15
Thoracic Neoplasms
Eugene C. Lin and Abass Alavi
Positron emission tomography (PET) is a well-established modality for evaluating indeterminate solitary pulmonary nodules. It is most cost-effective when used in nodules with a pretest probability of malignancy between 12 and 69%.1
- If the pretest probability of malignancy is very low, observation alone is considered acceptable in most circumstances.
- If the pretest probability is high, biopsy/resection should be considered instead. With a pretest probability of 80%, the probability of malignancy is still 14% with a negative PET.
- PET. Sensitivity 97%, specificity 78%2
- PET/CT. Sensitivity 97%, specificity 85%3
- By incorporating the computed tomography (CT) findings into the PET/CT interpretation (e.g., a highly suspicious nodule on CT would be interpreted as positive even if PET is negative), the sensitivity of CT and specificity of PET are synergistic. This approach results in a higher accuracy compared with PET alone3 and may be particularly helpful for nodules < 1 cm.
- A negative PET scan indicates that a nodule is highly likely to be benign, but follow-up is still necessary, as a small number of nodules will be malignant and have low fluorodeoxyglucose (FDG) uptake.
- It is important to take the pretest probability of malignancy into account with a negative PET scan result.
- A positive result indicates that the nodule is most likely malignant.
- Although false-positive results are noted with PET, PET has higher specificity than competing modalities.
- A negative PET result is usually more accurate than a positive result, as false-negative findings are less common than false-positive lesions for malignancy.
- Dynamic contrast-enhanced CT. Sensitivity 98%, specificity 58%4
- In two studies comparing PET and contrast-enhanced CT, PET had a slightly lower sensitivity and much higher specificity in one5 and a greater sensitivity and comparable specificity in another.6 Overall, PET is more accurate than contrast-enhanced CT for pulmonary nodule evaluation. CT should primarily be used in nodules < 1 cm, if PET is not available, or in low-risk patients.
- Technetium 99m depreotide (somatostatin analogue). PET is more sensitive than technetium 99m depreotide, and specificity is comparable.7,8
- PET scan can be useful after a positive dynamic contrast CT examination if biopsy is not desirable.
- Over half of false-positive lesions on contrast CT can be shown to be true-negative on PET.9
- An additional benefit of PET over other modalities is that if a PET scan is performed to evaluate a solitary pulmonary nodule and is positive for malignancy, PET is the most accurate modality for staging.
- Interpretation.10 A nodule is positive for malignancy if
- Standardized uptake value (SUV). SUV > 2.5
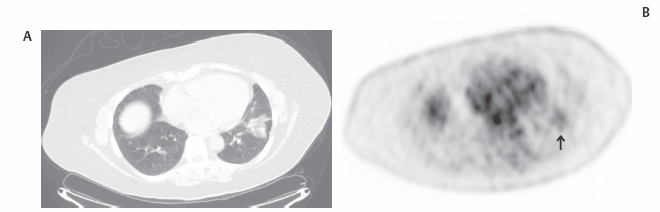
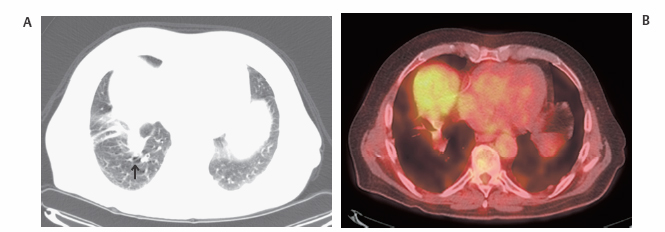
- Visual analysis. Intensity is greater than that of the mediastinum (Fig. 15.1).
- Visual and SUV analyses are comparable in accuracy.
- Lower thresholds (SUV > 2.0 and intensity equal or greater than mediastinum) have also been used successfully.3
- Small nodules. Use caution when evaluating small nodules. For nodules < 1 cm, SUV values will be substantially lower due to partial volume effects. Visual analysis threshold should also be lowered.
- If a nodule < 1 cm demonstrates any FDG uptake, it should be considered potentially malignant.11
- What size pulmonary nodule should be evaluated?
- Detection of malignancy in nodules as small as 5 mm12 has been reported. As a practical consideration, PET is best used in nodules > 1 cm in size (dynamic contrast-enhanced CT is an alternative method for nodules < 1 cm).
- However, there is limited evidence that PET may be accurate in nodules ≤ 1 cm.13
- Small nodules in the upper and anterior lungs are more optimal sites for assessment by PET than other sites because
- There is less respiratory motion in the upper lungs.
- Significant scatter from the liver in the lower lungs obscures small lesions.
- There is normal background activity in the posterior and lower lungs, particularly if the PET is acquired primarily in expiration, which may decrease the contrast between the lesion and the adjacent tissues and therefore limit detectability.
- Respiratory misregistration artifact (seen on PET/CT but not PET) can artifactually decrease uptake in lung nodules near the hemidiaphragms.
- PET could be considered in nodules < 1 cm in intermediate-risk patients if negative nodules are closely observed.14–16
- Scan time. Scanning should begin ~50 minutes after FDG injection to best separate malignant from benign lesions.17
- Dual point imaging. Imaging at 1 and 3 hours (using a threshold of 10% SUV increase for malignancy) improves accuracy.18 Malignant lesions show increased uptake on delayed images, whereas benign inflammatory lesions are stable or less active on the second scan.
- This technique may be particularly helpful for equivocal lesions with SUVs ~2.5.
- Benign lesions (in particular, granulomas) can sometimes demonstrate increasing uptake, but this is typically less than seen in malignancies. However, uptake in malignant lesions should not decrease.19
- Histology. Squamous cell carcinomas have greater FDG uptake than adenocarcinomas or large cell carcinomas.20
- Round atelectasis. Round atelectasis usually does not have FDG uptake (Fig. 15.2). PET can be used to differentiate atypical round atelectasis from malignant tumors.21
- False-positives. Active granulomatous/inflammatory process (tuberculosis, fungal infection, rheumatoid nodule, sarcoid, lipoid pneumonia, talc granulomata, inflammatory pseudotumor), benign tumors (sclerosing hemangioma, leiomyoma)22
- False-negatives. Bronchioalveolar carcinoma (particularly in lesions without an invasive component) (Fig. 15.3), differentiated adenocarcinoma, carcinoid, mucoepidermoid carcinoma,22 small lesions
- Most false-negative malignant pulmonary nodules on PET imaging are differentiated adenocarcinoma.23
- The sensitivity of PET for the multifocal form of bronchioalveolar carcinoma is substantially higher than for the solitary form.24
- The average SUV in a pulmonary carcinoid tumor is 3.0.25
- The false-negative rate may be higher if PET is used to evaluate nodules detected during screening chest CT, as these nodules, if malignant, tend to be small and/or low-grade.26
- Ground glass opacities. PET should not be used to evaluate ground glass opacities seen on CT (sensitivity 10%, specificity 20%).27
- False-negative results are common due to bronchoalveolar carcinoma.
- False-positive results are common due to pneumonia.
- Lack of CT correlate. A focus of FDG uptake in the lung should not be considered to represent a nodule if there is no CT correlate, as the latter can detect almost any nodule in the lung. This may not be true if a CT performed during respiration (as part of a PET/CT) is used for correlation, as small lung nodules may not be detected. If there is no corresponding CT lesion, consider these possibilities:
- Misregistration on PET/CT (see Chapter 7). If the study is a PET/CT, the PET uptake and lung nodule may be misregistered and appear to be in different sites from each other. In addition, a liver dome lesion could appear to be in the lung base due to misregistration (see Fig. 8.10).
- Injected clot. Injection of radioactive clot (following blood draw) in the syringe can result in pulmonary hot spots without a CT correlate (see Fig. 6.22, p. 54). A similar phenomenon is seen on pulmonary perfusion images during ventilation perfusion scans.
- Lesions with FDG uptake and SUV < 2.5. There is some evidence that lesions with SUV < 2.5 should be further stratified by level of visual uptake. In one study,23 lesions with faint or no visible uptake had a very low probability of malignancy, whereas lesions that were visually evident had a probability of malignancy of 60%, even if SUV was < 2.5. An SUV cutoff of 1.6 was proposed by the authors of this study. Another study suggests using an SUV cutoff of 2.0 for nodules < 1 cm.28 In practice, we recommend reporting discordant visual and SUV findings (e.g., visual uptake greater than mediastinum, but SUV < 2.5) as suspicious for malignancy. This is particularly true for small nodules where SUV may be artifactually low due to partial volume effects. If a nodule is not small (> 2 cm) and there is uptake less than the mediastinum and SUV < 2.5, we would report this as probably benign. Small nodules (between 1 and 2 cm) with definite uptake less than mediastinum and SUV < 2.5 are the most problematic. If the SUV is > 1.6 for these nodules, we will at least recommend very close follow-up. In addition, we would give greater weight to the CT characteristics in these nodules. Nodules < 1 cm cannot be diagnosed as benign by PET even if there is no FDG up-take.29
- Lung base nodules. PET/CT should be used with caution in nodules near the hemidiaphragms. Due to photopenic respiratory misregistration artifact (see Chapter 8), SUVs can be artifactually decreased in these nodules.
PET can be used to evaluate an indeterminate pulmonary lesion in a patient with a known primary tumor. Minimal data exist for this application of PET. Note that in this setting, a metastasis cannot be distinguished from other causes of uptake, including bronchogenic carcinoma.
Using a cutoff SUV of 2.5 or lesion-to-background ratio of 3.0, PET can distinguish a pulmonary metastasis from a benign nodule with an accuracy of 91%.30
- PET is a standard modality for staging non–small cell lung cancer (NSCLC).
- The addition of PET to the conventional work-up will prevent unnecessary surgery in one out of five patients31 and results in changing stage from that determined by conventional modalities in over half of patients.32
- PET is valuable in both mediastinal and distant staging.
- Mediastinal staging16
- PET is most useful in patients without enlarged mediastinal nodes on CT and no clinical evidence of systemic metastases.
- In patients with enlarged mediastinal nodes, PET is usually less valuable, as a negative PET may not preclude mediastinoscopy due to possible false-negative results.
- PET has a limited role in clinical stage I (peripheral) tumors, as the incidence of mediastinal metastases is low.
- Distant staging16
- PET is most useful in patients with a positive clinical evaluation suggesting systemic metastasis (clinical stage IV) or radiographic evidence of mediastinal lymph node enlargement (clinical stage III).
- In these situations, PET should be performed in conjunction with a head CT or MRI.
- PET may also be useful to detect distant metastases in patients with clinical stage II tumors (particularly central tumors or adenocarcinoma).
- PET has a limited role in clinical stage I (peripheral) tumors, as the incidence of unsuspected distant metastases is low.
- Mediastinal staging33
- PET
- PET is superior to CT for N0, N2, and N3 disease, but not N1 disease.
- PET has a lower frequency of false-positive findings in the upper mediastinal nodes.
- PET has a lower frequency of false-negative findings in adenocarcinoma and false-positive findings in squamous cell carcinoma.
- PET vs. CT34 Table 15.1
- PET/CT. PET/CT has superior accuracy to that of CT, PET alone, or visual correlation of CT and PET for tumor and nodal staging.35
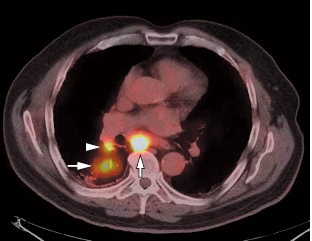
- Tumor stage. PET/CT is superior to PET for T (tumor) staging. The CT component allows for determination of tumor size and extension in adjacent soft tissues. PET/CT is ideally suited for assessing chest wall and mediastinal invasion (Fig. 15.4). The advantages of PET/CT compared with PET are probably greater for T staging than nodal staging.36
- Nodal stage. PET/CT increases confidence in diagnosing nodal disease and decreases equivocal results substantially.
- PET/CT has superior sensitivity to PET alone for left hilar, subaortic, and right paratracheal nodes and higher accuracy for subcarinal and interlobar nodes.37
- Distant staging16
- PET. PET will detect unsuspected distant metastases in ~10% of patients.32
- PET/CT. For distant metastases, PET/CT is primarily useful in determining the exact location of abnormalities noted on the FDG study.35
- Bone marrow metastases
- PET. Sensitivity 92%, specificity 99%38
- Compared with bone scintigraphy, PET is equal or greater in sensitivity and more specific for the diagnosis of bone marrow metastases from lung carcinoma (Fig. 15.5).
 Solitary Pulmonary Nodule
Solitary Pulmonary Nodule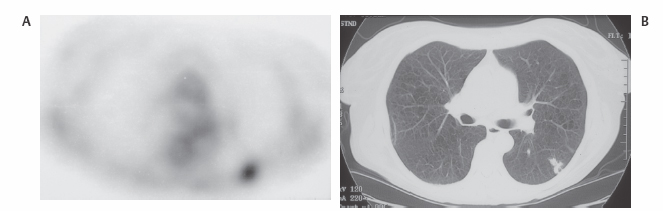
 Pulmonary Metastasis versus Benign Nodule
Pulmonary Metastasis versus Benign Nodule Staging of Non–Small Cell Lung Cancer
Staging of Non–Small Cell Lung Cancer