteus tendon was completely torn off of its femoral attachment. A “drive-through” sign was present in the lateral compartment (Fig. 8.6) [2]. The lateral meniscus was repaired with two vertical mattress sutures. The tibial ACL reconstruction tunnel was reamed using a cruciate ligament aiming device and a 10-mm reamer. Once the ACL graft was pulled into place, it was fixed with a titanium interference screw.
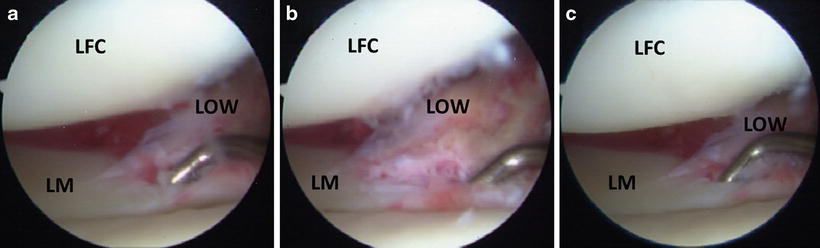
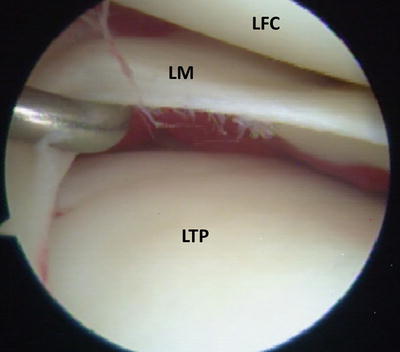
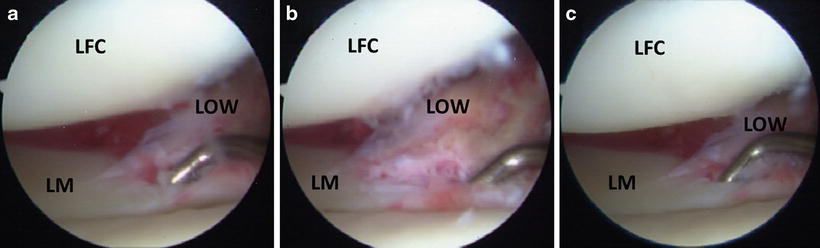
Fig. 8.5
(a, b, c) Arthroscopic images demonstrating a tear in the posterior horn of the lateral meniscus (probe) near the attachment of the ligament of Wrisberg (right knee). LFC lateral femoral condyle, LM lateral meniscus, LOW ligament of Wrisberg
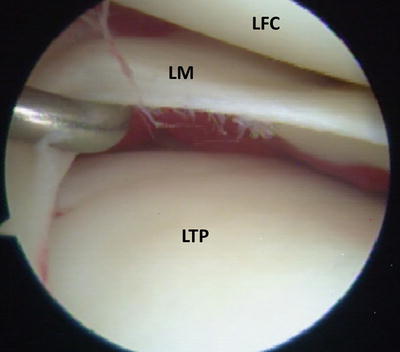
Fig. 8.6
Arthroscopic visualization of the lateral compartment indicates the presence of a “drive-through” sign, consistent with a posterolateral corner injury (right knee). LFC lateral femoral condyle, LM lateral meniscus, LTP lateral tibial plateau
The FCL and popliteus tendon grafts were passed into their respective femoral tunnels and fixed with 7 × 20-mm titanium interference screws. The popliteus tendon graft was passed down to the popliteal hiatus, and the FCL graft was passed under the superficial layer of the iliotibial band. The avulsed biceps femoris was found, and it was passed through the biceps bursa to allow for a more anatomic position of the biceps femoris once it was repaired. Once properly positioned and tensioned, the FCL graft was fixed in the fibular head with a 7 × 23-mm bioabsorbable screw. Both the popliteus tendon and FCL grafts were pulled together anteriorly through the tibial reconstruction tunnel with a passing suture, and the grafts were cycled through knee flexion and extension to eliminate any slack. Both grafts were fixed at 20° of flexion. Stability of the grafted structures was confirmed using the dial test and posterolateral drawer test.
The lateral capsule was repaired using a suture anchor to openly repair the lateral meniscus. Two anchors were placed in the fibular head, and the biceps femoris was repaired while the knee was in full extension. Finally, the ACL was fixed in the tibial tunnel with a 9 × 20-mm interference screw, which eliminated her positive Lachman’s test. The procedure was completed by closing the incisions in the lateral capsule, iliotibial band, and superficial skin.
Discussion
By combining elements of the patient’s history, physical exam, diagnostic imaging, and arthroscopy, it is possible to formulate a comprehensive understanding of complex, combined posterolateral corner injuries. In this case, the correlation between diagnostic imaging on MRI and the intraoperative findings on arthroscopy helped to identify complex injury patterns and formulate an appropriate surgical treatment plan.
The MRI demonstrated an avulsion fracture of the biceps femoris. Diagnostic MRI was also helpful in evaluating the integrity of the cruciate and collateral ligaments. With regard to the PLC, the MRI was able to discern the presence of grade III popliteus tendon and FCL injuries, both later confirmed at arthroscopy. However, due to the extended and complex nature of injuries in this patient, the injury patterns of the posterior horn lateral meniscus, peroneal nerve, and articular cartilage of the patient were difficult to determine on MRI and required further examination. In addition, a large trochlear cartilage defect was not discovered until the time of arthroscopy and was not evident on MRI.
A total PLC reconstruction, such as with this patient, is often performed in combination with other repairs and reconstructions since the majority of PLC injuries are combined injuries. Therefore, open and arthroscopic procedures may both be required to complete the requisite repairs and reconstructions for each patient. For this reason, the findings on MRI must be confirmed both through open and arthroscopic examination. In this patient, many of the repairs or reconstructions, such as the biceps femoris repair and the total PLC reconstruction, were completed through an open incision due to the extra-articular location of the structures. However, the reconstruction of the ACL and the examination of the posterior horn of the lateral meniscus, articular cartilage of the knee joint, and intra-articular popliteus tendon all required the use of arthroscopy. In cases with a wide variety of complex ligamentous, tendinous, or meniscal pathology, arthroscopy may be necessary in order to confirm the presence of articular cartilage damage or meniscal tears. Arthroscopy is also used to verify the presence of a lateral compartment “drive-through” sign, which has been described as a frequent indication of a grade III PLC corner injury [2]. The “drive-through” sign was seen in this patient, which was consistent with the MRI diagnosis of a grade III PLC injury. In addition, MRI diagnosis of the presence of bone bruises on the medial tibial plateau or medial femoral condyle may also increase suspicion of a PLC injury [4].
Case 2: ACL, FCL, Lateral Meniscus, and PFL Tear
History/Exam
A 40-year-old male presented to clinic 1 month after twisting and injuring his right knee while skiing and dropping off a 15-foot cliff. He experienced pain and swelling immediately after the injury and reported to an outside hospital where an MRI series and radiographs were obtained.
On physical exam, the patient had an obvious antalgic gait, favoring his right side. There was a moderate effusion of the right knee. Range of motion in the right knee revealed 5° of hyperextension and 120° of flexion with some pain secondary to swelling. The patient’s contralateral knee exhibited 8° of hyperextension and 130° of flexion. He had a 2+ Lachman’s test and negative posterior drawer test along with increased gapping with varus testing at 30° of knee flexion. There was no increased varus gapping at 0°. His knee was otherwise stable, with no increased gapping to valgus testing at 0° and 30° of knee flexion. The dial test demonstrated symmetric external tibial rotation at 30° and 90° of knee flexion. In light of the instability found on physical exam, imaging studies performed at an outside hospital were reviewed, and bilateral varus stress radiographs were obtained to assist with the diagnostic assessment.
Imaging
A full bilateral knee series was reviewed. Radiographs of the right knee demonstrated well-preserved medial and lateral tibiofemoral joint spaces and ruled out the presence of fractures. Varus stress radiographs demonstrated a side-to-side increase in varus gapping in the right knee compared to the left knee of 2.19 mm. An MRI performed at an outside hospital demonstrated a complete ACL midsubstance tear (Fig. 8.7), edema and discontinuity along the FCL, and a radial tear in the body of the lateral meniscus (Fig. 8.8a–c). Some changes were noted in the popliteofibular ligament, but a tear could not be definitively ruled in or out (Fig. 8.9). No articular cartilage pathology was noted.