The Role of the Orthopedic Radiologist
Spectacular progress has been made and continues to be made in the field of radiologic imaging. The introduction and constant improvements of new imaging modalities—computed tomography (CT) and its spiral (helical) and 3D variants, 64-channel multidetector row CT (MDCT), high resolution flat-panel volume computed tomography (fpVCT), 3D CT-angiography, digital (computed) radiography (DR or CR) and its variants: digital subtraction radiography (DSR) and digital subtraction angiography (DSA), 3D ultrasound (US), radionuclide angiography and perfusion scintigraphy, positron emission tomography (PET), PET-CT, and PET-MRI, single-photon emission computerized tomography (SPECT), magnetic resonance imaging (MRI) and its 3D variant, 3D MRI/CT fusion imaging, MR-arthrography (MRa), and MR-angiography (MRA). Among others—have expanded the armamentarium of the radiologist, facilitating the sometimes difficult process of diagnosis. These new technologic developments have also brought disadvantages. They have contributed to a dramatic increase in the cost of medical care and have often led clinicians, trying to keep up with new imaging modalities, to order too many frequently unnecessary radiologic examinations.
This situation has served to emphasize the crucial importance of the role of the orthopedic radiologist and the place of conventional radiography. The radiologist must not only comply with prerequisites for various examinations but also, more importantly, screen them to choose only those procedures that will lead to the correct diagnosis and proper evaluation of a given disorder. To this end, radiologists should bear in mind the following objectives in the performance of their role:
To diagnose an unknown disorder, preferably by using standard projections along with the special views and techniques obtainable in conventional radiography before using the more sophisticated modalities now available.
To perform examinations in the proper sequence and to know what should be performed next in the radiologic investigation.
To demonstrate the determining imaging features of a known disorder, the distribution of a lesion in the skeleton, and its location in the bone.
To monitor the progress of therapy and possible complications.
To be aware of what specific information is important to the orthopedic surgeon.
To recognize the limits of noninvasive radiologic investigation and to know when to proceed with invasive techniques.
To recognize lesions that require biopsy and those that do not (the “don’t touch” lesions).
To assume a more active role in therapeutic management, such as performing an embolization procedure, delivering chemotherapeutic material by means of selective catheterization, or performing (usually CT-guided) radiofrequency thermal ablation of osseous lesions (such as osteoid osteoma).
The radiologic diagnosis of many bone and joint disorders cannot be made solely on the basis of particular recognizable radiographic patterns. Clinical data, such as the patient’s age, gender, symptoms, history, and laboratory findings, are also important to the radiologist in correctly interpreting an imaging study. Occasionally, clinical information is so typical of a certain disorder that it alone may suffice as the basis for diagnosis. Bone pain in a young person that is characteristically most severe at night and is promptly relieved by salicylates, for example, is so highly suggestive of osteoid osteoma that often the radiologist’s only task is finding the lesion. However, in many cases clinical data do not suffice and may even be misleading.
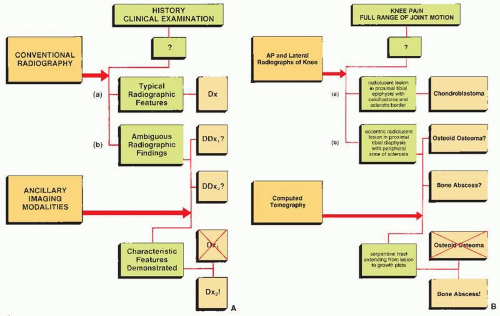
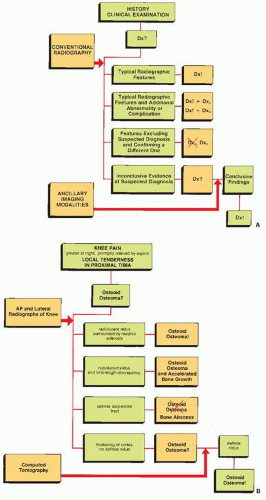
When presented with a patient, the cause of whose symptom is unknown (Fig. 1.1) or suspected on the basis of clinical data (Fig. 1.2), the radiologist should avoid, as a point of departure in the examination, the more technologically advanced imaging modalities in favor of making a diagnosis, whenever possible, on the basis of simple conventional radiographs. This approach is essential not only to maintain cost-effectiveness but also to decrease the amount of radiation to which a patient is exposed. Proceeding first with conventional technique also has a firm basis in the chemistry and physiology of bone. The calcium apatite crystal, one of the mineral constituents of bone, is an intrinsic contrast agent that gives skeletal radiology a great advantage over other radiologic subspecialties and makes information on bone production and destruction readily available through conventional radiography. Simple observation of changes in the shape or density of normal bone, for example in the vertebrae, can be a deciding factor in arriving at a specific diagnosis (Figs. 1.3 and 1.4).
To aid the radiologist in the analysis of radiographic patterns and signs, some of which may be pathognomonic and others nonspecific, a number of options within the confines of conventional radiography are available. Certain ways of positioning the patient when radiographs are obtained allow the radiologist the opportunity to evaluate
otherwise hidden anatomic sites and to more suitably demonstrate a particular abnormality. The frog-lateral projection of the hip, for example, is better than the anteroposterior view for imaging the signs of suspected osteonecrosis (ON) of the femoral head by more readily demonstrating the crescent sign, the early radiographic feature of this condition (see Figs. 4.59 and 4.60B). The frog-lateral view is also extremely helpful in the early diagnosis of slipped femoral capital epiphysis (see Fig. 32.30B). Likewise, the application of special techniques can help to identify a lesion that is difficult to detect on routine radiographs. Fractures of complex structures such as the elbow, wrist, ankle, and foot are not always demonstrated on the standard projections. Because of the overlap of bones on the lateral view of the elbow, for example, detecting a nondisplaced or minimally displaced fracture of the radial head occasionally requires a special 45-degree angle view (called the radial head-capitellum view) that projects the radial head free of adjacent structures, making an otherwise obscure lesion evident (see Figs. 6.12 and 6.28). Stress radiographic views are similarly useful, particularly in evaluating tears of various ligaments of the knee and ankle joints (see Figs. 9.16, 9.74B, 10.10, and 10.11).
otherwise hidden anatomic sites and to more suitably demonstrate a particular abnormality. The frog-lateral projection of the hip, for example, is better than the anteroposterior view for imaging the signs of suspected osteonecrosis (ON) of the femoral head by more readily demonstrating the crescent sign, the early radiographic feature of this condition (see Figs. 4.59 and 4.60B). The frog-lateral view is also extremely helpful in the early diagnosis of slipped femoral capital epiphysis (see Fig. 32.30B). Likewise, the application of special techniques can help to identify a lesion that is difficult to detect on routine radiographs. Fractures of complex structures such as the elbow, wrist, ankle, and foot are not always demonstrated on the standard projections. Because of the overlap of bones on the lateral view of the elbow, for example, detecting a nondisplaced or minimally displaced fracture of the radial head occasionally requires a special 45-degree angle view (called the radial head-capitellum view) that projects the radial head free of adjacent structures, making an otherwise obscure lesion evident (see Figs. 6.12 and 6.28). Stress radiographic views are similarly useful, particularly in evaluating tears of various ligaments of the knee and ankle joints (see Figs. 9.16, 9.74B, 10.10, and 10.11).
An accurate diagnosis depends on the radiologist’s acute observations and careful analysis, in light of clinical information, of the radiographic findings regarding the size, shape, configuration, and density of a lesion; its location within the bone; and its distribution in the skeletal system. Until the conventional approach with its range of options fails to provide the radiographic findings necessary for correct diagnosis and precise evaluation of an abnormality, the radiologist need not turn to more costly procedures.
Knowing the proper sequence of procedures in radiologic investigation depends, to a great extent, on the pertinent clinical information provided by the referring physician. The choice of modality or modalities for imaging a lesion or investigating a pathologic process is dictated by the clinical presentation as well as by the equipment availability, physician expertise, cost, and individual patient restrictions. Knowing where to begin and what to do next, as rudimentary as it may sound, is of paramount importance in reaching a precise diagnosis by the shortest possible route, with the least expense and detriment to the patient. Redundant studies should be avoided. For example, if a patient presents with arthritis and if clinician is interested in demonstrating the distribution of “silent” sites of the disorder, the radiologist should not begin by obtaining radiographs of every joint (a so-called joint survey). It is instead more sensible to perform a skeletal scintigraphy and, afterward, to order radiographs of only those areas that show increased uptake of radiopharmaceutical. A simple radionuclide bone scan rather than a broad-ranging bone survey is also a reasonable starting point for investigating other possible sites of involvement when a lesion is detected in a single bone and is suspected of representing part of a multifocal or systemic disorder, such as polyostotic fibrous dysplasia or metastatic disease. Similarly, if a patient is suspected of having osteoid osteoma around the hip joint and standard radiography has not demonstrated the nidus, a radionuclide bone scan should be performed next to determine the site of the lesion. This should be followed up
by CT for more precise localization of a nidus in the bone. However, if the routine examination demonstrates the nidus, scintigraphy can be omitted from the sequence of examination. At this point, only CT scan is required to determine the lesion’s exact location in the bone and to obtain specific measurements of the nidus (Fig. 1.5; see also Fig. 17.10). If ON of the femoral head is suspected and the radiographs are normal, MRI should be ordered as the next diagnostic procedure, because it is a more sensitive modality than CT, or scintigraphy. The text that follows presents many similar situations in which the proper sequence of imaging modalities may dramatically shorten the diagnostic investigation.
