Fig. 4.1
Spondylolysis at L5. The arrow points to the bony defect in the pars interarticularis (Image copyright Shriners Hospital for Children Northern California)
Box 4.1: Spondylolysis
Frontal | 30° cranial angulation helps visualization |
Oblique/lateral | Lucency crossing neck of “Scottie dog” |
Unilateral | Spinous process tilts toward lytic side |
Contralateral lamina sclerotic, hypertrophied |
On the oblique or lateral view, the typical isthmic spondylolysis appears as lucency below the eyelike intervertebral foramen and crossing the pars interarticularis at the neck of the “Scottie dog” (Fig. 4.2). The margins of the defect may be ragged and square or smooth and tapered. The size of the gap varies, and there may be fragmentation in the fracture interval. After the fracture heals, the gap may close and the isthmus may appear normal, elongated, or sclerotic (reflecting repair).
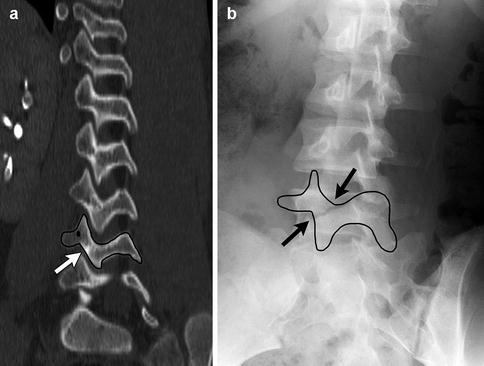
Fig. 4.2
Spondylolysis of L5 in a teen. (a) For comparison, normal pedicle, pars interarticularis (white arrow), and articulating facets of the L4 vertebra on an oblique sagittal reformatted computed tomography (CT) image. (b) “Scottie dog” formed by the “neck” of the Scottie dog is broken (black arrows)
When only one lamina is involved, the facet on the unstable side will advance, causing the spinous process of that vertebra to tilt toward the defective side. Additionally, increased stress on the normal side causes sclerosis and hypertrophy of this lamina and pedicle [7]. In the typical isthmic or superior facet defect, this change occurs at the level of the abnormal lamina; in uncommon inferior laminar defects, the hypertrophied pedicle is below the lesion [8]. In a child with back pain, the affected pedicle may be mistaken for osteoid osteoma, since it is sclerotic and also shows increased uptake on nuclear scintigraphy.
Nuclear Medicine Imaging
Bone scan with single-photon emission computed tomography (SPECT) is very useful for diagnosing spondylolysis (Fig. 4.3). SPECT may show increased uptake at the pars interarticularis when radiographs are normal. In addition, it can help distinguish between symptomatic spondylolysis (increased activity) and silent spondylolysis (normal activity) [9].
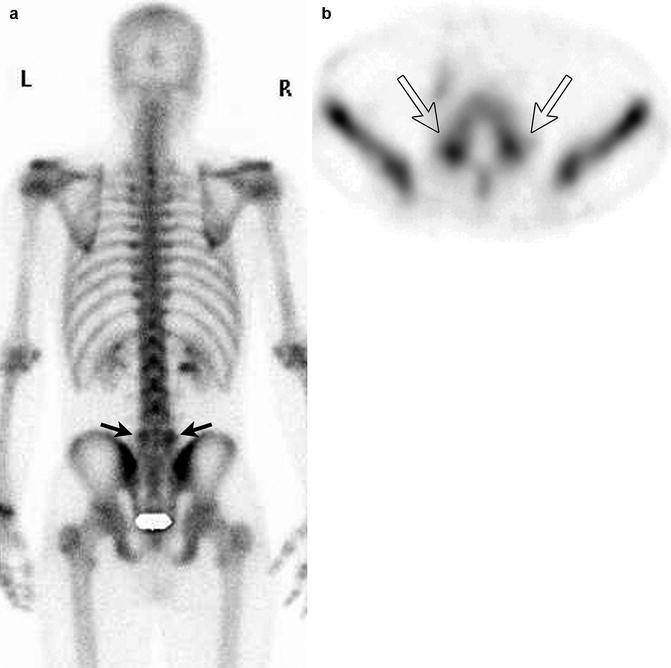
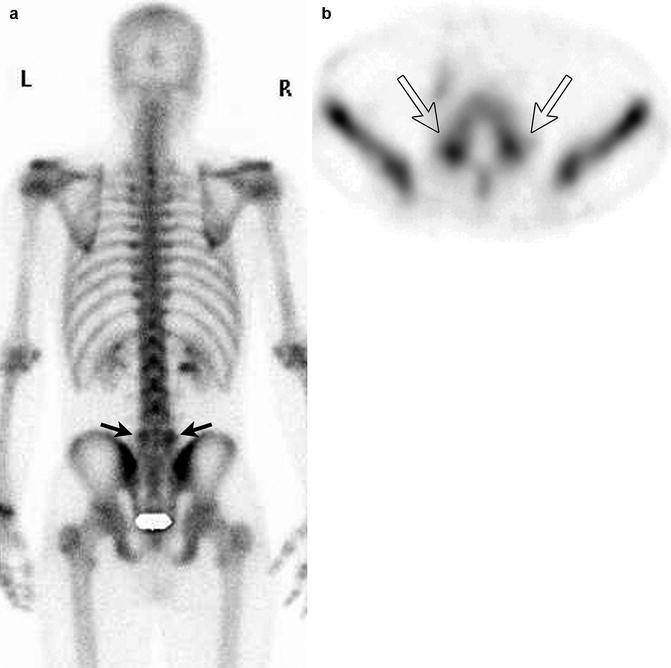
Fig. 4.3
Bilateral spondylolysis at L5 in a 16-year-old athlete. (a) Note the increased uptake on the posterior view planar bone scan (black arrows). (b) Increased uptake at the pars interarticularis at L5 on axial single-photon emission computed tomography (SPECT) (white arrows) (Courtesy of Cameron Foster)
Computed Tomography (CT) (Box 4.2)
CT is a valuable tool for diagnosing spondylolysis, as it provides excellent bony detail and can be reformatted in multiple planes (Fig. 4.4). On the axial projection, it may be challenging to distinguish between a spondylolytic defect and a normal facet joint, and all the contiguous slices in the series must be studied in sequence. The facet is smoothly marginated, slightly curved, and level with the disc, whereas the pars defect is usually irregularly marginated, fragmented, or sclerotic and both more superior (at the level of the pedicle) and anterior to the normal facet joint [10]. Sagittal and coronal reformatted images show pars defects well. The anteroposterior diameter of the canal is often increased, and disc herniation is occasionally associated, usually at the level above the laminar defect. Spondylolisthesis may cause a false impression of herniation.
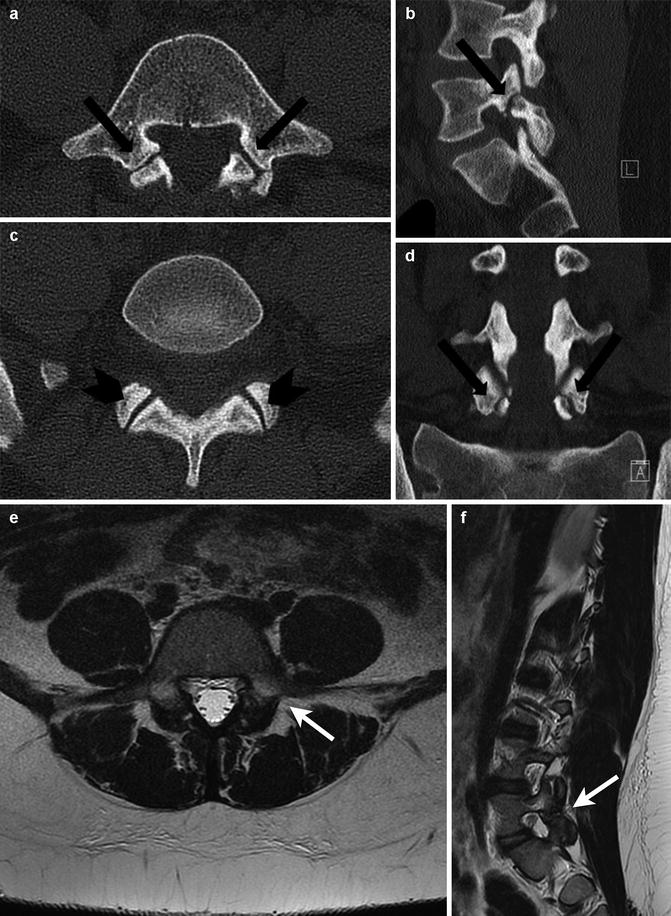
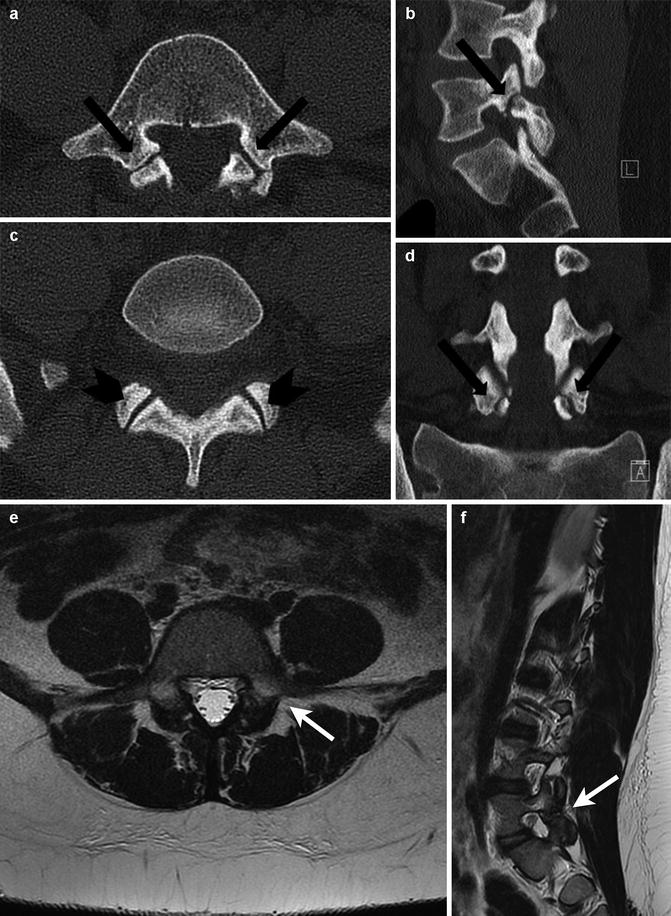
Fig. 4.4
Bilateral spondylolysis in an 11-year-old. (a, b) Axial CTs show that the irregular pars interarticularis defects (arrows) are located at the level of the pedicles. These must be differentiated from the normal facet joints (arrowheads) that are located at the level of the disc. Sagittal (c) and coronal (d) reformatted CTs show the spondylolysis defects. Axial (e) and sagittal (f) T2-W images show hyperintense edema anterior to the hypointense pars defects (arrows)
Box 4.2: Spondylolytic Lucency Vs Normal Facet Joint CT
Spondylolysis | Facet |
Superior to disc,anterior to facet joint | Level with disc |
Irregular margins | Smooth margins |
Fragmented and sclerotic | Slightly curved |
Magnetic Resonance Imaging (MRI)
MRI is as accurate as CT in the diagnosis of lower lumbar spondylolysis [11]. It is characterized by interruption of marrow signal in the lamina and increased T2 signal in the defect. A sclerotic but continuous pars interarticularis may result in a false positive. On all pulse sequences, the cleft is best shown in the sagittal plane as a zone of intermediate signal that is perpendicular to the facets; signal varies with the amount of fibrous tissue, cartilage, and fluid in the defect (Fig. 4.4). Surrounding marrow edema appears hyperintense on T2-weighted (T2-W) images. If spondylolisthesis is present, the disc may appear prolapsed and may be split into two parts [12].
2 Spondylolisthesis
Spondylolysis may lead to spondylolisthesis, as the fracture allows one vertebral body to slip forward over the one below. This lesion is almost exclusively limited to the lower lumbar spine, usually with L5 slipping forward over S1 (Fig. 4.5). The most common cause of spondylolisthesis is an isthmic (pars interarticularis) defect in which the posterior neural arch remains stationary while the anterior body slides forward. In rare cases, neural arch dysplasia allows slippage, when facet and laminar defects insufficiently restrain forward movement. This can occur with myelomeningocele and neurofibromatosis. Degenerative and traumatic causes are rare in children. Spondylolisthesis is very unusual in the cervical spine.


Fig. 4.5
Bilateral spondylolysis and grade 1 spondylolisthesis in an 11-year-old girl. Forward slip of L5 on S1 is less than one fourth the width of the S1 vertebra (Image copyright Shriners Hospital for Children Northern California)
Spondylolisthesis develops in less than half of those with spondylolysis. This slipping process rarely starts before age 7 and often begins or accelerates between the ages of 9 and 12, rarely increasing after age 20. While no prognostic radiographic or clinical factors can predict the progression of mild slips [13], in most cases ultimate vertebral displacement is less than 25 or 30 %.
Dysplastic spondylolisthesis is more common in girls, whereas the isthmic form is more common in boys. Most patients with spondylolysis alone are asymptomatic. When spondylolisthesis develops, low back pain and hamstring spasm are often noted.
Imaging
The vertebra above slips forward on the one below, usually L5 on S1 (Fig. 4.6). On a frontal view, if L5 is slipped significantly forward on S1, a double density results, resembling an inverted cocked hat (Fig. 4.7). A reliable method for recognizing (but not quantifying) spondylolisthesis on the oblique projection is noting that each successive facet is located anterior to the one just above. If this progression is reversed, corresponding slip must have occurred.
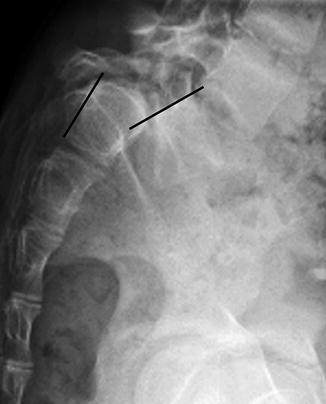

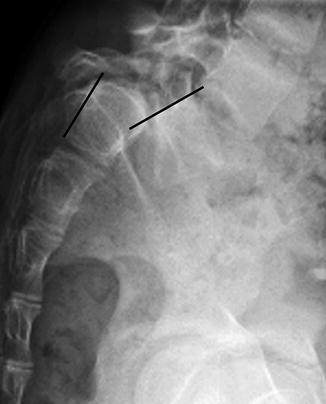
Fig. 4.6
Grade IV spondylolisthesis in a 12-year-old girl with spondylolysis and about 90 % anterior slip of L5 on S1 (Image copyright Shriners Hospital for Children Northern California)

Fig. 4.7
Grade IV spondylolisthesis. The inverted cocked hat, or tricorn hat, creates a double density on frontal projection (Image copyright Shriners Hospital for Children Northern California)
Erect lateral radiographs may show more extensive slip than recumbent cross-table lateral examinations. Hypoplasia or scoliotic rotation of L5 can result in a false impression of spondylolisthesis. Using the lateral view, magnitude is grading from I to V: the superior surface of the sacrum is divided into four zones and the location of the slipped vertebra’s posteroinferior corner is determined (Fig. 4.8). An alternate, more reproducible assessment determines the percentage of slip by dividing the distance slipped by the width of the body below.
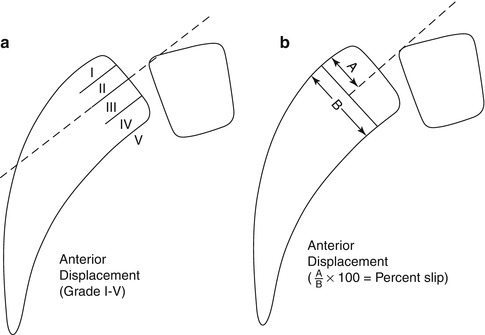
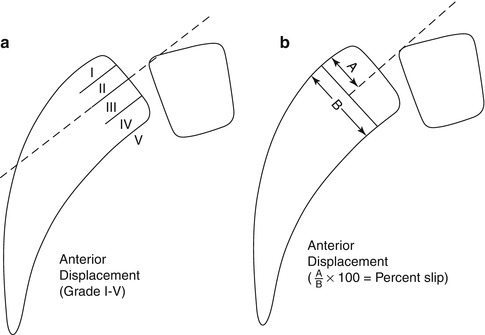
Fig. 4.8
Methods for assessing severity of spondylolisthesis. (a) shows technique for grading spondylolisthesis, and (b) shows technique for calculating the percentage of slip. Grade I is forward slip of the posterior corner of the affected vertebra (usually L5) by less than one fourth (0–25 %) of the width of the vertebra it slips on (usually S1). Grade II is 1/4–1/2 (26–50 %) of the width. Grade III is 1/2–3/4 (51–75 %). Grade IV 3/4–1 (76–100 %). Grade V is more than 100 % slip; the displaced vertebral body falls forward and is angled caudally
In long-standing spondylolisthesis, the slipped vertebral body becomes trapezoidal and its anterior face longer than the posterior due to underdevelopment of the posteroinferior corner. The superior surface of the sacrum becomes rounded because of abnormal pressure and impaired growth.
3 Spinal Trauma
Stability of the vertebral column depends on the vertebrae; the posterior muscular, ligamentous, and capsular structures; the intervertebral disc; and the anterior and posterior longitudinal ligaments. The mechanisms that cause traumatic stress include flexion, rotation, extension, compression, and shearing. The anatomic peculiarities of various segments determine the type of lesion: horizontal facets of the cervical region promote dislocation and disc tear without fracture, whereas the more vertical lumbar facets predispose to facet fracture and slice-type fracture of the vertebral body. Dissolution of bone, for example, in the odontoid, may follow trauma.
The cervical spine is fractured in 37–80 % of pediatric spine injuries, and there is a higher incidence of neurologic injuries in younger children (less than 8 years of age) than in older children or adults [14]. Fractures in younger children are more likely to affect the upper cervical spine—from the occiput to C3. This is in part because movement occurs at a higher fulcrum, about C2–3 in young children versus C5–6 in adults and older children. It is also a consequence of their relatively large head and small body as well as increased mobility due to lax ligaments and underdeveloped neck muscles. In young children the geometry of the cervical vertebrae differs from that in adults, further predisposing them to upper cervical spine injury [15]. Elasticity of the ligaments also increases the likelihood of cord injury without osseous injury. Common upper cervical injuries include occiput-C1 injury, with possible rupture of ligaments and craniocervical separation; Jefferson fractures of the atlas; atlantoaxial separation or rotation; odontoid fractures; and hangman fracture of C2.
Older children are subject to similar fractures as adults. Most fractures involve the thoracic and lumbar spine, though the mid and lower cervical spine may be affected. Vertebral body compression fractures are most common. It is important to evaluate for additional fractures if one fracture is identified, as the presence of injury at multiple noncontiguous levels in children is associated with an increased probability of neurologic injury [16].
Imaging
Radiographs provide initial evaluation of spine injury (Fig. 4.9). Flexion and extension radiographs can help identify unstable ligamentous injury and clarify questionable abnormalities but are fraught with problems and can be unsafe to perform [14]. Patients with radiographic abnormalities and those with high-risk mechanism of injury require CT examination with coronal and sagittal reformatting. CT is superior to all other modalities in detecting and delineating spinal fractures, while MRI best defines muscular, ligamentous, and spinal cord injury (Fig. 4.10) [17]. MRI can delineate significant craniocervical junction injury in young children with normal CTs and may be considered if there is a high likelihood of injury [18].
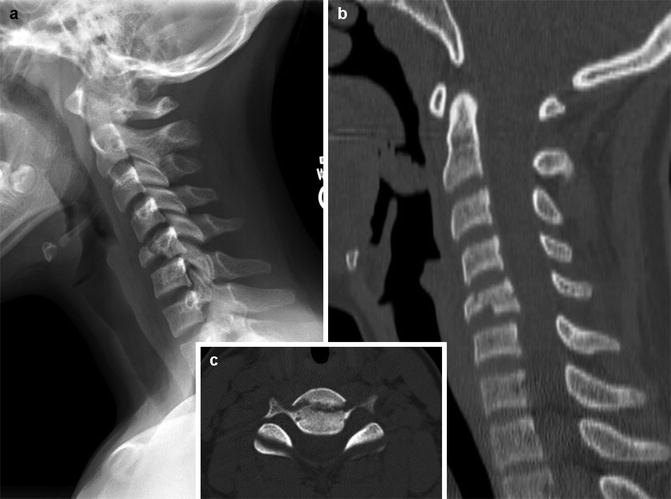

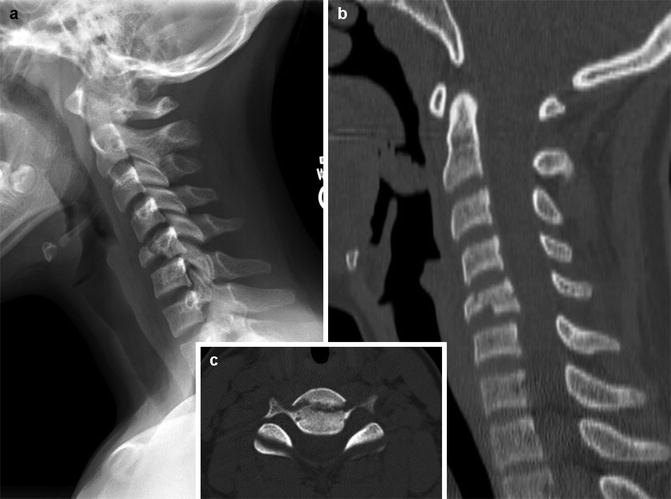
Fig. 4.9
Flexion-distraction fracture at C5–6 in a 12-year-old boy. (a) The C5–6 injury shows the C6 vertebral body is fractured, and there is increased distance between the spinous processes of C5 and C6, suggesting ligamentous injury. Loss of normal cervical lordosis. (b) Sagittal reformatted CT confirms these findings. (c) Axial CT shows the fracture bisects the vertebral body

Fig. 4.10
C5–6 flexion-distraction injury. Sagittal short tau inversion recovery (STIR) MRI shows C5 and C6 are fractured, and C6 is deformed with mild retropulsion of the posterior aspects of the vertebrae and resultant cord compression. Extensive soft tissue edema and ligamentous injury (arrow)
Flexion injury results in tears and sprains of posterior spinal muscles and ligaments, as well as vertebral body compression fractures. Rotational forces may contribute to subluxation. The cervical spine is prone to hyperextension injury caused by blows to the head, collisions, and whiplash. The thoracic and lumbar spine can suffer posterior element avulsion fractures [17].
Burst fractures, secondary to axial compressive loading, show up clearly by CT (Fig. 4.11). A retropulsed fragment may be rotated and displaced craniad or caudad. Callus extending into the spinal canal may cause late neurologic deterioration. MRI may investigate spinal cord injury. Acute intraspinal hemorrhage or cord laceration along with late myelopathy, syrinx formation, and atrophy may be evident, as well as neural injury remote from the region of skeletal injury.
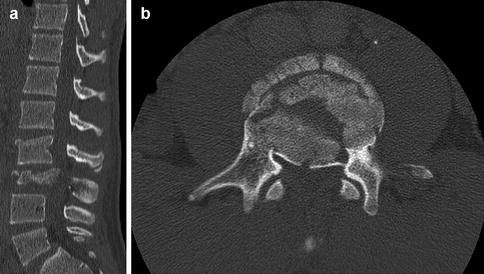
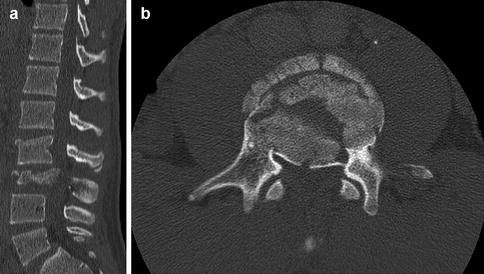
Fig. 4.11
Burst fracture in a teen. Sagittal reformatted (a) and axial (b) CT images show a burst fracture of L3. Retropulsion of posterior fragments significantly narrows the spinal canal
The Chance fracture of the spine (Fig. 4.12) is an unstable flexion-distraction transverse disruption through the posterior elements and into the vertebral body [19]. It typically occurs at the T12–L2 level. Chance fractures are frequently associated with the lap belt injury complex: acute flexion of the abdomen over a lap belt during rapid deceleration. The abdominal viscera are compressed, possibly resulting in hollow viscus injury, as the spine flexes over the fulcrum of the belt. Sagittal reformatted CT images best show Chance fractures. Fortunately, associated spinal cord injury is rare.
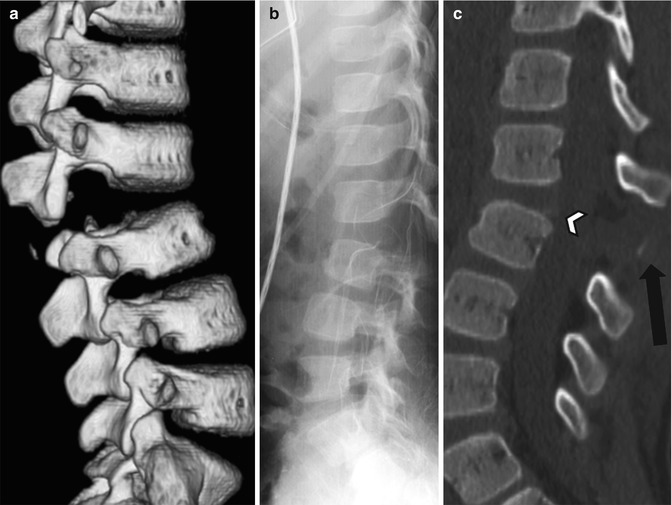
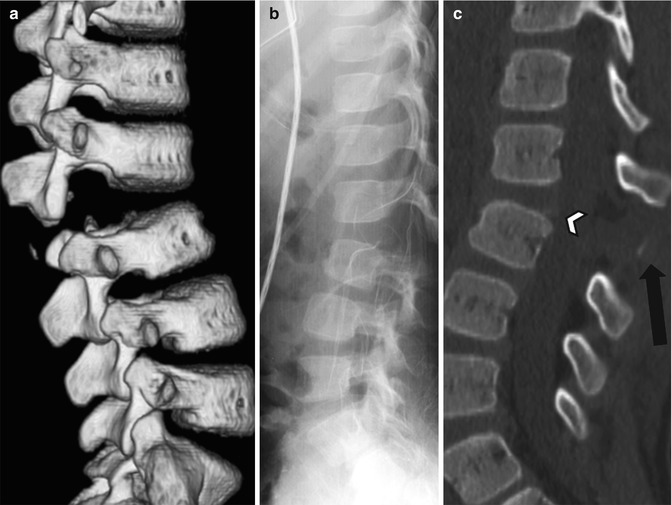
Fig. 4.12
Chance fracture in an 8-year-old girl who was a restrained backseat passenger in a motor vehicle accident and presented with a lap-belt bruise across her lower abdomen. Three-dimensional (3D) CT (a), radiograph (b), and sagittal reformatted CT (c) all show the fracture with distraction of the spinous processes at L2–3. A fragment avulsed from the L2 spinous process is displaced into the gap (black arrow). Vague lifting of bony density at the posterosuperior L3 vertebral body likely results from fracture through the ring apophysis (arrowhead). Widening of the disc space indicates disc fracture
Hyperflexion compression fractures may occur in children under age 2 who are subject to nonaccidental trauma [20]. These fractures may be clinically silent or associated with neurologic injury (Fig. 4.13). Subluxation and kyphosis may result. Extreme vertebral compression may suggest the dysostosis multiplex picture of mucopolysaccharidoses, and loss of disc space from traumatic intravertebral herniation may mimic pyogenic infection.


Fig. 4.13
T11–12 hyperflexion dislocation in an abused infant who was slammed buttocks first onto a table
4 Intervertebral Disc Disorders
4.1 Discitis
Discitis is a relatively rare disorder of the pediatric spine, possibly inflammatory or due to low-grade bacterial infection (see Chap. 19 for additional discussion). Clinical findings may include back pain and stiffness, limp, fever, and increased sedimentation rate. Interestingly, children under 28 months of age tend not to complain of back pain, while older children do [21]. In most cases, blood cultures are sterile; occasionally, biopsy material from the involved disc shows bacterial growth—usually Staphylococcus aureus. Typically, biopsy or aspiration is unnecessary unless antibiotic treatment fails. Prognosis for full recovery is good. The lumbar spine is involved in three fourths of patients, whereas the cervical spine is rarely affected. Occasionally, lesions are present at more than one level.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree