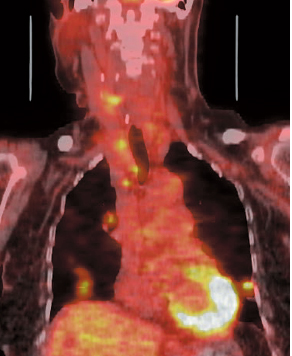
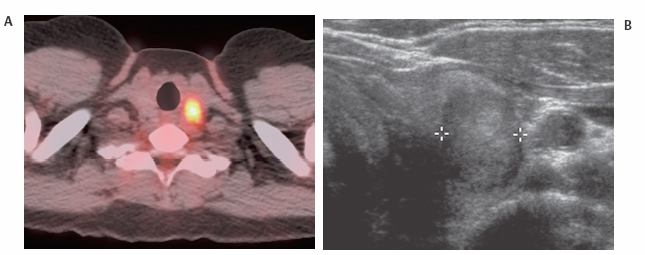
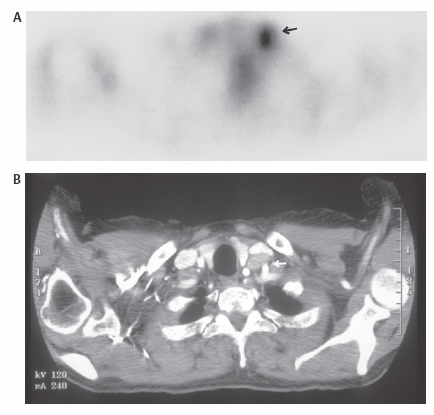
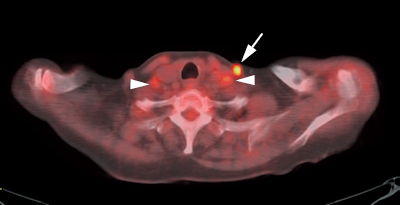
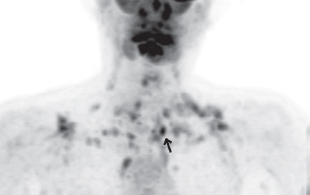
14 Positron emission tomography (PET) has a limited role in primary evaluation of thyroid nodules. However, uptake in thyroid nodules is often seen as an incidental finding (Fig. 14.1). Fig. 14.1 Thyroid nodule. (A) Axial positron emission tomography/computed tomography scan demonstrates focal uptake in the left thyroid. (B) Ultrasound confirms the presence of a left thyroid nodule. Fig. 14.2 Medial neck node mimicking a thyroid nodule. (A) Focal uptake in the left neck (arrow) on axial positron emission tomography scan is suspicious for a thyroid nodule. (B) Computed tomography scan demonstrates a medial node (arrow) immediately lateral to the left thyroid lobe, corresponding to the area of fluorodeoxyglucose uptake. Conversely, a thyroid nodule can mimic a medial neck node. Localizing metastatic disease in patients with an elevated thyroglobulin and negative radio-iodine whole-body scan is the primary clinical indication for PET in thyroid cancer (Figs. 14.3, 14.4, and 14.5). Fig. 14.4 Muscle uptake and nodal metastases. Axial positron emission tomography/computed tomography scan demonstrates increased uptake in a left neck node (arrow) secondary to metastatic thyroid cancer. Note the proximity of the node to muscle uptake (arrowheads). Fig. 14.5 Brown fat uptake and nodal metastases. Extensive brown fat uptake in the neck, supraclavicular regions, and superior mediastinum on a coronal positron emission tomography (PET) scan severely limits evaluation in a patient with suspected metastatic thyroid cancer. A single superior mediastinal nodal metastasis (arrow) was present. This is slightly more intense than the brown fat uptake but otherwise similar in appearance. PET/computed tomography was necessary to identify this node.
Thyroid Cancer
Eugene C. Lin and Abass Alavi
 Thyroid Nodules
Thyroid Nodules
Clinical Indication: C
Accuracy: Differentiating Benign from Malignant Nodules
Pearls
Pitfalls
 Recurrent Thyroid Cancer10–12
Recurrent Thyroid Cancer10–12
Clinical Indication: B
Accuracy
Comparison with Other Modalities
Sensitivity %
Specificity %
PET
75
90
Iodine 131
50
99
Sestamibi/thallium
53
92
Pearls
- Thyroglobulin level. In patients with a negative radioiodine whole-body scan and elevated thyroglobulin, PET is most useful at thyroglobulin levels > 10 ng/mL.28
Table 14.2 Sensitivity and specificity of Positron Emission Tomography Compared with Other Modalities in Medullary Thyroid Cancer
Sensitivity
%
Specificity
%
PET
78
79
Somatostatin receptor
25
92
Scintigraphy
Dimercaptosuccinic
33
78
acid
Sestamibi
25
100
CT
50
20
MRI
82
67
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging; PET, positron emission tomography.
- Thyroid hormone withdrawal/recombinant thyroid-stimulating hormone (TSH). Although radioiodine imaging is most helpful when performed in patients with elevated TSH levels (thyroid hormone withdrawal or recombinant TSH administration), there are several other factors to consider with FDG PET imaging:
- Although thyroid carcinomas may increase their metabolic demand after TSH stimulation, the tumors that have FDG uptake are usually poorly differentiated and may be less dependent upon TSH.
- A TSH-stimulated hypothyroid state can decrease metabolic organ activity and may decrease metabolic activity in tumor cells.
- Although thyroid carcinomas may increase their metabolic demand after TSH stimulation, the tumors that have FDG uptake are usually poorly differentiated and may be less dependent upon TSH.
- Thyroid hormone withdrawal. Conflicting studies indicate both increased and decreased sensitivity with an elevated TSH after thyroid hormone withdrawal.17,29,30
- The discrepant results may represent the conflicting effects of increased tumor metabolism from TSH stimulation and decreased metabolism from hypothyroidism.
- Recombinant TSH. Lesion detectability is greater with recombinant TSH compared with TSH suppression.31 Using recombinant TSH has two advantages over thyroid hormone withdrawal: patients are spared a prolonged hypothyroid state, and the possible negative effects of hypothyroidism on tumor FDG uptake are avoided. However, given the substantial cost of recombinant TSH, it is unclear whether this is cost-effective in most clinical settings.
- Thyroglobulin and TSH. In patients with a thyroglobulin > 100 ng/mL, TSH stimulation is probably not necessary due to the high sensitivity of PET in this subpopulation.32
Pitfalls
- Pulmonary metastases. PET has poor sensitivity for pulmonary metastases from thyroid cancer < 1 cm. If pulmonary metastases are of clinical concern, a chest CT should be performed.
- Muscle/brown fat. Neck muscle or brown fat uptake can be mistaken for cervical or mediastinal nodal disease (Figs. 14.4 and 14.5). Anatomical correlation is necessary to avoid such errors; this is particularly important in thyroid cancer, where the prevalence of cervical node disease is high.
- Vocal cord. Unilateral vocal cord activity can cause false-positive results (as seen in Fig. 6.14, p. 49).
References
- Kresnik E, Gallowitsch HJ, Mikosch P, et al. Fluorine-18-fluorodeoxyglucose positron emission tomography in the preoperative assessment of thyroid nodules in an endemic goiter area. Surgery 2003;133(3):294–299
- Bloom AD, Adler LP, Shuck JM. Determination of malignancy of thyroid nodules with positron emission tomography. Surgery 1993;114(4):728–734
- Bogsrud TV, Karantanis D, Nathan MA, et al. The value of quantifying 18F-FDG uptake in thyroid nodules found incidentally on whole-body PET-CT. Nucl Med Commun 2007;28(5):373–381
- de Geus-Oei LF, Pieters GF, Bonenkamp JJ, et al. 18F-FDG PET reduces unnecessary hemithyroidectomies for thyroid nodules with inconclusive cytologic results. J Nucl Med 2006;47(5):770–775
- Mitchell JC, Grant F, Evenson AR, et al. Preoperative evaluation of thyroid nodules with 18FDG-PET/CT. Surgery 2005;138(6):1166–1174
- Kim JM, Ryu JS, Kim TY, et al. 18F-fluorodeoxyglucose positron emission tomography does not predict malignancy in thyroid nodules cytologically diagnosed as follicular neoplasm. J Clin Endocrinol Metab 2007;92(5):1630–1634
- Chen YK, Ding HJ, Chen KT, et al. Prevalence and risk of cancer of focal thyroid incidentaloma identified by 18F-fluorodeoxyglucose positron emission tomography for cancer screening in healthy subjects. Anticancer Res 2005;25(2B):1421–1426
- Kang KW, Kim SK, Kang HS, et al. Prevalence and risk of cancer of focal thyroid incidentaloma identified by 18F-fluorodeoxyglucose positron emission tomography for metastasis evaluation and cancer screening in healthy subjects. J Clin Endocrinol Metab 2003;88(9):4100–4104
- Choi JY, Lee KS, Kim HJ, et al. Focal thyroid lesions incidentally identified by integrated 18F-FDG PET/CT: clinical significance and improved characterization. J Nucl Med 2006;47(4):609–615
- Haugen BR, Lin EC. Isotope imaging for metastatic thyroid cancer. Endocrinol Metab Clin North Am 2001;30(2):469–492
- Larson SM, Robbins R. Positron emission tomography in thyroid cancer management. Semin Roentgenol 2002;37(2):169–174
- Zhuang H, Kumar R, Mandel S, Alavi A. Investigation of thyroid, head, and neck cancers with PET. Radiol Clin North Am 2004;42(6):1101–1111 viii.