by CT for more precise localization of a nidus in the bone. However, if the routine examination demonstrates the nidus, scintigraphy can be omitted from the sequence of examination. At this point, only CT scan is required to determine the lesion’s exact location in the bone and to obtain specific measurements of the nidus (Fig. 1.5; see also Fig. 17.10). If ON of the femoral head is suspected and the radiographs are normal, MRI should be ordered as the next diagnostic procedure, because it is a more sensitive modality than CT, or scintigraphy. The text that follows presents many similar situations in which the proper sequence of imaging modalities may dramatically shorten the diagnostic investigation.
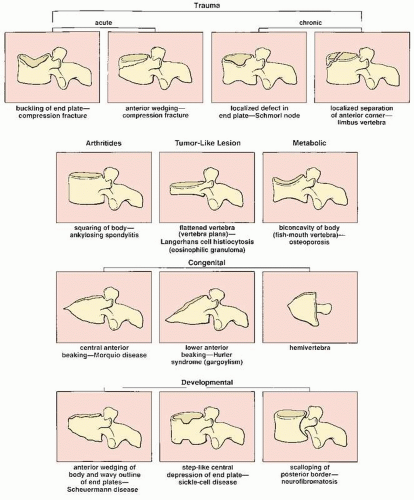 FIGURE 1.3 Shape and contour of bone. Observation of changes in the shape and contour of a vertebral body on conventional radiographs may disclose critical information leading to a correct diagnosis. |
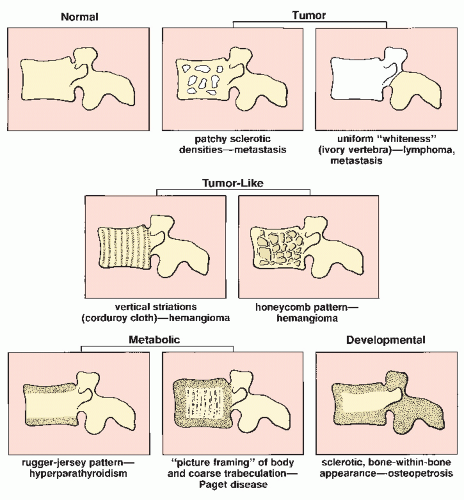 FIGURE 1.4 Density and texture of bone. Changes in the density and texture of a vertebral body on conventional radiographs may offer useful data for arriving at a diagnosis. |
Reaching a correct diagnosis does not end the process of radiologic investigation, because the course of treatment often depends on the identification of distinguishing features of a particular disorder (Fig. 1.6). For example, the diagnosis of Ewing sarcoma by conventional radiography is only the beginning of a radiologic workup of the patient. The crucial features of this tumor must be identified, such as intraosseous and soft-tissue extension (by CT or MRI) and the vascularity of the lesion (by conventional arteriography or magnetic resonance angiography [MRA]). Similarly, a diagnosis of osteosarcoma must be followed by determination of the exact extent of the lesion in the bone and the status of bone marrow in the vicinity of the tumor. This can be accomplished by precise measurement of bone marrow density using Hounsfield numbers during CT examination (see Fig. 2.14) or by using MR images with or without contrast enhancement. Diagnosing Paget disease may be an important achievement in the investigation of an unknown disorder, but even more important is the further search for an answer to a crucial question: Is there any sign of malignant transformation? (see Fig. 29.19). Localization of a lesion in the skeleton or in a particular bone can frequently be more important than diagnosis itself. The best example of this is, again, the precise localization of the nidus of osteoid osteoma because incomplete resection of this lesion invariably results in recurrence. Determining the distribution of a lesion in the skeleton is helpful in planning the treatment of various arthritides and the management of a patient with metastatic disease. Scintigraphy is an invaluable technique in this respect.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree