Chapter 6 Thoracic Trauma
The plain chest radiograph, as part of the trauma series (i.e., anteroposterior chest radiograph, anteroposterior pelvis radiograph, and cross-table lateral view of the cervical spine) is typically the initial means of diagnostic imaging for all cases of trauma. The trauma series identifies injuries that have the potential for being immediately life threatening (e.g., tension pneumothorax) or iatrogenic insults that may occur from the injudicious placement of tubes and lines during resuscitation (e.g., right mainstem bronchus intubation) (Box 6-1). However, the importance of chest radiography for clearing major chest trauma victims has considerably diminished, and computed tomography (CT) has become the primary imaging modality for all hemodynamically stable trauma patients. This represents a rather significant change in practice compared with less than a decade ago.
INJURIES TO THE CHEST WALL
Rib Fractures
Injuries to the chest wall, particularly rib fractures, are common (Box 6-2). The complications of rib fractures, such as pneumothorax and splenic injury, are often of greater consequence than the fractures themselves. Rib fractures are frequently not detected on the initial chest radiograph because an undisplaced or minimally displaced fracture, or a costovertebral separation are radiographically occult. Multiple rib views are not necessary because the treatment for clinically suspected rib fractures is the same whether they are shown by radiography or not. In children, rib fractures are uncommon because of the elasticity of the cartilage. The presence of multiple rib fractures, particularly if of various ages or if posteriorly located is strongly suggestive of child abuse. In adults, multiple, bilateral, healed or healing fractures are often associated with repeated falls and frequently indicate alcoholism or chronic drug use.
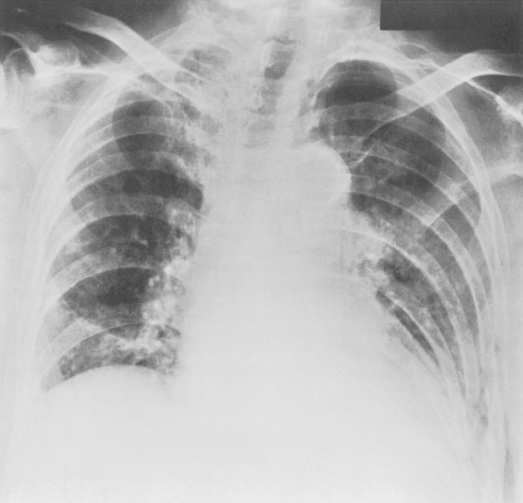
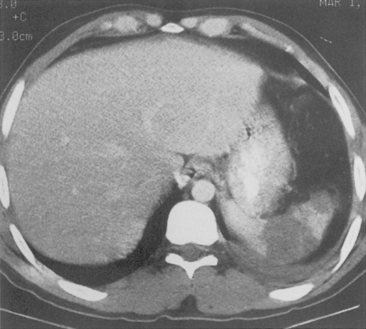
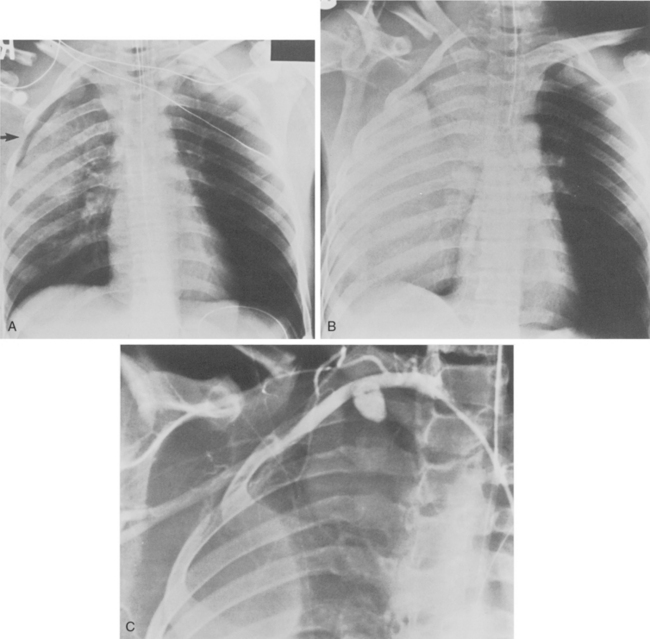
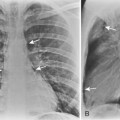
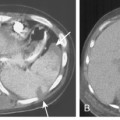
Rib fractures are an important indicator of the trauma mechanism, providing information about the vector and severity of the applied forces, as well as indicating the possible complications (Fig. 6-1). Fractures of the first three ribs raise concern for more severe traumatic injury since these can be associated with airway, spinal, or vascular injury (Table 6-1). Ninety percent of patients with tracheobronchial injury have rib fractures at this site. However, only 3% to 15% of patients with upper rib fractures have brachial plexus or vascular injury; CT’s ability to effectively screen for these injuries permits the highly selective use of other modalities. For example, angiography is reserved for those patients for whom clinical or CT findings are inconclusive or warrant a more specific approach to investigation. Fractures of the lower three ribs should raise suspicion for splenic, hepatic, or renal trauma (Fig. 6-2) and should prompt an abdominal CT study to evaluate for these solid visceral injuries (Fig. 6-3).
| Location | Associations or Complications |
|---|---|
| First three pairs | Spinal or vascular injury, tracheobronchial rupture |
| Last three pairs | Hepatic, splenic, renal injury |
| Multiple sites | Flail chest |
| Multiple healed, adult | Alcoholism |
| Multiple healed, child | Child abuse |
Several plain chest radiographic findings may indicate splenic trauma. Displacement of the gas-filled fundus of the stomach medially and anteriorly by hematoma and/or signs of left diaphragmatic rupture indicate a greater likelihood of splenic injury. Segmental rib fractures involving more than three contiguous ribs or single fractures involving five consecutive ribs constitute a flail chest (Fig. 6-4). Severe respiratory compromise may develop as a result of the paradoxical movement of the flail segment during respiration. For this reason some institutions have begun to perform open reduction internal fixation (ORIF) of flail segments using hardware plates.
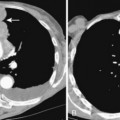
Extrapleural hematomas frequently accompany rib fractures. On the chest radiograph, the hematoma may appear as a focal, lobulated opacity that has a convex margin with the lung. Unlike pleural fluid, these hematomas do not alter configuration with changes in patient position. Extrapleural hematoma at the apices may be caused by subclavian vessel hemorrhage as a result of the initial trauma or after central line placement (Fig. 6-5). Aortic injury can also result in a left apical extrapleural hematoma, manifest as increased opacity above the left lung apex. More inferiorly, extrapleural hematoma is usually the result of injury to intercostal vessels. Hemorrhage from intercostal vessels may result in a rapidly developing hemothorax, or even exsanguination. Angiography with embolization can be life saving (Fig. 6-6).
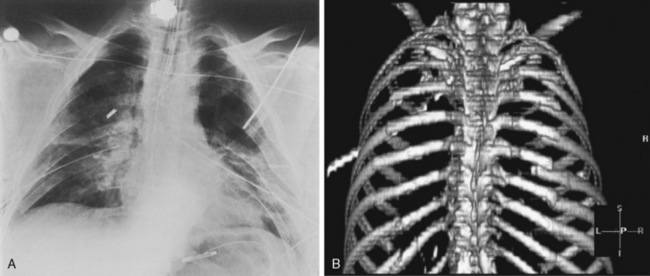
Sternal Fractures
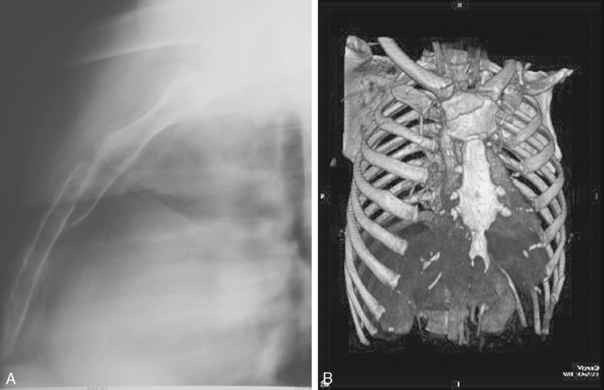
Sternal fractures occur in less than 10% of patients with major thoracic trauma and may be associated with injury to the mediastinal vascular structures or myocardial contusion, the diagnosis was most easily made on the lateral chest radiograph (Fig. 6-7A). Today, coronal or sagittal reformations or three-dimensional renderings of the chest CT readily show sternal fracture as well as the degree of fracture displacement (see Fig. 6-7B). Sternoclavicular dislocations can be difficult to identify on the chest radiograph, but CT can readily show them. Most dislocations are anterior and are of little clinical significance. Posterior dislocations are more concerning given their greater association with injuries to adjacent mediastinal vessels, trachea, and esophagus.
Spinal Injury
Spinal injury is common in cases of high-velocity trauma where up 30% of patients with significant thoracic trauma have spinal injuries. More than 60% of fracture dislocations in the thoracic spine are associated with neurologic defects. This compares with a prevalence of 32% in the cervical spine and 2% in the lumbar spine (Box 6-3). Early identification of spinal fractures may prevent irreversible and potentially devastating cord injury. Thoracic spine radiographs are not necessary for trauma patients who have undergone volumetric chest CT. Studies have shown that coronal and sagittal reformatted images are more sensitive, specific, and accurate for detecting and characterizing spinal injuries. Most fracture dislocations occur at the thoracolumbar junction (Fig. 6-8). Multiple fractures are found in 10% of patients and eighty percent of these injuries are noncontiguous. The radiologic features to be considered include abnormal vertebral shape, location, size, and density. The “rule of 2 s” applies (Box 6-4).
Box 6-3 Thoracic Spinal Injury
Occurs frequently with high-velocity injury
10% of patients have multiple fractures
80% of multiple fractures are noncontiguous
60% of fracture dislocations are associated with complete neurologic defect
Box 6-4 Rule of 2s for Normal Spinal Dimensions
Posterior vertebral height is less than 2 mm greater than the anterior height (except T11 and T12).
Facet joint width is less than 2 mm.
Transverse interpedicular distance of contiguous vertebrae has a less than 2 mm difference.
Vertical interpedicular distance of contiguous vertebrae has a less than 2 mm difference.
Interspinous distance of adjacent vertebrae has a less than 2 mm difference.
INJURY TO THE TRACHEA AND MAJOR AIRWAYS
Tracheobronchial Rupture
Tracheobronchial injury is frequently associated with fractures or dislocations to the upper thoracic cage. The tear may be partial or complete. The diagnosis is frequently delayed, resulting in tracheal or bronchial stenosis from partial healing. The early diagnostic features include persistent severe pneumomediastinum, subcutaneous emphysema, and pneumothorax (Box 6-5). Uncommon signs of rupture include the fallen lung sign, bayonet deformity of the trachea, and ectopic position of the endotracheal tube or balloon cuff.
Bronchial Rupture
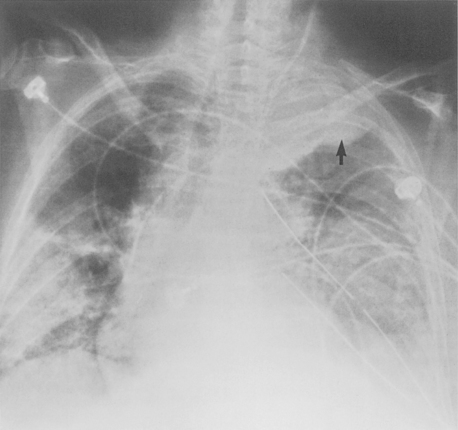
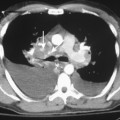
Bronchial rupture occurs within 2.5 cm of the carina in 80% of patients. Right-sided rupture is more common than left, and most patients develop a pneumothorax. Pneumomediastinum, however, may be the only finding, particularly with injury to the left main bronchus, which has a longer extrapleural course in the mediastinum. Bronchial rupture that occurs within the pleural space leads to pneumothorax that is usually large and fails to resolve despite tube drainage because of the persistent air leak (Fig. 6-14). The fallen lung sign occurs with complete disruption of the main stem bronchus (Fig. 6-9). The detached lung segment falls inferiorly and laterally to the base of the hemithorax. This contrasts with a pneumothorax from a partial bronchial tear, for which the lung typically collapses medially and centrally toward its attachment. In both instances the lung fails to reexpand on chest tube drainage. A missed partial bronchial tear should be suspected if there is persistent lobar atelectasis or air trapping in the affected lung.
PLEURAL ABNORMALITIES
Pneumothorax
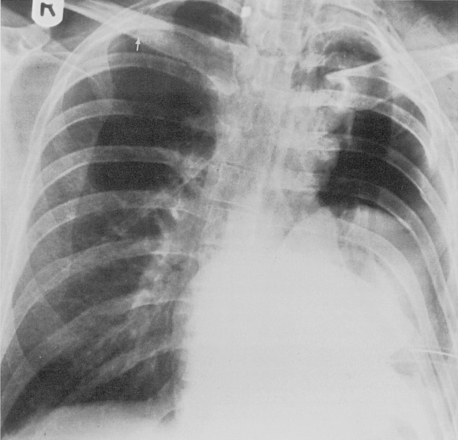
A pneumothorax occurs twice as often in patients with blunt trauma as in those with a penetrating injury. The identification of even a small pneumothorax is important, because a rapid increase in size of the pneumothorax may occur in mechanically ventilated patients. Because most chest radiographs are performed with the patient in the supine position, it may be difficult to recognize even a large pneumothorax. Air collects in the most nondependent regions; in the supine position air collects in an anterior and often inferior location and results most commonly in the deep sulcus sign (Box 6-6 and Fig. 6-10). On an erect radiograph, identification of the visceral pleural edge with absence of lung vessels peripherally is diagnostic (Fig. 6-11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree