10 The Urinary Bladder
V. Nicolas and D. Beyersdorff
Introduction
Ultrasound, cystography, voiding cystourethrography, and intravenous urography are the primary imaging modalities for examining the urinary bladder. If these diagnostic tests are inconclusive, CT or MRI can be employed to obtain important supplementary information. As elsewhere in the body, MRI affords excellent soft-tissue contrast and enables multiplanar imaging. However, CT is gaining on MRI now that multislice spiral CT scanners provide thin-slice reconstruction with the option of additional multiplanar reconstruction.
Indications
MRI of the bladder is mainly used to stage known bladder cancer, detect tumor recurrence, and evaluate for secondary invasion of the bladder by gynecologic, prostatic, or rectal neoplasms. In addition, the multiplanar capabilities of MRI may provide important information in selected patients with congenital anomalies or inflammatory disease.
Imaging Technique
Phased-array coil systems have become the standard in abdominal MRI. When imaging the urinary bladder and perivesical fat, a phased-array coil (usually consisting of four to eight elements) markedly improves the signal-to-noise ratio (SNR) compared with the integrated whole-body resonator and thus enables acquisition of higher-resolution images. Optimal bladder filling is important for a complete evaluation and the detection of small lesions. This is achieved by asking the patient to void a couple of hours before the examination and then not again until completion of the test. On the other hand, overdistention must also be avoided as it may obscure small lesions and can lead to motion artifacts because the patient is uncomfortable and more likely to move. To minimize such artifacts, it is also important to ensure comfortable positioning, e.g., by elevating the patient’s knees with a small pad. Respiratory artifacts can be reduced by placing a compression band across the abdomen. The same effect is achieved by exerting slight pressure above the pubic bone with the phased-array coil. Artifacts caused by bowel motion are minimized by intravenous/intramuscular injection of an antispasmodic agent.
Imaging Planes
The bladder protocol should include an imaging plane perpendicular to the interface between a suspected lesion and the bladder wall, i. e., an axial or coronal plane for evaluating a lesion of the lateral wall and a sagittal or coronal plane for lesions involving the bladder dome or bladder outlet. Occasionally, a double oblique imaging plane is necessary to acquire images perpendicular to the affected wall.1
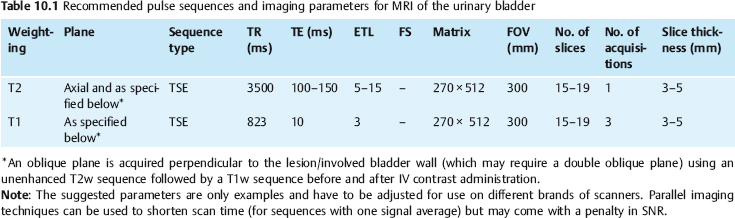
Pulse Sequences
The urinary bladder is imaged with a combination of unenhanced T2w and T1w sequences in at least two planes and a T1w sequence after intravenous contrast administration (Table 10.1). The slice thickness should not exceed 4–5 mm.
We use the following protocol for MRI of the bladder:
- a multiplanar localizer scan
- standard fast T1w and T2w sequences in axial, coronal, and sagittal planes for tumor localization
- an axial T2w TSE sequence for acquisition of high-resolution images (oblique plane perpendicular to the tumor–bladder wall interface if necessary)
- a T1w sequence oriented perpendicular to the tumor-bladder wall interface before and after administration of nonspecific Gd-based contrast medium.
Alternatively, thin-slice T1w sequences or 3D sequences can be used.
Contrast Media
Contrast-enhanced bladder MRI is performed using one of the commercially available Gd-based contrast media (e.g., Magnevist, Dotarem, Prohance) injected at a standard dose of 0.1 mmol Gd per kg body weight. When images are acquired with a conventional T1w TSE sequence, it is important to start acquisition immediately after intravenous bolus injection in order not to miss the early phase of maximum contrast between urine, mucosa, and bladder wall. Bladder neoplasms typically enhance early in a dynamic study. In patients with suspected tumor recurrence, quantification of the signal increase on dynamic contrast-enhanced images may occasionally help distinguish scar tissue from recurrent tumor. Atumor may be obscured on postcontrast MRI if images are acquired after distribution of the contrast medium in the urine. Since the signal intensity of urine varies with the Gd concentration, inhomogeneous distribution of the contrast medium may occasionally lead to layering within the bladder. This is seen as low signal intensity in the dependent portion of the bladder, where the Gd concentration is highest; as high signal intensity of a middle layer, reflecting urine containing less contrast medium; and as low signal intensity of a third layer anteriorly, representing unenhanced urine (see Fig. 10.3). Direct intravesical administration of iron-oxide-based contrast medium causes uniform signal loss of urine on T2-weighted images but offers no diagnostic advantage because delineation of the mucosa is not improved.2
MRI Appearance of Normal Anatomy
The standard protocol for MRI of the urinary bladder comprises unenhanced T1w and T2w sequences and a T1w sequence after intravenous contrast administration. With their rather long T1 times, urine and the bladder wall have low signal intensity on T1w images. On heavily T1-weighted images, the distinction between urine and the wall may become difficult if the bladder is very full. On T2w images, the bladder wall is seen as a low-signal-intensity band between the high-signal-intensity urine and the rather high signal intensity of the perivesical fat. One must be aware that chemical shift artifacts which occur at the bladder/perivesical fat interface can obscure the bladder wall or mimic pathology. The true nature of such artifacts will be revealed by changing the phase-encoding direction. Following intravenous contrast administration, the mucosa enhances earlier than the outer muscular layer.3 On later images, the entire bladder wall becomes enhanced but the SI remains below that of the mucosa. Contrast-enhanced urine entering the bladder can result in inhomogeneous enhancement around the ureteral orifices on early postcontrast images with subsequent layering before the urine finally shows relatively uniform enhancement.
MRI Appearance of Pathologic Entities
Anomalies
The most common urinary bladder anomalies are agenesis, hypoplasia, duplication, exstrophy, and diverticula. Since ultrasound and cystography enable reliable diagnosis in most cases, MRI is very rarely used in patients with suspected bladder anomalies.
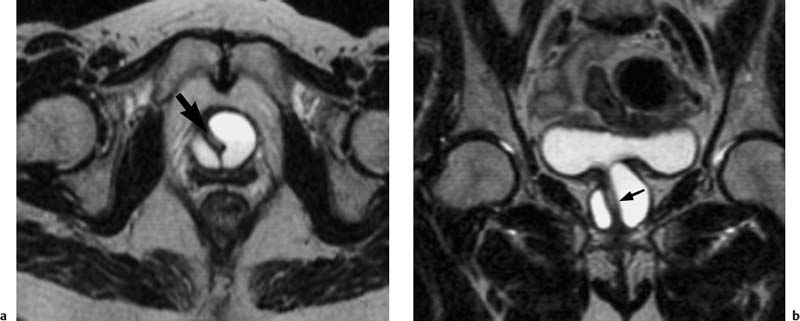
Urinary bladder diverticula are often detected incidentally in patients undergoing pelvic MRI for other reasons. The majority are acquired (pseudo-)diverticula that develop as a result of increased intravesical pressure due to conditions causing bladder outlet obstruction such as benign prostatic hyperplasia (BPH), prostate cancer, or urethral stricture. MRI will reveal a bladder diverticulum as an outpouching of the bladder wall. The wall is thinner than the normal bladder wall and has low signal intensity on T2w images. The diverticular neck is typically narrow, but some diverticula have a wide neck (Fig. 10.1). Most bladder diverticula have no clinical relevance. However, stagnant urine in the pouch can lead to inflammation and stone formation, and bladder neoplasms more often arise in a diverticulum (see below).
Inflammation
The diagnosis of cystitis is made by clinical and bacteriologic examinations in most cases, occasionally supplemented by cystoscopy with biopsy. Bacteria are the most common etiologic agents. Older women often have concomitant urethritis and vaginitis. Other causes are bladder voiding dysfunction, surgery, and radiotherapy, e.g., for gynecologic tumors. Inflammation causes focal or diffuse thickening of the bladder wall with an intermediate signal intensity or heterogeneous appearance on T1w images. On T2w images, inflammatory areas are of higher signal intensity than uninvolved wall segments. According to Hricak4 acute radiation cystitis has a characteristic MR appearance with the wall showing uniform signal intensity on unenhanced T1w images, while T2w images reveal a thin inner layer of lower signal intensity compared with the thickened outer layer. Following intravenous contrast administration, the inflamed bladder wall will show inhomogeneous enhancement. The high signal intensity on T2w images and the strong enhancement are due to hyperemia.5 Chronic cystitis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree