Hill-Sachs fracture: subchondral fracture along the posterolateral humeral head
Bankart fracture: anteroinferior glenoid fracture
Glenohumeral dislocations usually result from direct injury during contact sports. In children, these injuries are most common in the second decade [2]. Forty percent of patients present before age 22 [3]. The younger the child is at the time of dislocation, the higher the likelihood of recurrent dislocation and glenohumeral shoulder instability. Approximately 65–90 % of teenagers who suffer one shoulder dislocation will have additional dislocations [4]. Children with collagen disorders such as Ehlers-Danlos or Ulrich collagen VI deficiency have increased incidence of shoulder dislocation.
Most dislocations are anterior, and the child presents with the arm abducted and externally rotated [5]. Less commonly, glenohumeral dislocations may be posterior, inferior (luxatio erecta), or superior. Seizures may cause posterior dislocation. An additional consideration—particularly for atraumatic recurrent posterior dislocations—is underlying primary glenoid dysplasia with excessive retroversion, which can predispose to posterior dislocation.
The glenohumeral joint is a ball and socket joint invested by glenohumeral ligaments, capsule, and shoulder girdle muscles. The static stabilizers include the capsule, labrum, and glenohumeral ligaments. The active stabilizers include the rotator cuff and biceps tendon [6]. The glenoid cavity is concave and slightly retroverted (approximately 2–4°) with respect to the body of the scapula (i.e., the articular surface is directed posteriorly with respect to the scapula). The glenoid cavity itself is shallow, and its perimeter is reinforced by the fibrocartilaginous labrum to increase contact and depth of apposition with the humeral head. Although the glenohumeral joint is technically a ball and socket joint, the relatively small glenoid fossa (compared with a relatively large humeral head) allows for greater mobility at the cost of relative instability. The glenohumeral joint is more predisposed to dislocation than are hinge-type joints.
Atraumatic glenohumeral instability is usually multidirectional and may be bilateral [6]. In addition to underlying glenohumeral dysplasia, risk factors include hypermobility syndromes encountered in mixed connective tissue disease such as Marfan disease and Ehlers-Danlos syndrome [7] or activities that lead to repetitive overstretching such as swimming and gymnastics [8]. Traumatic glenohumeral dislocation tends to be unilateral and unidirectional.
Patients may respond well to rehabilitation after one traumatic dislocation, but primary repair is recommended after two or more, due to the high incidence of recurrent dislocation [9]. In one study, the incidence of recurrent dislocation was 19 % in patients treated operatively, compared with 60 % for a similar group treated nonoperatively [10]. Arthroscopic Bankart repair may be performed if the bone of the glenoid is relatively preserved. If greater than 25 % of the inferior glenoid is deficient as a result of a Bankart fracture, a Latarjet procedure may be indicated [11, 12]. In this procedure, a portion of the coracoid is transferred to the area of bone loss along the anteroinferior glenoid, improving glenoid and humeral head congruency. However, the Latarjet procedure has a relatively high incidence of complications, and, if bone loss is very severe, grafting with iliac crest bone graft may be necessary.
Traumatic multidirectional instability is treated with physical rehabilitation. If physical rehabilitation is unsuccessful, anterior capsular shift is recommended [13]. This procedure tightens the anterior and inferior capsule.
Imaging
Suspected glenohumeral dislocation is evaluated with an axillary view along with frontal radiographs in internal and external rotation. The normal glenohumeral joint has a smooth, round scapulohumeral arch, which is formed by the axillary border of the scapula, the inferior portion of the humeral neck, and the proximal humeral shaft (Fig. 6.1). In both anterior and posterior shoulder dislocations, the humeral head moves medially, and the arch is no longer aligned (Fig. 6.2). The extent of medial displacement is subtler with posterior dislocations than anterior dislocations. Axillary, Velpeau, and “Y” views help distinguish posterior from anterior glenohumeral dislocation (Fig. 6.3). The axillary view also evaluates for a glenoid fracture (bony Bankart) and determines if a Hill-Sachs fracture is either engaging (Hill-Sachs fracture depression is locked in place along the inferior glenoid rim) or non-engaging. The Velpeau view provides similar information and is useful for patients who cannot tolerate a traditional axillary view. The “Y” view principally helps determine the anteroposterior relationship but also supplements the frontal views for evaluation of the glenoid (Fig. 6.4). Hill-Sachs and Bankart fractures are presented in greater detail below.


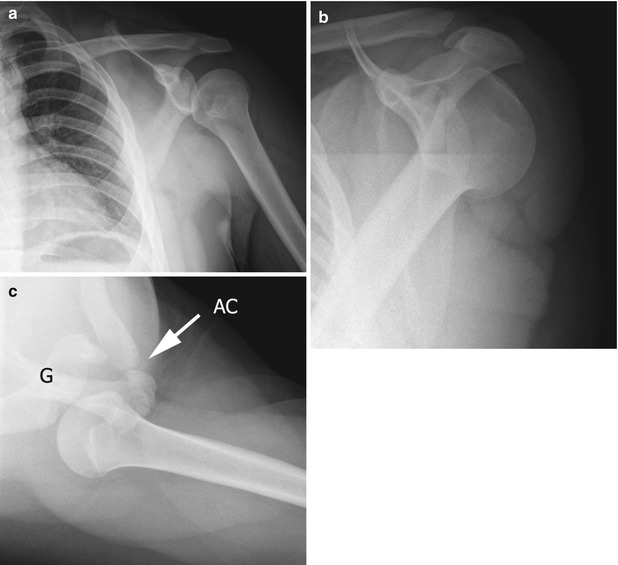
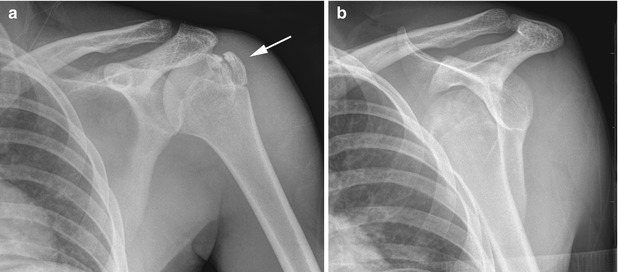

Fig. 6.1
Normal shoulder radiograph with humerus in external rotation in a 13-year-old boy. Note normal smooth scapulohumeral arch. Do not confuse the normal concavity at the interface of the greater tuberosity and humeral head (arrow) on this view (or on a poorly obtained frontal internal rotation radiograph) for a Hill-Sachs fracture

Fig. 6.2
Anterior shoulder dislocation in a 17-year-old girl. The humeral head is displaced inferomedially. Hill-Sachs fracture of the humeral head and bony Bankart fracture of the anteroinferior glenoid rim are also present (arrow)
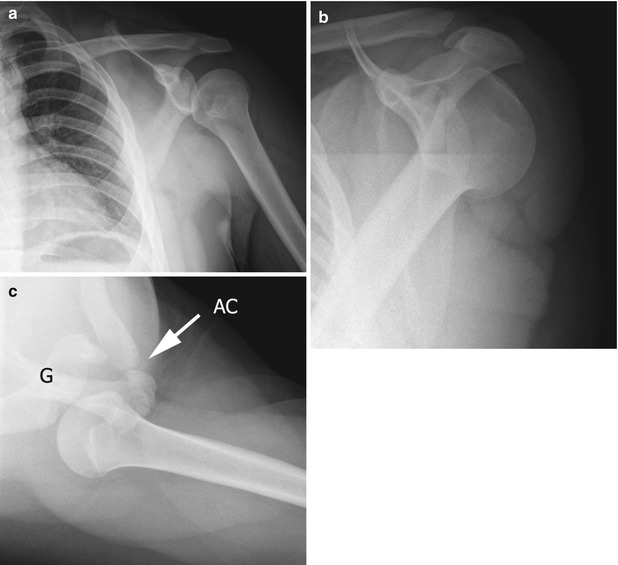
Fig. 6.3
Posterior shoulder dislocation in a 15-year-old girl. (a) There is subtle disruption of the scapulohumeral arch with medial humeral head displacement. The “Y” (b) and axillary (c) views confirm posterior shoulder dislocation. AC acromioclavicular joint. G glenoid
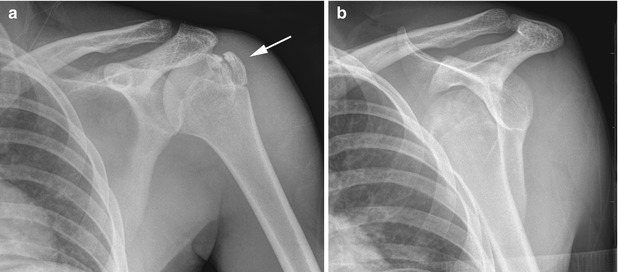
Fig. 6.4
Greater tuberosity fracture in an 11-year-old boy. (a) On the frontal view, the fracture fragment (arrow) is slightly separated, and glenohumeral alignment appears normal. (b) The “Y” view shows the humeral head is actually dislocated
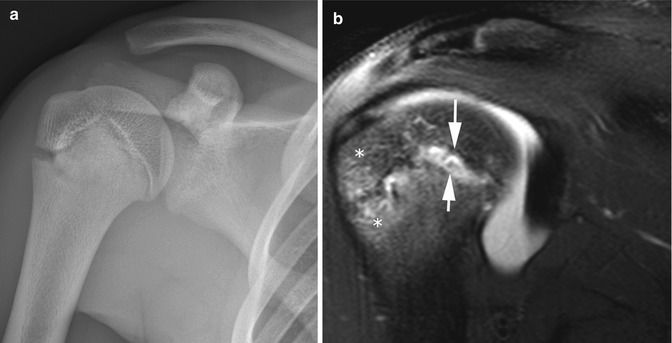
Secondary signs of anterior shoulder dislocation include a Hill-Sachs fracture and osseous Bankart fracture (Figs. 6.5 and 6.6). These fractures result as the posterolateral humeral head and anteroinferior glenoid collide as the humeral head anteriorly dislocates. These fractures are less common in children than in adults and—like shoulder dislocation in general—are more likely in the second decade. The Hill-Sachs fracture occurs along the posterolateral humeral head and is optimally seen on a frontal internal rotation view (Fig. 6.7). The normal concavity at the interface between the humeral head and the greater tuberosity may mimic a Hill-Sachs fracture on a poorly obtained internal rotation AP view. Furthermore, normal glenoid fragmentary ossification may mimic an osseous Bankart fracture. Whereas the former is usually distributed evenly throughout the glenoid rim, the Bankart fracture is more focal, at the anteroinferior glenoid.

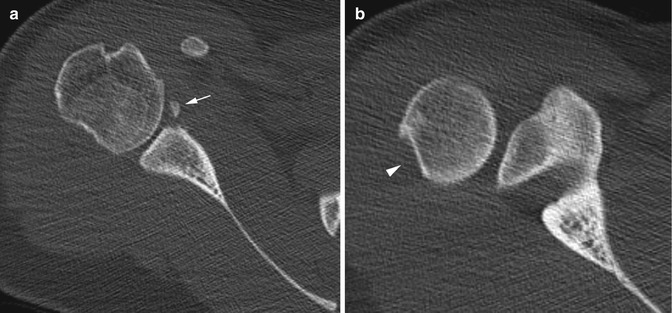


Fig. 6.5
Anterior shoulder dislocation in a 17-year-old boy. There is a bony Bankart fracture (arrow)
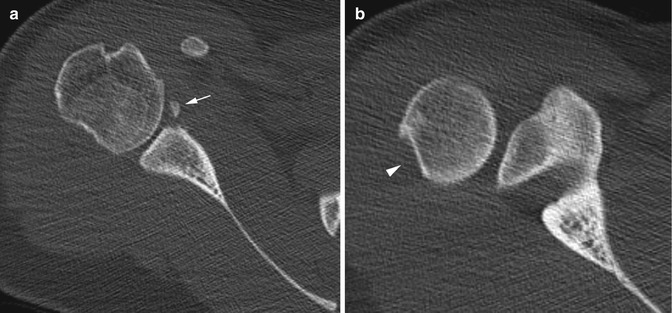
Fig. 6.6
Fractures in a 16-year-old girl with prior anterior shoulder dislocation. Axial CT images show (a) mildly displaced bony Bankart (arrow) and (b) depressed Hill-Sachs (arrowhead) fractures

Fig. 6.7
Sequela of anterior shoulder dislocation in a 15-year-old boy. There is a large Hill-Sachs fracture (arrow) on this frontal view with internal rotation
Less common glenohumeral dislocations include luxatio erecta (inferior dislocation) and posterior dislocation. Luxatio erecta occurs when the humeral head displaces inferiorly; as a result, the arm is fully abducted and held upward. Secondary signs of posterior shoulder dislocation include a reverse Hill-Sachs fracture and reverse osseous Bankart fracture. A reverse Hill-Sachs fracture occurs along the anteromedial humeral head.
Computed tomography (CT) helps determine the type of surgical stabilization necessary to repair the glenohumeral joint. Sagittal and coronal reformatted images along with three-dimensional (3D) maximum intensity projections (MIPs) are especially helpful for determining the amount of bone loss at the anteroinferior glenoid. The normal glenoid is pear-shaped. It may become an “inverted pear” (large end up) if a Bankart fracture causes bone loss along the anteroinferior quadrant (Fig. 6.8). If more than 25 % of the glenoid is deficient, surgical fixation with a Latarjet procedure or iliac crest grafting may be indicated [11, 12].
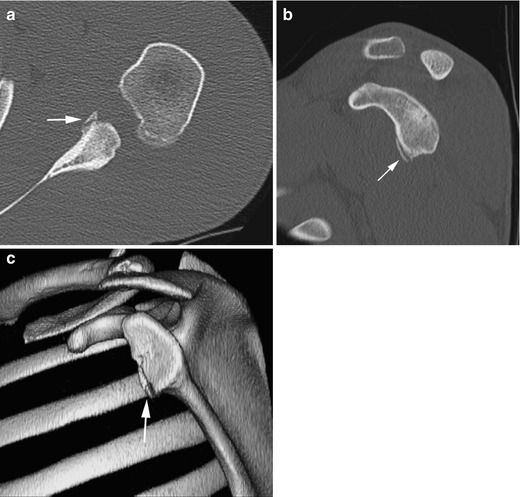
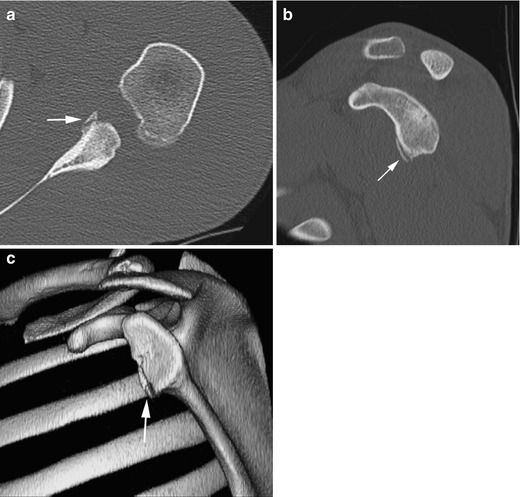
Fig. 6.8
A 16-year-old girl with osseous Bankart (arrows) demonstrated on axial (a), sagittal (b), and 3D (c) reconstructions. 3D-CT best delineates the inverted pear appearance of the glenoid due to anteroinferior deficiency after Bankart fracture (Courtesy of Tal Laor, Cincinnati Children’s Hospital)
Magnetic resonance arthrography (MRA) delineates the status of the static stabilizers of the glenohumeral joint and the various soft tissue Bankart injuries [14]. Although CT arthrography (CTA) and MRA may have comparable accuracy for the evaluation of Bankart injuries [15], MRA avoids radiation and can also evaluate marrow and soft tissue edema, as well as delineate subtypes of Bankart injuries. In the acute setting, posttraumatic glenohumeral joint fluid may have an arthrographic effect, making intra-articular gadolinium injection unnecessary.
Anteroinferior glenoid and labroligamentous injuries are classified into two subtypes: osseous Bankart and soft tissue Bankart lesions. The true soft tissue Bankart lesion is an anteroinferior labral tear with a torn scapular periosteum (Fig. 6.9), but there are many subtypes for soft tissue injuries (Fig. 6.10). It is more important to accurately describe findings than to label the exact subtype (Table 6.1). The status of the glenoid cartilage (Fig. 6.11), inferior glenohumeral ligament, labrum, and glenoid bone must all be closely evaluated.
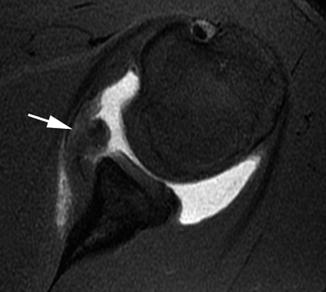
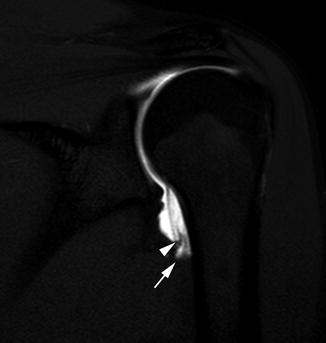
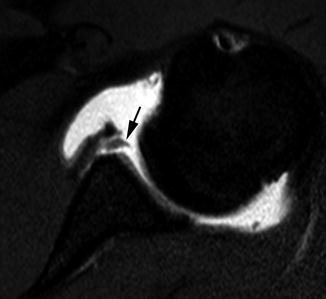
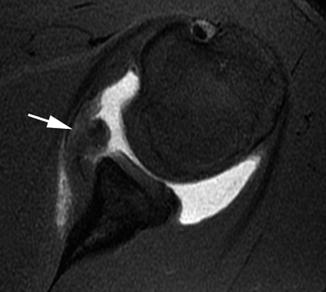
Fig. 6.9
Soft tissue Bankart lesion in a 16-year-old boy. Axial T1-weighted (T1-W) fat-suppressed (FS) image from MR arthrography (MRA) shows intra-articular contrast material insinuating between the glenoid and the displaced, torn, mass-like labral tissue (arrow)
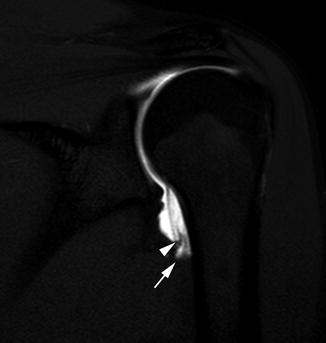
Fig. 6.10
Humeral avulsion of the glenohumeral ligament injury (HAGL) in a 16-year-old girl. Coronal T1-W FS MRA shows extra-articular contrast extension (arrow) and retracted inferior glenohumeral ligament (arrowhead)
Table 6.1
Soft tissue Bankart variations
Soft tissue Bankart variations | Description |
|---|---|
Bankart lesion (Fig. 6.9) | Anteroinferior labral tear with a torn scapular periosteum |
Perthes | Non-displaced Bankart with intact scapular periosteum |
Anterior labroligamentous periosteal sleeve avulsion (ALPSA) | Bankart lesion with medial displacement with intact scapular periosteum |
Glenolabral articular disruption (GLAD) (Fig. 6.11) | Bankart with associated glenoid chondral defect |
Humeral avulsion glenohumeral ligament (HAGL) (Fig. 6.10) | Avulsion of the anterior inferior glenohumeral ligament at its humeral insertion |
Bony avulsion glenohumeral ligament (BAGHL) | HAGL but with a humeral bone avulsion injury |
Floating anterior inferior glenohumeral ligament (AIGHL) | Combined Bankart and HAGL lesion |
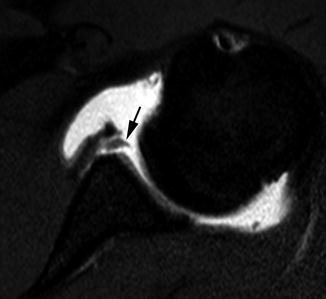
Fig. 6.11
Glenolabral articular disruption (GLAD) subtype of soft tissue Bankart lesion in a 17-year-old boy. Axial T1-W FS MRA shows a component of cartilage has been stripped (arrow)
Superior labral anterior-posterior (SLAP) injuries are sometimes associated with glenohumeral instability and at least in adults occur in approximately 20 % of patients with glenohumeral instability [17]. However, treatment is not always necessary.
There are no specific imaging findings for atraumatic multidirectional shoulder instability other than a patulous glenohumeral capsule, which is best seen along the axillary recess after distention during arthrography. Therefore, the diagnosis is generally made on gestalt interpretation in conjunction with clinical findings [8]. Associated findings include articular and labral injuries resulting from recurrent dislocations.
2 Proximal Humeral Fractures
Proximal humeral fractures comprise 0.5 % of all fractures in children and between 4 and 7 % of all epiphyseal fractures [18]. The mechanism and force of injury resemble those for shoulder dislocations, but the force decompresses along the proximal humerus. The unbalanced biomechanical pull of muscle insertions proximal and distal to the site of fracture leads to angular and displacement deformities.
An understanding of the timing and appearance of the ossification centers of the proximal humerus helps in interpreting radiographs in the setting of trauma and elbow ossification centers also helps determine the clinical significance of different fracture patterns. There are three ossification centers at the proximal humerus. The humeral head epiphysis begins to ossify at or shortly after birth, and the greater tuberosity apophysis begins to ossify at age 3 years. The lesser tuberosity begins to ossify at age 5 years, and the humeral head, greater tuberosity, and lesser tuberosity fuse at age 6 [19]. The proximal humeral physis remains open until age 14–17 in girls and 16–18 in boys [20]. Damage to this physis can result in significant growth disturbance, as it is responsible for 80 % of the longitudinal growth of the humerus. However, as a general rule, proximal humeral fractures are more likely to remodel in younger children than in older children due to the open physis.
Non-displaced or minimally displaced proximal humeral fractures are treated nonoperatively. Severely angulated or displaced fractures may require operative fixation in children older than 10–13 years of age [18, 21]. In children under 11 years of age, most if not all fractures will remodel without long-term sequelae and can be treated nonoperatively [19]. Surgical reduction is indicated in open proximal humeral fractures or if there is evidence of neurovascular compromise.
Imaging
Three-view shoulder (frontal internal and external rotation along with axillary) or two-view humerus radiographs adequately assess most proximal humeral fractures. It is important to determine the amount of displacement, as this predicts prognosis and determines appropriate treatment. The Neer classification offers a convenient way to categorize proximal humeral fractures (Table 6.2), although it is not generally used with children [19]. Angulation should also be addressed (Fig. 6.12), although the need to report the precise degree of fracture angulation varies with institution and orthopedic surgeon preference [18]. In older children, fractures are frequently complete (Fig. 6.12), while in younger children, buckle fractures are common (Fig. 6.13). The fracture line orientation, physeal involvement (humeral head, greater tuberosity, lesser tuberosity) (Fig. 6.14), and presence of comminution should be discussed, as with any fracture.



Table 6.2
Neer classification of proximal humeral fractures
Grade | Displacement |
|---|---|
I | <5 mm |
II | <1/3 shaft width |
III | 2/3 shaft width |
IV | >2/3 shaft width |

Fig. 6.12
Neer type I displaced and mildly comminuted fracture of the surgical neck of the humerus in a 5-year-old girl. There is less than 5 mm of lateral displacement of the distal fragment

Fig. 6.13
Non-displaced buckle fracture (arrow) of the surgical neck of the humerus in a 3-year-old girl

Fig. 6.14
Neer grade 4 proximal humeral fracture in a 13-year-old boy. The fracture extends from the lateral physis to the greater tuberosity and is displaced by more than two-third of the width of the shaft
Radiography is almost always sufficient for imaging proximal humeral fractures. Occasionally, for complicated fractures, magnetic resonance imaging (MRI) may help identify tendon, periosteum, or muscle interposition at the fracture site [22], which could impede proper healing.
3 Little Leaguer’s Shoulder (Box 6.2)
Box 6.2: Little Leaguer’s Shoulder (Young Throwing Athlete)
Radiographs: |
Proximal metaphyseal sclerosis, lateral metaphyseal fragmentation |
Wide physis (resembles acute Salter-Harris I fracture) |
MRI: |
T1: Physeal widening |
Fluid sensitive: metaphyseal edema, periosteal reaction, and juxtacortical soft tissue edema |
Less common: epiphyseal edema, juxtaphyseal cysts, and periosteal edema |
Little Leaguer’s shoulder, seen in athletes who throw overhead, is an overuse injury of the proximal humeral physis and is most likely a chronic non-displaced Salter-Harris I fracture. The injury most commonly occurs during growth spurts in boys between 11 and 14 years of age [23]. Rotational torqueing generated during the acceleration phase of an overhead throw probably causes the injury.
The glenohumeral joint in childhood is quite lax. However, in early adolescence, a dramatic change in range of motion occurs, with decreased internal and external rotation, along with increased shoulder elevation. The decrease in rotational motion may contribute to excessive stress at the physis with throwing and thus predispose children to this injury [24].
A single acute event generally does not cause the injury; symptoms develop gradually and correlate with pitch count. Symptoms include pain during throwing, with palpation of the proximal humerus, and during resisted external rotation of the humerus [25].
The treatment for Little Leaguer’s shoulder is rest from overhead throwing [23]. Surgery is not indicated. If the child returns to throwing too early, continued physeal damage may lead to displacement and eventual early physeal closure. Prevention of this injury is one of the reasons for pitch count regulations for Little League players.
Imaging
Little Leaguer’s shoulder is usually diagnosed clinically. Radiographs can confirm the diagnosis or suggest alternative etiologies for symptoms. Findings include proximal metaphyseal sclerosis, lateral metaphyseal fragmentation, physeal widening, and demineralization (Fig. 6.15) [25, 26]. Note that this appearance is indistinguishable from an acute non-displaced Salter-Harris I fracture. The term Little Leaguer’s shoulder should not be used when there is a displaced Salter-Harris I proximal humeral fracture (Fig. 6.16).