- Pryma DA, Schoder H, Gonen M, et al. Diagnostic accuracy and prognostic value of 18F-FDG PET in Hürthle cell thyroid cancer patients. J Nucl Med 2006;47(8):1260–1266
- Diehl M, Graichen S, Menzel C, et al. F-18 FDG PET in insular thyroid cancer. Clin Nucl Med 2003;28(9):728–731
- Diehl M, Risse JH, Brandt-Mainz K, et al. Fluorine-18 fluorodeoxyglucose positron emission tomography in medullary thyroid cancer: results of a multicentre study. Eur J Nucl Med 2001;28(11):1671–1676
- Wang W, Larson SM, Fazzari M, et al. Prognostic value of [18F]fluorodeoxyglucose positron emission tomographic scanning in patients with thyroid cancer. J Clin Endocrinol Metab 2000;85(3):1107–1113
- Grunwald F, Kalicke T, Feine U, et al. Fluorine-18 fluorodeoxyglucose positron emission tomography in thyroid cancer: results of a multicentre study. Eur J Nucl Med 1999;26(12):1547–1552
- Palmedo H, Bucerius J, Joe A, et al. Integrated PET/CT in differentiated thyroid cancer: diagnostic accuracy and impact on patient management. J Nucl Med 2006;47(4):616–624
- Chung JK, So Y, Lee JS, et al. Value of FDG PET in papillary thyroid carcinoma with negative 131I whole-body scan. J Nucl Med 1999;40(6):986–992
- Jeong HS, Baek CH, Son YI, et al. Integrated 18F-FDG PET/CT for the initial evaluation of cervical node level of patients with papillary thyroid carcinoma: comparison with ultrasound and contrast-enhanced CT. Clin Endocrinol (Oxf) 2006;65(3):402–407
- Ito S, Kato K, Ikeda M, et al. Comparison of 18F-FDG PET and bone scintigraphy in detection of bone metastases of thyroid cancer. J Nucl Med 2007;48(6):889–895
- Rodrigues M, Li S, Gabriel M, et al. 99mTc-depreotide scintigraphy versus 18F-FDG-PET in the diagnosis of radioiodine-negative thyroid cancer. J Clin Endocrinol Metab 2006;91(10):3997–4000
- Wang W, Larson SM, Tuttle RM, et al. Resistance of [18F]-fluorodeoxyglucose-avid metastatic thyroid cancer lesions to treatment with highdose radioactive iodine. Thyroid 2001;11(12):1169–1175
- Salvatore B, Paone G, Klain M, et al. Fluorodeoxyglucose PET/CT in patients with differentiated thyroid cancer and elevated thyroglobulin after total thyroidectomy and (131)I ablation. Q J Nucl Med Mol Imaging 2008;52(1):2–8
- Shiga T, Tsukamoto E, Nakada K, et al. Comparison of (18)F-FDG, (131)I-Na, and (201)Tl in diagnosis of recurrent or metastatic thyroid carcinoma. J Nucl Med 2001;42(3):414–419
- Phan HT, Jager PL, Plukker JT, Wolffenbuttel BH, Dierckx RA, Links TP. Detection of bone metastases in thyroid cancer patients: bone scintigraphy or 18F-FDG PET? Nucl Med Commun 2007;28(8):597–602
- Ong SC, Schoder H, Patel SG, et al. Diagnostic accuracy of 18F-FDG PET in restaging patients with medullary thyroid carcinoma and elevated calcitonin levels. J Nucl Med 2007;48(4):501–507
- Schluter B, Bohuslavizki KH, Beyer W, et al. Impact of FDG PET on patients with differentiated thyroid cancer who present with elevated thyroglobulin and negative 131I scan. J Nucl Med 2001;42(1):71–76
- Grunwald F, Biersack HJ. FDG PET in thyroid cancer: thyroxine or not? J Nucl Med 2000;41(12):1996–1998
- van Tol KM, Jager PL, Piers DA, et al. Better yield of (18)fluorodeoxyglucose-positron emission tomography in patients with metastatic differentiated thyroid carcinoma during thyrotropin stimulation. Thyroid 2002;12(5):381–387
- Chin BB, Patel P, Cohade C, et al. Recombinant human thyrotropin stimulation of fluoro-D-glucose pos itron emission tomography uptake in well-differentiated thyroid carcinoma. J Clin Endocrinol Metab 2004; 89(1):91–95
- Stokkel MP, Duchateau CS, Dragoiescu C. The value of FDG-PET in the follow-up of differentiated thyroid cancer: a review of the literature. Q J Nucl Med Mol Imaging 2006;50(1):78–87
- Bloom AD, Adler LP, Shuck JM. Determination of malignancy of thyroid nodules with positron emission tomography. Surgery 1993;114(4):728–734
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree