Key Points
- •
Recognizing normal thyroid gland anatomy and architecture is important for providers utilizing ultrasound at the bedside.
- •
Thyroid nodules are common, but nodules with concerning findings by ultrasound, such as hypoechogenicity, irregular or infiltrative margins, microcalcifications, and increased intranodular flow, should undergo further workup with fine-needle aspiration.
- •
Ultrasound-guided fine-needle aspiration is a safe procedure with minimal complications and is the method of choice for definitive evaluation of thyroid nodules.
Background
A thyroid nodule is a discrete lesion within the normal thyroid parenchyma. Widespread use of neck ultrasound and other anatomic imaging modalities has led to an increase in the diagnosis of thyroid nodules.
Thyroid nodules are common but few are malignant. In iodine-sufficient countries, prevalence of a palpable thyroid nodule is 5% in women and 1% in men. However, high-resolution thyroid ultrasound is able to detect thyroid nodule in 19–67% of randomly selected individuals.
Some nodules identified with ultrasound require evaluation with fine-needle aspiration (FNA) to exclude cancer, but most small thyroid nodules can be monitored over time with ultrasound. Several factors should be considered to determine which nodules should undergo FNA, including nodule size, ultrasound appearance, and high-risk history. High-resolution thyroid ultrasound is the method of choice to evaluate thyroid nodules, and the American Thyroid Association recommends that thyroid ultrasonography be performed in all patients with a thyroid nodule. Ultrasound features of thyroid nodules that need to be evaluated include echogenicity, structure, vascularity, calcifications, margins, and shape.
Ultrasound-guided FNA is widely accepted as the method of choice for the evaluation of thyroid nodules that meet criteria for biopsy. Using ultrasound guidance for FNA improves the rate of obtaining an adequate biopsy specimen and lowers the rate of false-negative results when compared to palpation-guided FNA.
Normal Anatomy
The thyroid gland is an encapsulated organ located in the anterior mid portion of the neck, inferior to the cricoid cartilage. The thyroid gland is composed of two lobes that are connected by an isthmus. The sternocleidomastoid muscle and carotid sheath are lateral to the thyroid gland. The strap muscles (sternohyoid, sternothyroid, and omohyoid) are anterior to the thyroid gland. The longus colli muscles are posterior and the trachea is posteromedial to the thyroid gland. The esophagus can be seen adjacent to the trachea, posterior to the left lobe of the thyroid. Peristalsis can be seen when the patient swallows, which helps to differentiate the esophagus from a thyroid nodule ( Figure 32.1 ).
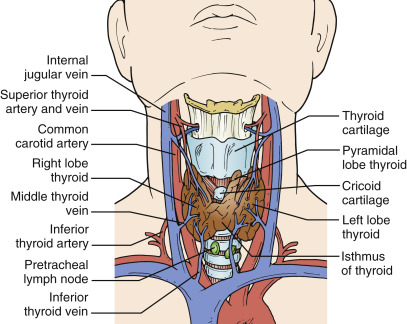
Image Acquisition
A high-frequency linear transducer should be used to image the thyroid gland. Images should be obtained in both the transverse and sagittal planes ( Figure 32.2 ). A high-frequency transducer provides excellent axial and lateral resolution of the superficial neck structures, including the thyroid gland, lymph nodes, and blood vessels. However, a lower-frequency transducer may be necessary when structures are deep in the neck in morbidly obese patients or in the setting of a large multinodular goiter. Thyroid lobes and nodules should be measured in three dimensions: depth (anterior-posterior), width (transverse), and length (superior-inferior). In the transverse imaging plane, depth is measured at the maximal anterior-posterior distance, and width is measured from the lateral edge of the trachea to the lateral border of the thyroid lobe. A normal thyroid gland is 2 cm or less in both anterior-posterior (depth) and transverse (width) dimensions. Length is measured in the sagittal imaging plane from the cranial to caudal border of the thyroid lobe and is normally 4.5–5.5 cm ( Figure 32.3 ).
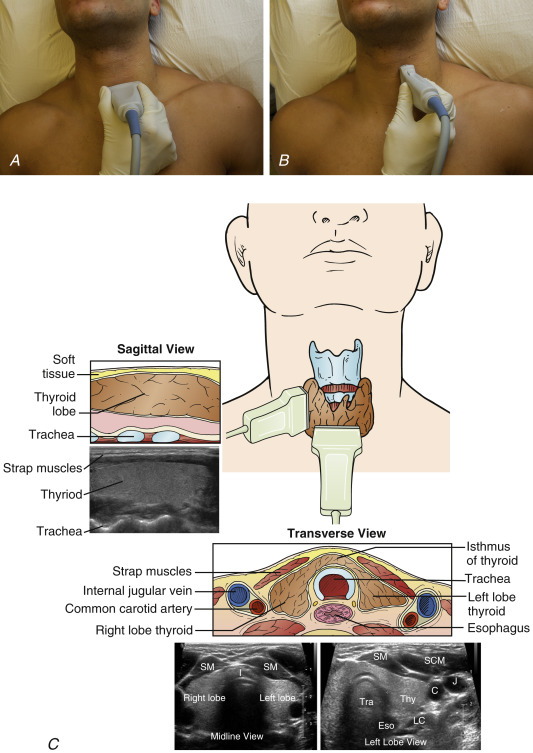
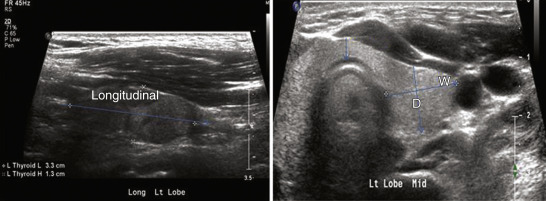
Image Interpretation
Thyroiditis
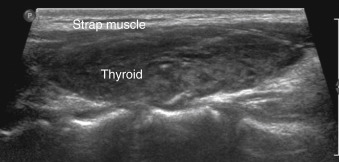
Normal thyroid gland parenchyma is homogeneous and hyperechoic when compared to the surrounding strap muscles.
The ultrasound appearance of thyroid tissue changes in diffuse autoimmune thyroid disorders, such as Hashimoto’s thyroiditis. The thyroid parenchyma in Hashimoto’s thyroiditis appears heterogeneous with patchy hypoechoic and hyperechoic areas. Thyroid size may be normal, enlarged, or small, with variable vascularity depending on duration of disease. Ultrasound findings manifest the underlying histologic changes, primarily diffuse infiltration of the gland with lymphocytes and fibrosis ( Figure 32.4 ).
Thyroid Nodules
The following characteristics should be described in the evaluation of a thyroid nodule: nodule size in three dimensions, echogenicity (isoechoic, hypoechoic, or hyperechoic), structure (solid, mixed, or cystic), margins (well-defined, irregular, or infiltrative), calcifications (microcalcifications, macrocalcifications, or eggshell calcifications), vascularity (absent, peripheral, or intranodular), and shape (round, tall).
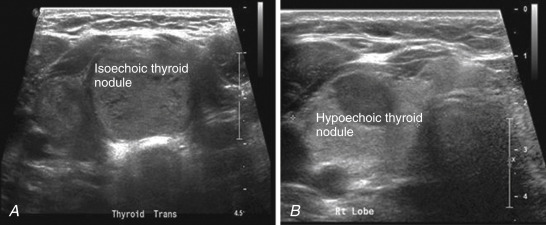
Echogenicity
Echogenicity is the brightness of thyroid nodules in comparison to normal thyroid parenchyma. Nodules are described as isoechoic (same echogenicity as surrounding thyroid tissue), hypoechoic (darker than surrounding thyroid tissue), or hyperechoic (brighter than surrounding thyroid tissue) ( Figure 32.5 ). Hypoechoic nodules are associated with malignancy. In a series published by Kim et al., 26.5% of malignant nodules were hypoechoic in comparison to 5.6% of benign nodules. Kim reported sensitivity of 26.5% and specificity of 94.3% for hypoechogenicity correlating with malignancy.
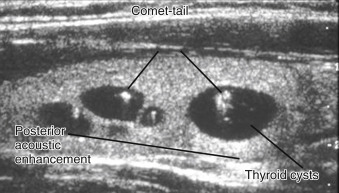
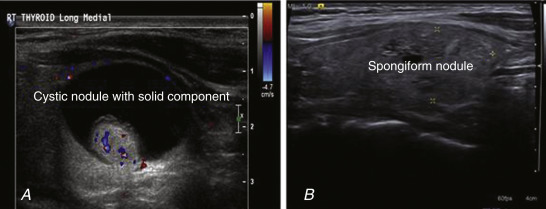
Structure
The structure of nodules is important to note during ultrasound evaluation. A pure cyst is anechoic with bright signal posterior to the cyst (posterior acoustic enhancement). A pure cyst is always benign and does not require further evaluation with FNA. A colloid cyst often contains comet-tail artifact, which is an echogenic focus with reverberation ( Figure 32.6 ). A mixed cystic and solid nodule may show a honeycomb or spongiform appearance, which is highly specific for benign nodule. Some nodules have a focal cystic component due to degeneration of a colloid nodule, and FNA should be considered in order to rule out cystic papillary thyroid carcinoma ( Figure 32.7 ). When a nodule is predominantly cystic, there is an increased rate of nondiagnostic FNA specimens because samples contain avascular debris and fibrosis rather than follicular cells. When performing FNA, providers must focus on sampling solid areas that contain follicular cells.
Margins
Margins of a nodule may be smooth and well defined or irregular and should be evaluated with ultrasound. Spiculated or irregular margins are associated with an increased risk of malignancy. Moon et al. reported that 48.3% of malignant thyroid nodules had spiculated margins, whereas only 8.2% of benign nodules had spiculated margins.
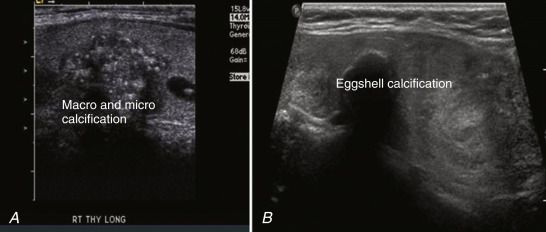
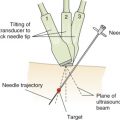
Calcifications
Calcifications are seen in almost one third of thyroid nodules. Calcification in thyroid nodules can appear as microcalcifications (<1 mm) without acoustic shadowing, rim (eggshell) calcifications, or macrocalcifications (>2 mm) with acoustic shadowing ( Figure 32.8 ). Microcalcifications are associated with an increased risk of malignancy because they often represent the psammoma bodies that are frequently seen in papillary thyroid carcinoma. Larger calcifications are often the result of degeneration and necrosis within a thyroid nodule and are more commonly seen in benign nodules. However, presence of any type of calcification increases the risk of malignancy. Eggshell calcifications can be seen in both malignant and benign nodules. In malignant lesions, eggshell calcifications may be interrupted.