Case presentation
An 11-year-old female presents with severe right-sided abdominal pain that began 5 days ago. The patient reports that she was in her usual state of good health until she experienced the pain, which initially seemed generalized, intermittent, and achy but has become more constant, sharp, and now is located primarily in the right lower quadrant. She developed a fever to 102 degrees Fahrenheit 2 days ago. She reports nausea but no emesis, diarrhea, hematuria, or trauma; she endorses dysuria. She also states that she had right flank pain several days ago, which has now resolved. She is generally healthy but does have a history of frequent urinary tract infections and at the age of 2 years had ureteral reimplant surgery on the right side for vesicoureteral reflux. She began her menses several months ago, but this has been somewhat irregular and occasionally associated with bilateral lower quadrant pain.
Examination reveals a visibly uncomfortable child who complains of right lower quadrant pain. She is afebrile, has a heart rate of 118 beats per minute, a respiratory rate of 20 breaths per minute, and a blood pressure of 120/80 mm Hg. She has focal right lower quadrant pain to palpation, with moderate guarding and rebound. There is no costovertebral tenderness. There are no signs of trauma.
Laboratory values demonstrate a total peripheral white blood cell (WBC) count of 11,000 cc/mm, a C-reactive protein level of 2.4 mg/dL, and a urinalysis with + nitrite, 1+ leukocyte esterase, few WBCs, and few bacteria.
Imaging considerations
Since the diagnosis of tubo-ovarian abscess (TOA) requires the presence of an inflammatory mass, imaging is usually employed.
Plain radiography
Plain radiography may be employed as an imaging modality during the evaluation of abdominal pain but is not helpful in identifying TOA.
Ultrasound (US)
US is often employed as a first-line imaging modality in adolescent patients with abdominal pain. , The general availability, rapidity of the study, and lack of ionizing radiation make this an attractive means to evaluate reproductive organs. US is useful in detecting ovarian pathology (torsion, cysts, masses) and pregnancy, both intrauterine and ectopic.
Transvaginal US is the imaging modality of choice when a TOA is suspected (or transabdominal US with a full bladder). In one study, 89% of patients with suspected ovarian pathology had imaging studies performed, and of these, 97% were pelvic US. A TOA appears as a complex multilocular cystic mass with thick irregular walls, partitions, and internal echoes. , The sensitivity of transvaginal and transabdominal US for the diagnosis of TOA has been reported to be 75% and 83%, respectively.
Computed tomography (CT)
This modality is often employed when there is suspicion for complex disease or an alternative diagnosis is under consideration, such as appendicitis or an inflammatory bowel process. CT may have an advantage over US in the visualization of a TOA. Compared to US, CT may have increased sensitivity to detect a TOA (78% to 100% vs. 75% to 82%, respectively) and improved specificity (100% to 91%). , Frequent findings of a TOA on CT include unilateral location (73%), multilocularity (89%), and thick, uniform, enhancing walls; less common findings included bowel thickening (59%), uterosacral ligament thickening (64%), and pyosalpinx (50%). , , A TOA appears on CT imaging as a multilocular, septate, cystic mass surrounded by a thick enhancing wall. CT, though, requires the use of intravenous (IV) contrast material and exposes the patient to ionizing radiation.
Magnetic resonance imaging (MRI)
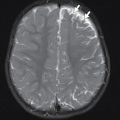
MRI can detect TOA. The abscess appears as a uni- or multilocular adnexal mass with thick and intensely enhancing walls, with low signal intensity on T1-weighted images and heterogeneous high signal intensity on T2-weighted images, although this may vary depending on the protein content of the abscess. Thick walls, multiple internal septa, and lymphadenopathy may also be seen. This modality is typically not employed as a first-line imaging modality in patients with suspected TOA but may be utilized if there is concern for a more complex infection or underlying genitourinary anatomic abnormalities.
Imaging findings
Initially, a limited abdominal US of the right lower quadrant was obtained to look for appendicitis. The appendix was identified and was normal. Because the patient has started her menstrual cycles and due to the previous report of right lower quadrant pain associated with these cycles, a pelvic US was obtained (transabdominal with a full bladder); there are several images presented here. The right ovarian borders are difficult to visualize, but there is a complex 7.1 × 6.3 × 6.0-cm mass-like structure in the right adnexa, containing the ovary, with a peripherally positioned dilated fluid-filled tubular structure. The left ovary measures 3.9 × 2.4 × 2.5 cm. Color-flow with spectral Doppler analysis shows normal arterial and venous blood flow to both ovaries ( Figs. 26.1–26.3 ). Although the findings are not specific, the right ovary does not appear normal and differential considerations include an ovarian torsion (arterial flow on Doppler examination of an ovary does not exclude ovarian torsion) or an infectious process.



Case conclusion
Pediatric Surgery was consulted to evaluate the patient in the emergency department. The decision was made to obtain an IV contrast-enhanced CT scan, since the history, physical examination, and US results were not specific and better visualization of the ovary and surrounding structures was desired. Select images from this study are presented here. These images demonstrate that the right ovary is large, with ill-defined borders, with a large dilated tubular structure around the right ovary, and surrounding edema is also seen ( Fig. 26.4 and 26.5 ).