The rapid evolution of brain imaging techniques has increasingly offered more detailed diagnostic and prognostic information about neurologic and psychiatric disorders and the structural and functional brain changes that may influence behavior. Coupled with these developments is the increasing use of neuroimages in courtrooms, where they are used as evidence in criminal cases to challenge a defendant’s competency or culpability and in civil cases to establish physical injury or toxic exposure. Several controversies exist, including the admissibility of neuroimages in legal proceedings, the reliability of expert testimony, and the appropriateness of drawing conclusions in individual cases based on the findings of research uses of imaging technology. This article reviews and discusses the current state of these issues.
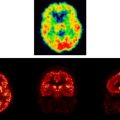
San Diego criminal defense attorney Christopher Plourd remembers well the first time he used a PET scan during a murder trial in the early 1990s. “Here was this nice color image we could enlarge, that the medical expert could point to,” Plourd said. “It documented that this guy had a rotten spot in his brain. The jury glommed onto that.”There is no doubt that imaging has revolutionized the clinical management of patients who have brain disorders, allowing the noninvasive evaluation of structural and functional abnormalities by using various standardized approaches. From the advent of computed tomography in the early 1970s to modern pulse sequences using magnetic resonance (MR) imaging, structural imaging studies allow the precise delineation of various brain lesions, improving the diagnosis and treatment of primarily neurologic disease. Similarly, measures of brain function, such as may be acquired with functional imaging techniques using MR or positron emission tomography (PET) technology, serve an increasingly important and complementary role in furthering understanding of neuropsychiatric disease and its management. Yet these technologies do not currently provide answers to all of the questions about brain functioning: research findings are not always sufficiently consistent or robust to be reliably identified in individual patient scans for routine clinical use, particularly in cases in which psychiatric disorders are at issue.
Despite these limitations, in the past few decades discussion of neuroimaging techniques has extended beyond the confines of medical offices and scientific laboratories into the legal arena. In courthouses across the United States, neuroimaging data have been introduced to establish facts about brain injury and brain malfunction. The authority of litigants to present neuroimaging evidence in court stems primarily from a 1985 decision of the US Supreme Court; in Ake v. Oklahoma , the Court held that the due process and equal protection clauses of the Constitution require “a state to provide access to a psychiatrist’s assistance” when the question of a criminal defendant’s sanity is at issue. In the years following the Ake decision, some states expanded the meaning of “psychiatrist’s assistance” to include access to neurologic tests (see, eg, ), thus opening the door for the admission of neuroimaging tests and testimony.
Rules of evidence governing expert testimony also guide the introduction of neuroimaging evidence, subject to court interpretation based on previous cases from relevant jurisdictions . Like other evidence, courts expect that neuroimages are interpreted within the bounds of acceptability within the respective scientific field, ie, using generally accepted standards within the radiologic community. These expectations, however, are not always rigorously met. Sometimes experts express conclusions based more on personal belief than on scientifically or medically supportable, evidence-based findings. Further, although scientists may interpret the significance of neuroimages within the bounds of acceptability of their respective fields, courts may derive their conclusions about the relevance and reliability of neuroimages from various sources. For these reasons, jurisdictions may develop varying admissibility standards, some of which seem to contravene traditional scientific norms about the validity of evidence.
This article assesses the current use of neuroimaging data for litigation purposes, offering a basic understanding of how brain imaging studies are introduced and evaluated in United States’ courtrooms, state and federal. The scientific, legal, and ethical complexities of using scans in such circumstances are the focus of this review. The authors primarily examine the uses of MR and PET imaging, initially reviewing the relevant techniques and their clinical and research applications in the evaluation of neuropsychiatric and behavioral disorders. We then discuss cases in which such scans have been introduced in the courtroom and the relevant legal and ethical principles that arise in such contexts.
Overview of imaging techniques relevant to legal uses
Magnetic resonance imaging
MR imaging is the primary modality for diagnosing structural brain abnormalities because of its exquisite anatomic detail, high tissue contrast, and lack of ionizing radiation. Improvements in image quality, sequence development, and device technology over the two decades since the first MR scanners arrived in hospitals and clinics have changed accepted views of the diagnostic capacity of MR imaging, and these continue to evolve. For example, lesions located at the interface between the cerebrospinal fluid and brain parenchyma are often difficult to detect and characterize on conventional or fast-spin echo T2-weighted images. Fluid-attenuated inversion recovery, or FLAIR imaging, in clinical use since 2000, has largely addressed this problem by greatly enhancing lesion conspicuity. FLAIR MR imaging offers greatly enhanced sensitivity for subcortical and periventricular lesions and thus has changed the standard of care and ability to detect abnormalities associated with multiple sclerosis, trauma, encephalitis, mesial temporal sclerosis, and mass lesions . Until recently, MR imaging using 1.5 Tesla scanners had been considered the gold standard, but high-field 3.0 Tesla scanners are becoming highly prevalent in clinical and in research centers . The higher signal-to-noise characteristics afforded by higher magnetic field strength systems, coupled with new coil technology, has improved spatial resolution and image quality while decreasing the time needed for image acquisition. MR applications with inherently low signal-to-noise ratios (eg, angiography, diffusion, perfusion, MR spectroscopy, and many functional studies) particularly benefit from 3.0-T imaging .
An important, albeit often overlooked, consideration in the interpretation of brain images is the profound and variable brain changes that occur with normal aging . Subject age is relevant in the interpretation of MR imaging, because scientists have observed extensive regional and global changes in brain volume and signal caused by “normal” aging processes. Age-related volume loss is highly variable among individuals and may be affected by coexisting medical illness. In addition to volume loss, aging is often accompanied by nonspecific foci of increased white matter signal; such losses occur with increased frequency in persons older than age 60 years . These white matter hypersensitivities have been found to correlate with an increased risk for cerebrovascular disease and hypertension, although a direct association between the hypersensitivities and cognitive changes has not been conclusively demonstrated .
Because the neuronal circuitry associated with mood regulation in humans is complex and involves multiple brain areas, imaging and analytic methods capable of identifying the functional interconnections among anatomic units are a critical focus of current research. In this context, functional MR (fMR) imaging represents the next major contribution of nuclear magnetic resonance to the study of mental disorders, by permitting investigators to identify the topologic structure of the neuronal circuitry under consideration and the relative synchrony of the neuroanatomic units involved. fMR imaging using blood oxygenation level-dependent (BOLD) contrast is frequently used to probe the study of brain function in humans. Changes in T2 ∗ signal reflective of differences in the blood oxygen content offer information on regional hemodynamic brain activity. Common research uses of BOLD entail a subtraction study design in which brain regions activated during a task or condition are identified by subtracting the stimulus scan from a baseline scan. Resulting “activation maps” generate pixel-by-pixel representations of image intensity and its correlation with the time course of the stimuli or task presentation. Because of the typically long durations of fMR imaging studies and the small signal detected, data analysis methods often require the use of motion correction and physiologic signal corrections to optimize data. Most fMR imaging methods remain in the research arena and are used primarily in between-group comparisons of subject data. The lack of standardization of analytic approaches across MR research facilities is notable .
There are, however, several MR imaging techniques reflective of functional brain measures, including brain water diffusion, cerebral blood volume, and perfusion, that have moved from the research laboratory to the clinic and for which sufficiently high sensitivity and specificity has been demonstrated to warrant diagnostic use in individual patients. Diffusion weighted (DW) imaging, which uses fast-echo planar imaging technology, is highly resistant to patient motion and far superior to conventional T2-weighted imaging for early stroke detection (within minutes to hours). DWI is widely used clinically to detect cytotoxic edema—indicative of stroke—formed in the shift of extracellular to intracellular water in ischemia, with a sensitivity and a specificity of 94% and 100%, respectively . This sequence may also be used to help differentiate arachnoid cysts (no restricted diffusion) from epidermoids (restricted diffusion) and to assess disease activity in multiple sclerosis . Perfusion MR techniques assess cerebral blood flow, cerebral blood volume, and mean transit time, to give additional information that can be used to discriminate among various pathologies that may appear structurally similar. Various approaches—T2 weighted dynamic susceptibility, T1 weighted dynamic contrast enhanced perfusion, and arterial spin labeling —may be used for various purposes to determine the extent and, together with DW imaging, potential reversibility of ischemic damage in stroke; to evaluate stroke risk in chronic cerebrovascular disease; and to assess post-treatment brain tumor viability .
Positron emission tomography
PET is a highly sensitive imaging technology capable of measuring brain physiology, including blood flow, metabolic processing (eg, glucose metabolism), and neurotransmitter function. This powerful tool has been used to study brain function in various neurologic and psychiatric conditions in which structural brain abnormalities are often not present or are observed only in the later stages of disease . Although PET has made substantial contributions to brain research over the past 20 years, there are only limited circumstances in which PET imaging has been shown to yield reliably and sufficiently high sensitivity and high specificity to warrant its use in clinical patient management.
Until recently, the US Department of Health and Human Services Health Care Financing Administration had approved a single indication for the use of brain PET and the glucose analog 18 F-fluorodeoxyglucose (FDG): presurgical evaluation of refractory seizures. Then, in June of 2004, Medicare granted approval for FDG PET in patients who have Alzheimer disease for restricted clinical settings. The limited practical applications of brain PET contrasts with the newer technology of whole-body PET imaging, for which there are numerous approved clinical uses supported by evidence of its reliability for patient diagnoses and management. PET has also been used to image brain tumors, in particular gliomas. Although CT and MR imaging provide excellent size and structural characteristics of tumors, they often cannot reliably distinguish neoplastic disease from post-treatment changes or offer prognostic information on tumor aggressivity .
Initial studies of FDG PET in head trauma cases seemed to offer promise for detecting areas of brain dysfunction for which no anatomic lesions were detected . The development and refinement of MR imaging technology from the mid-1980s to the present, however, has yielded greatly improved sensitivity for evaluating the sequelae of head trauma. Although PET remains an excellent technique for characterization of changes in brain physiology associated with head trauma or hypoxia , this body of literature remains limited . The lack of specificity of FDG PET scanning further limits its potential clinical value. For example, although the regional localization of PET findings in head trauma is variable , several studies of post-traumatic neurobehavioral syndromes have shown frontal hypometabolism (with FDG) or hypoperfusion (with 15 O-radiolabeled water) . Similar findings of reduced frontal metabolism have been reported in several other neuropsychiatric conditions, including schizophrenia, depression, and bipolar disorder (ie, manic–depressive illness) , and in violent criminals accused of murder .
As with MR imaging, PET with 15 O-water may be used to evaluate changes in perfusion associated with a specific task or stimulus-related behavior. Such work contributes greatly to understanding of the brain processes that may be common or disparate in neuropathology. Yet translation of these techniques to single-subject analyses is fraught with questions as to the sensitivity and specificity of findings, the appropriateness of the comparison subjects to which the single scan is compared, the type of spatial normalization used in the statistical comparison, and the level of statistical significance required for a finding to be deemed meaningful.
In 1996, the Brain Imaging Council of the Society of Nuclear Medicine issued a report on the “Ethical Clinical Practice of Functional Brain Imaging” . The Council’s report emphasized caution in the use of PET in forensics because of the inherent difficulty in establishing causal relationships in neuropsychiatric conditions and the limited information on the sensitivity and specificity of imaging observations and neuropsychologic parameters. Further, many local Medicare carriers and other third-party payers have classified as “investigational” the use of PET in cognitive and psychiatric disorders and in head trauma.
Having reviewed the relevant neuroimaging technology, the authors turn now to the courtroom uses of such technology in the United States. The following section examines the admission of neuroscientific evidence in criminal and civil cases to address issues ranging from competence to toxic tort injury.
Neuroimaging in the courtroom
The admission of neuroscience evidence generally turns on the court’s assessment of the reliability and relevance of that evidence, an inquiry that encompasses the robustness of the scientific technique and the expert’s ability to draw pertinent conclusions from the techniques used. Criminal lawyers use neuroimaging evidence to challenge the defendant’s competency (to stand trial, to be sentenced, to be executed), to establish the defendant’s insanity at the time of the crime, and to argue that the defendant lacked the capacity to form the mental state required for the charged crime. Neuroimages in civil lawsuits help jurors assess the damage suffered by the plaintiff; such evidence routinely can establish the fact of the plaintiff’s injuries yet is more controversial when used to argue that the defendant’s actions or product caused those injuries.
In this section, the authors first explain the standards that govern the admissibility of neuroscience evidence and then address how such evidence has been used to bolster or challenge arguments in criminal cases and in civil litigation involving physical injury and toxic torts.
Admissibility standards for scientific evidence
A jurisdiction’s rules of evidence govern the admissibility of neuroscientific images in civil and criminal trials; these rules determine which evidence the judge and jury can consider and for what purpose such evidence may be used. Each state has its own Evidence Code, and the federal courts are subject to the Federal Rules of Evidence, but generally the party introducing scientific evidence through an expert witness must establish three points before the evidence is admitted: the expertise of the witness (the expert is competent and qualified to testify regarding the matters that he or she intends to address), the reliability of the evidence (the methodology by which the expert has reached conclusions is sufficiently reliable), and the relevance of the evidence (the expert’s testimony can actually assist the judge or jury to understand the evidence or to determine a fact in issue). Because there are no constitutional or evidentiary code provisions that specifically address the use of neuroimaging evidence, trial courts admit such evidence as instructed by these basic evidentiary rules and in accordance with legal rulings from prior cases.
Expertise and reliability
The expertise of the witness concerns his or her qualifications to comment on the matter at issue. Lawyers establish expertise by asking a witness to recount his or her educational background, clinical training, scholarship, and work experience. Questions about qualifications also include familiarity with the relevant literature, participation in on-going studies, and contributions to policy debates in the relevant circles. Experts are permitted to testify only within their sphere of knowledge; testimony that lies outside the expert’s competence is excluded .
The reliability of the evidence is judged according to one of two alternative rules, depending on the jurisdiction. The dominant view, presently followed by all federal courts and most state courts, derives from the US Supreme Court’s opinion in Daubert v. Merrell Dow Pharmaceuticals, Inc . and is codified in Federal Rules of Evidence 702 . The alternative position, formulated by the District of Columbia Circuit in Frye v. United States , prevailed from 1923 until 1993 and remains effective in most of those states that have elected not to follow the federal approach (a few states have their own distinctive rules). In a court following the Frye reliability test, the party introducing the evidence must prove, by a preponderance of the evidence, that the theory or methodology used by the expert is generally accepted within the relevant scientific community. In a court following the Daubert rule, the judge personally evaluates the scientific validity of the evidence under consideration. He or she “need not weigh or choose between two legitimate but conflicting scientific views” but rather must determine that the expert’s opinion is based on scientific knowledge, rather than on guesswork or theory alone .
The Supreme Court has identified several factors to help courts determine whether scientific testimony or other technical evidence meets the Daubert standard of reliable scientific knowledge: falsifiability (whether the expert’s theory can and has been tested), peer review (whether the theory has been subject to peer review), error rate (the known or expected rate of error), and general acceptance (whether the theory or methodology used is generally accepted within the relevant scientific community). These factors are not exhaustive, because courts can consider other measures and facts in their analysis of reliability . Other facts may include whether the field of expertise claimed by the expert is known generally to reach reliable results (eg, astrology or necromancy does not qualify as reliable science), whether the expert has adequately accounted for obvious alternative explanations, whether the expert’s opinions were developed expressly for the purpose of litigation, whether the expert’s fee has compromised his or her precision, whether the expert has extrapolated from an accepted premise to an unfounded conclusion, and whether the expert has properly applied accepted principles and methods to the facts of the case .
Finally, when an expert offers into evidence a professional, scientific opinion, he or she may rely on neuropsychologic and medical tests he or she personally performed and on tests performed by others, as long as those tests and the formulae used to assess the data from those tests meet the jurisdiction’s reliability standard . An expert may also base his or her professional opinion on sources of background information (such as statements from the patient or other witnesses), police reports, and hospital records . A judge, however, may exclude mention of otherwise inadmissible evidence procured outside the four corners of the courtroom if he or she predicts that the probative value of this evidence is outweighed by its capacity to prejudice or confuse the jury, or to unnecessarily delay the trial .
A survey of recent cases from state and federal jurisdictions suggests that courts typically regard PET scans, MR images, and electroencephalography (EEG) as valid, reliable devices to document the existence of brain structures and to measure the performance of neurologic functions . In fact, in many cases the admission of neuroimaging evidence to establish encephalopathy seems entirely noncontroversial; the case opinions mention the evidence but do not explicitly discuss the reliability of the procedures for the purposes sought . Two cases are notable for their contrary outcomes; in both cases lawyers attempted to use neuroimaging evidence for novel purposes. In In re Welding Fume Products Liability Litigation , the district court, citing recent neuroscience literature, declared that PET scans are not reliable differential diagnostic devices for Parkinson disease; in Jackson v. Calderon , the court stated that PET scans are not generally accepted tools to diagnose chronic PCP abuse.
Documenting the presence of structure or function is not enough to establish the abnormality of that structure or function, however; the expert’s conclusion about abnormality must be supported by reliable scientific methodology . Attorneys thus have encountered problems when the expert’s opinion about abnormality stems from comparison with improper control groups or in situations in which no baseline measures exist . In many imaging research studies, a normative comparison image is obtained by pooling and spatially normalizing brain images of “normal” or healthy control subjects. Questions then arise as to the size and inclusion/exclusion criteria of the control group. Age, gender, handedness, sensory and neuropsychologic state, and other such details may be relevant to the appropriateness of a group to serve as a control or comparison cohort . Furthermore, the expert must establish, through reliable scientific methods, the etiology of the observed abnormality and the implications of that abnormality for the patient’s behavior . Because the brain demonstrates elasticity, a functional image taken at a certain time or under certain conditions may not be similar to an image at a different point in time, although both depict normal brain functioning. Additionally, there is widespread disagreement about the degree to which one can predict behavior from neuroimage findings . Conflicting or confirming interpretations of the cause of the observed abnormality or its behavioral implications may come from other diagnostic studies, including personality tests, and from clinical interviews .
In Huber v. JLG Industries, Inc. , the plaintiff fell while operating a lift designed by the defendant and thereafter developed a partial seizure disorder. His medical expert testified that the fall caused his disorder. She supported this conclusion by pointing to EEG scans of the plaintiff’s brain (which showed intermittent left mid-temporal spikes, a finding consistent with partial seizure disorder), the plaintiff’s previous seizure-free history, and the signs of visible head injury at the time of the fall. The court held that the doctor’s conclusion was reliable because it was based on reliable principles and methods, including her specialty in seizure disorders, her treatment relationship with the plaintiff, and her reliance on brain data from EEG and MR imaging.
In California v. Holt , a defendant who was convicted of capital murder introduced evidence of congenital brain damage in the penalty phase of his trial, in an effort to mitigate the seriousness of his offense. One defense expert testified that EEG and PET scan results showed Holt’s temporal lobes and part of his frontal lobe were “two standard deviations below normal” and that “emotional system damage” existed in the cingulate gyrus portion of his brain, injuries consistent with malfunctioning cognition, judgment, planning, execution, judgment, impulse-control, and sexual behavior (Id. at 231). A second defense expert testified that an EEG he performed on the defendant showed “an unusual amount of alpha wave activity in the front of defendant’s brain, and a relative lack of activity in the side and back,” a pattern consistent with a high degree of violent, impulsive, aggressive behavior (Id.). A third expert conducted clinical interviews with the defendant and read his medical reports before concluding that Holt had epilepsy. All three doctors pointed to lack of oxygen during birth as the principal cause of this brain damage. The court accepted the defense’s neuroscience evidence as reliable but ultimately concluded that death was the appropriate sentence for Holt, given the severity of his crimes.
Although these cases demonstrate courts’ acceptance of neuroscience evidence, in other matters reliability has proven to be a major obstacle for the party seeking to introduce scientific evidence. In Craig v. Oakwood Hospital , plaintiff Craig sued the hospital and doctor who assisted his mother in childbirth, claiming that improper doses of Pitocin administered during labor caused him trauma during birth and that this trauma resulted in cerebral palsy and other lifelong injuries. An MR imaging examination showed that the plaintiff’s brain tissue had developed asymmetrically, according to the plaintiff’s medical expert. The doctor, however, never explained how this asymmetric development related to either the trauma of the birth or the specific neurologic conditions presently displayed by the plaintiff. Although the court accepted the MR images as reliable proof of asymmetry, it held that the plaintiff had failed to prove that the expert’s opinion about the cause and implications of his injuries was sufficiently reliable to constitute evidence.
In U.S. v. Gigante , organized crime figure Gigante was charged with racketeering, extortion, and conspiracy to commit murder. Gigante contended that he was incompetent to stand trial because of mental illness, including schizophrenia and dementia. A PET scan showed bilateral parietal hypometabolism, characteristic of Alzheimer disease, although Gigante was taking psychotropic medications at the time of the scan. Because these drugs might have corrupted the test’s reliability, because the control group members differed from the defendant in age and background, and because Gigante had a history of malingering, the court found the expert’s conclusions unreliable and declared Gigante competent to stand trial.
Likewise, the court in Penney v. Praxair, Inc . refused to allow a plaintiff to substantiate his claim of traumatic brain injury with PET scan evidence. The court cited two major reasons for denying the plaintiff’s request. First, although Penney was 66 years old at the time of the PET scan, the doctors compared his scan results to a control group consisting of people ranging in age from 18 to 70 years. Second, the plaintiff was taking medication for a heart condition and other ailments at the time of the scan, which could have influenced the study’s result. For these reasons, the court held that the expert’s conclusions about abnormalities he observed in Penney’s brain images were not reliable.
Relevant issues addressed by neuroscientific images
A court admits reliable neuroimaging evidence only if it helps the trier of fact to understand an issue in the case or if it makes a fact at issue more likely true or false . Once a piece of evidence is found to be relevant, it is usually admissible in court, with some exceptions . For example, relevant evidence (such as a neuroimage) could be excluded if its probative value is substantially outweighed by its tendency to cause unfair prejudice, to confuse the issues, or to mislead the jury, or by considerations of undue delay, waste of time, or needless presentation of cumulative evidence . In addition to passing the reliability test set forth in the jurisdiction, the party seeking to use neuroimages must therefore also convince the court that such evidence is relevant and not unduly prejudicial or confusing.
Courts recognize that the state of mind, mental abilities, and cognitive capacity of a defendant can affect his or her criminal prosecution and punishment. In criminal trials, four theories of relevance are available to the attorney seeking to introduce neuroimages: competence, insanity, mental state, and mitigation. A defendant who is presently incompetent cannot be tried, sentenced, or executed, although he may be forced to take medication that renders him competent to undergo those procedures. A defendant who, at the time of the crime, was either insane or lacked the ability to form the requisite mental state cannot be convicted of the crime. Finally, a defendant who has been convicted of a crime may introduce neuroscience evidence during his sentencing hearing to argue that his encephalopathy reduces his ability to make rational choices and therefore renders him less responsible as a criminal actor and more deserving of leniency.
Competence refers to the defendant’s ability to participate meaningfully in his trial. A defendant who, because of mental disease or defect, is incapable of contributing to his own defense or of understanding the nature of the proceedings against him is considered incompetent to stand trial . The same rules apply to sentencing, execution, and acceptance of the defendant’s guilty plea . Because savvy defendants may try to feign incompetence to avoid prosecution, defense counsel must establish their clients’ incompetence in an evidentiary hearing. Competence hearings typically involve testimony from medical or mental health experts who have examined the defendant and reports prepared in advance that document the defendant’s mental functioning . Consistent with this evidentiary showing, courts accept expert interpretations of neuroimages that document brain damage likely to affect the defendant’s ability to understand the proceedings and to make meaningful decisions as to waiver of rights or defense strategy ; neuroimages also may help clarify whether the defendant is malingering .
The defense of insanity and the mental state argument both address the defendant’s state of mind at the time of the crime, rather than at the time of the prosecution. The former—insanity—is an affirmative defense, which means that to prevail the defendant must persuade the jury that, because of a mental disease or defect, he was unable to appreciate the nature, quality, and wrongfulness of his acts at the time of the crime. The latter is by contrast a direct challenge to the prosecution’s burden of proof on the mental state element of the crime; because the prosecution must prove each element of the crime beyond a reasonable doubt, to prevail, a defendant need only create a reasonable doubt about his capacity to form the mental state necessary to commit the crime. For a thorough discussion of the difference between the insanity argument and the mental state argument, see . As to mental state and insanity, medical experts must be able to testify that the brain damage they witness on a current neuroimaging scan not only existed at the time of the crime but also prevented the defendant from forming the requisite intent to commit the crime . Defendants generally have not been successful in their efforts to convince courts that brain abnormalities, even where observable on PET scans and MR imagess, prevented them from having the capacity to deceive, to premeditate, or to form a murderous intent .
For example, in People of New York v. Weinstein , the defendant claimed that he lacked criminal responsibility for murder because of a mental disease. The defense introduced an MR image that showed an arachnoid cyst on the defendant’s brain, a common and benign developmental anomaly. A PET scan confirmed these findings and further demonstrated regional hypometabolism. Based on these findings, the defendant argued that his brain abnormalities reduced his responsibility for violent behavior. The only piece of research supporting the defendant’s claims, however, was a study involving only four subjects, and the author of the study clearly mentioned that further investigation was necessary to establish that hypometabolism in the frontal lobe causes violence. Experts also admitted that arachnoid cysts are commonly found in people who are not violent. For these reasons, the court held that a causal link between the defendant’s violent behavior and his brain abnormalities had not been substantiated, and the defendant was not allowed to argue that these abnormalities were relevant to his criminal conduct.
When neuroimages are offered during the sentencing phase of a criminal case, they help the defense argue for mitigation. That is, to encourage the court to understand why the defendant acted as he did, defense counsel seeks to establish a physiologic explanation for unwarranted aggression, inappropriate sexuality, poor judgment, and the like. Physiology is thus presented as the antithesis of choice, the foundation on which most formulations of criminal responsibility rest. For example, in the penalty phase of Henry Marshall’s murder trial, a medical expert pointed to MR imaging results showing that the “decision-making area” of the defendant’s brain had shrunk significantly, that the folds in his brain were more pronounced than normal, and that his brain had atrophied; an EEG showed that his brain’s electrical activity occurred at a lower than normal frequency, and a single-photon emission tomography (SPECT) scan showed abnormal blood flow to the brain. The doctor then testified that, because of this brain damage, the defendant would be worse at understanding, comprehending, remembering, and decision-making than most other people . Likewise, experts for murderer Eddie Lee Sexton testified in his penalty phase that a dysfunctional limbic system in the lower half of the defendant’s brain (revealed by a PET scan) and structural injury to the top half of the brain (visible in MR imaging results) rendered the defendant incapable of responding normally to emotional situations, of handling stress, and of linking past, present, and future . Neither of these arguments proved persuasive to the courts and juries evaluating the evidence.
Although criminal courts use neuroimaging evidence to examine the defendant’s mental functioning, civil courts consider such evidence relevant to establishing the existence of the plaintiff’s alleged injuries. For example, in Siharath v. Sandoz Pharmaceuticals Corp. , doctors used MR imaging to diagnose and to identify brain hemorrhages in two women who had taken a drug manufactured by the defendant. Likewise, the court in In re Welding Fume Products Liability Litigation discussed the usefulness of MR imaging for revealing “where manganese accumulates in the brain”; a PET scan was used for the same purpose in Hose v. Chicago Northwestern Transportation Company . Further, MR imaging has been used to establish asymmetry in the brain’s development and to identify signs of a seizure disorder . In some cases, experts rely on neuroscience evidence to rule out alternative diagnoses. For example, in City of Owensboro v. Adams , the employer claimed multiple sclerosis, rather than workplace injury, was responsible for the claimant’s observable symptoms; the claimant’s expert pointed to MR imaging (and other evidence) to explain his conclusion that multiple sclerosis was not possible. The plaintiff’s expert in Hose v. Chicago Northwestern Transportation Company used a PET scan for a similar purpose—to rule out alternative diagnoses such as Alzheimer disease, stroke, and alcoholism, as the cause of the plaintiff’s observable encephalopathy.
In sum, neuroimaging evidence has become an increasingly important tool of proof in criminal and civil cases in the United States. Although subject to the constraints of reliability and relevance, results of neuroimaging scans can and do help courts to understand the nature, causes, and behavioral implications of injuries to the brain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree