Fig. 6.1
Embryonic bladder and relationships with the ureters, male reproductive structures, and urethral components
The bladder is an extraperitoneal structure centrally positioned in the pelvis with three fixed landmarks important in bladder ultrasound:
1.
The bladder base or trigone
2.
The ureters, which enter the trigone approximately 2 cm lateral to the midline on each side
3.
The bladder neck which is seen as a slightly open funnel at the base of the bladder
Identification of these landmarks allows for descriptive interpretation of prostate pathology as well as localization for TRUS biopsy.
Prostate and Accessory Glands
The seminal vesicles are of mesodermal origin. They differentiate during the 12th week of embryonic development from the mesonephric (Wolffian) duct near where they open into the urogenital sinus (Fig. 6.2). The prostate has both an endodermal and mesodermal origin. The glandular elements differentiate from the prostatic part of the urogenital sinus (endodermal) during the 12th week. The stroma and smooth muscle differentiate from mesodermal cells under the influence of dihydrotestosterone. The 12th week is also punctuated by the genesis of the bulbourethral (Cowper’s) and urethral (Littré’s) glands, which differentiate from protrusions along the urethra (endodermal).
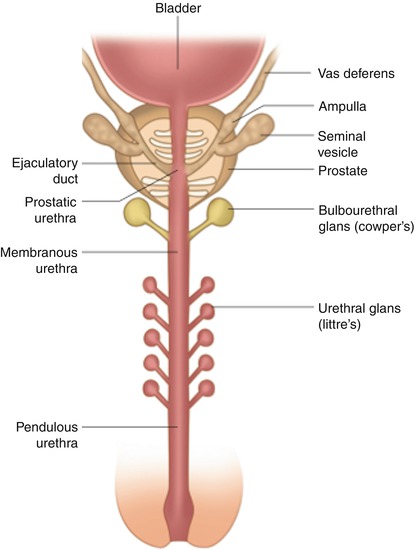
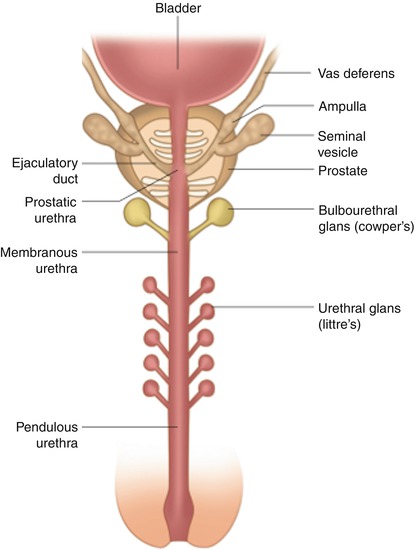
Fig. 6.2
The prostate and accessory glands of the urethra
The prostate is a retroperitoneal structure lying anterior to the rectum and inferior to the bladder, and it is separated from the rectum by an obliterated peritoneal plane (Denonvilliers’ fascia). Lateral to the prostate are the levator ani and obturator internus muscles.
The “prostatic capsule” is not a true fibroelastic capsule, but rather periprostatic fat and stroma well visualized with ultrasound.
Vasculature
The prostate and seminal vesicles are supplied by the inferior vesical, internal pudendal, and middle rectal arteries (Fig. 6.3). The seminal vesicles are also supplied by a branch of the superior vesicle artery, the vesiculo-deferential artery.
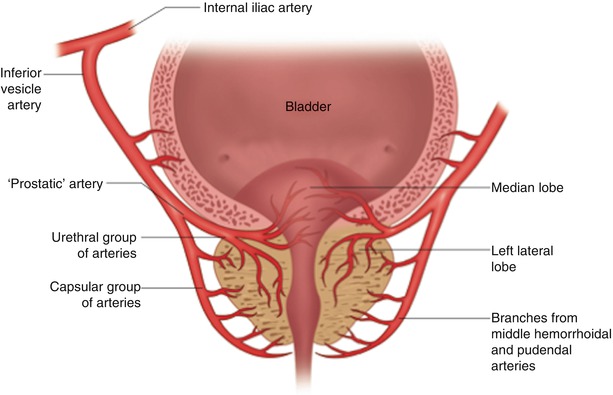
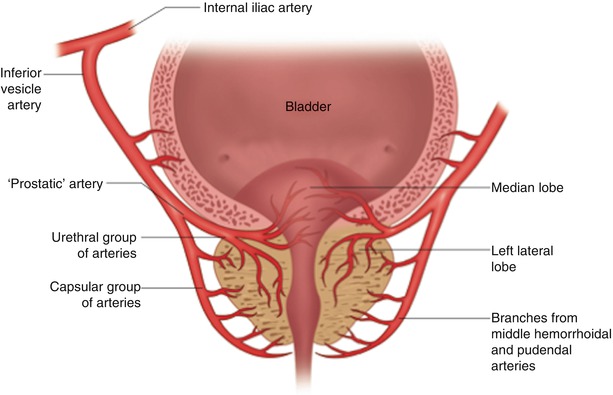
Fig. 6.3
Arterial supply to the prostate, bladder neck, and prostatic urethra
Prostate Zonal Anatomy
Clinically, and from an ultrasound prospective, the prostate is best identified as being divided into four zones (Fig. 6.4). Three of which are glandular (central, transition, and peripheral zones) and one is nonglandular (anterior fibromuscular stroma).
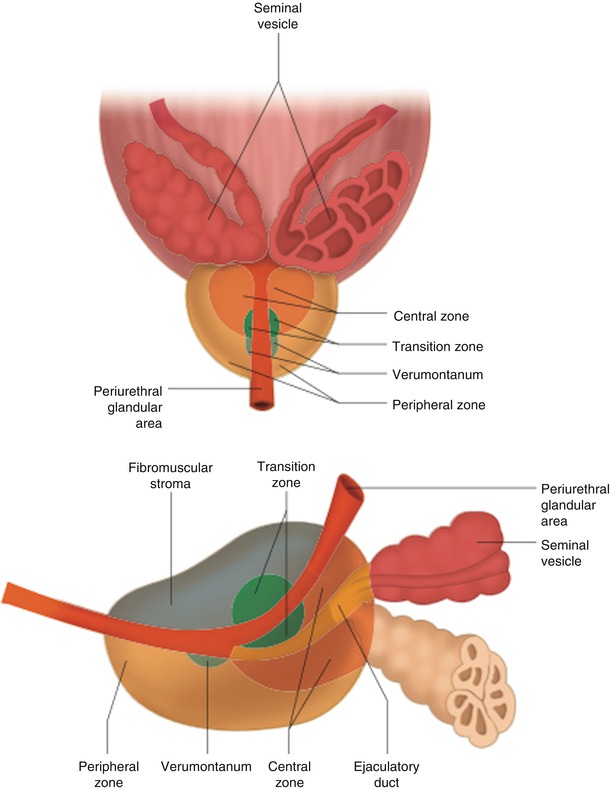
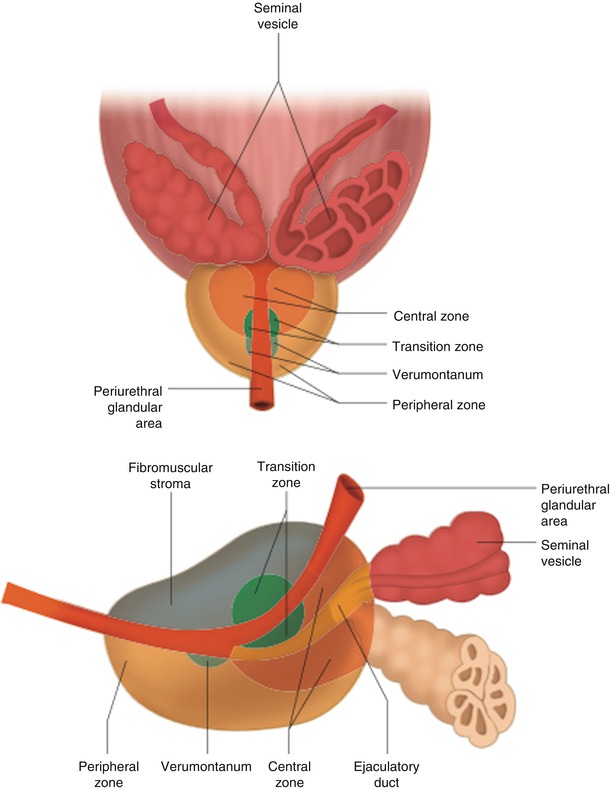
Fig. 6.4
Schematic of the prostate zonal anatomy
The central zone regresses with age and is often difficult to identify on ultrasound. The periurethral transition zone increases in size with age and is a major contributor to benign prostatic hypertrophy. The surgical “capsule” is the line between the peripheral and central/transition zones. The nonglandular zone, the anterior fibromuscular stroma, is located entirely anterior to the urethra.
Understanding prostatic zonal anatomy is important for understanding disease distribution and biopsy considerations. Furthermore, it is invaluable for understanding the ultrasound appearance of the prostate.
Prostate Orientation
The standard orientation for transrectal ultrasound (TRUS) of the prostate in the sagittal longitudinal image places the anterior of the prostate at the top of the screen, posterior of the prostate at the bottom (Fig. 6.5). The base of the prostate is at the bladder neck (which lies to the left side of the screen), while the apex is where the prostatic urethra meets the bulbar urethra (falling more to the right side of the screen). It is oriented as if the observer were positioned to the right of the patient, looking through them sagittally, in cross section. The transverse ultrasound standard orientation is similar to the CT scan appearance with the anterior of the prostate at the top of the ultrasound display and the posterior at the bottom, while the right prostate is on the left side of the screen and left prostate on the right when looking at the ultrasound display. It is oriented as if the observer were positioned at the patient’s feet looking up through them in cross section.
Fig. 6.5
Prostate orientation mimicking typical sagittal ultrasound view with the bladder to the left and the apex of the prostate to the right
Clinical Interpretation
Patient Concerns
Our patients often present for ultrasound examinations, prostate ultrasound in particular, with much trepidation about the exam, especially when a biopsy is to be done, as well as a heightened anxiety regarding what our findings might be. It is essential that we understand our patients’ concerns and make every effort to address them. Our patients appreciate the preprinted information about the ultrasound examination we provide. The brochure might include a discussion of the procedure, the preparation prior to the exam, what they might feel during the exam, as well as post-procedural instructions.
The examination is conducted in a warm room where the patient’s privacy is maintained. Traffic in and out of the room is kept to a minimum during the procedure. All equipment is readied prior to the patient entering the room to ensure the procedure proceeds as rapidly as possible and to minimize patient anxiety.
Equipment Maintenance and Preparation
Transrectal ultrasound is a procedure that mandates disinfection of all equipment between patients. Biopsies should only be done with disposable single-use needles. The physician should document (in a procedure manual) policies for prevention of infectious disease, cleaning of ultrasound transducers, and a policy for equipment maintenance and calibration. Manufacturer guidelines should always be followed. Patient complications should be documented and logged.
Clusters of infectious complications or bleeding should be investigated for protocol violations or equipment failures.
Normal Imaging
The use of the standard terminology is important to describe ultrasound findings:
1.
Hypoechoic is darker and more black.
2.
Hyperechoic is brighter and more white.
3.
Isoechoic is similar to the reference.
4.
Anechoic is without echoes.
5.
Homogeneous is of uniform echogenicity.
6.
Heterogeneous is of mixed echogenicity.
High water content makes tissue appear hypoechoic, while high fat content makes tissue appear hyperechoic. Unlike renal and abdominal ultrasounds where the liver is usually used as the benchmark for comparisons of echogenicity, the prostatic ultrasound does not include the liver, and thus the left and right sides of the gland should always be compared to each other (Fig. 6.6).
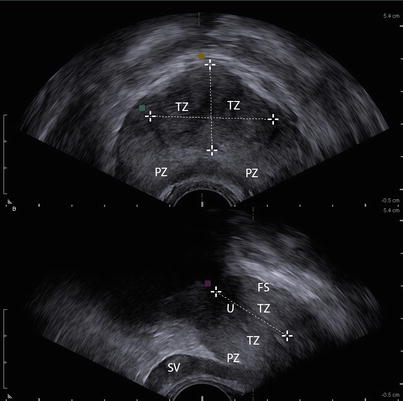
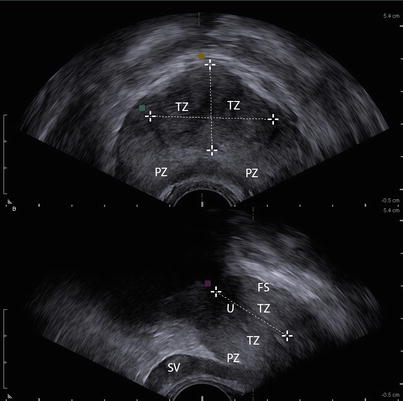
Fig. 6.6
The adult prostate. The top panel represents a transverse view and the bottom a longitudinal view. The transition zones (TZ), peripheral zones (PZ), anterior fibromuscular stroma (FS), seminal vesicle, and urethra (U) are indicated. The calipers are placed on the dimensions of the transition zone. Notice the symmetric echogenicity of the left and right sides in the top panel
The Adult Prostate
The young male prostate is homogenous with different zones often difficult to discern from each other. The “sonographic capsule” can be identified due to the impedance difference between the prostate and surrounding fat. The prominence of the urethra (u) is related to the surrounding low reflectivity of urethral muscles (Figs. 6.6 and 6.7).
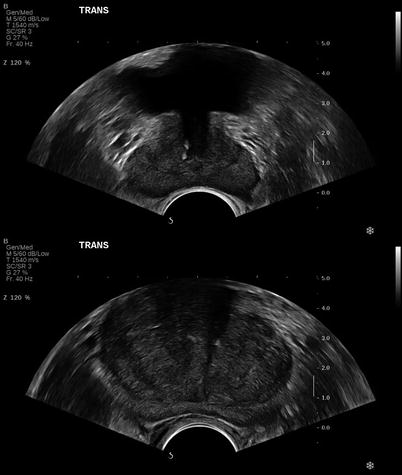
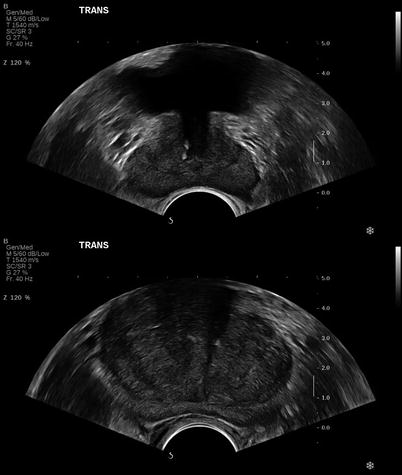
Fig. 6.7
The prostate in a 35-year-old male (top panel) and 65-year-old male (bottom panel). Note the prominence of the transition zone in the older male
In the young male, the peripheral zone (pz) is often hyperechoic compared to the central zone (cz) and transition zone (tz). The cz and tz are difficult to differentiate from each other, and the fibromuscular stroma (fs) is positioned anterior to the urethra.
In the older male the glandular and stromal elements enlarge, increasing the size of the tz and occasionally the pz. The tz is generally distinguishable from other zones. The cz is difficult to visualize (Fig. 6.7).
The base of the prostate is located at the superior aspect of the prostate contiguous with the bladder neck. The apex of the prostate is located at the inferior aspect of the prostate continuous with the striated muscles of the urethral sphincter (Fig. 6.5).
Scanning Protocol
A systematic scan will ensure that a comprehensive examination is performed and appropriately documented. A high-frequency (7.5–10 Mhz) transducer is usually used. This can be a biplanar or a single-plane transducer.
The patient is usually examined in the (left) lateral decubitus position with his legs flexed in the knee-to-chest position. It is essential to perform a digital rectal exam prior to inserting the ultrasound probe. Any pain, tenderness, rectal stricture, mass, lesion, and/or bleeding that is encountered when performing the rectal exam or when inserting the probe might preclude the TRUS.
The following represents one author’s protocol for scanning the prostate. It should be viewed as a guide and modified as the physician deems appropriate.
Protocol
After probe insertion, perform a “survey” scan of the prostate from base to apex including the seminal vesicles and rectal wall. This provides the sonographer with an overview of the prostate and surrounding structures and allows for the development of a “road map” for more detailed evaluation.
The seminal vesicles are then examined in the transverse plane for comparative evaluation of echogenicity and measurements of seminal vesicle height and ampulla (vas deferens) diameter. Next the mid-prostate, transverse image of the prostate is examined and the AP and width measurements are taken. If using a biplane probe, the length measurement can also be obtained from the midsagittal longitudinal image. If not using a biplane probe, then obtain a midsagittal longitudinal image for the length measurement. Prostate volume, predicted prostate-specific antigen (PPSA), and prostate-specific antigen density (PSAD) can then be calculated usually by formulas already programmed in the ultrasound machine.
Continue the exam in the transverse plane, obtaining appropriate image documentation of both base and apex views. The sonographer should then rotate the probe (or switch views if using a biplane probe) into a longitudinal plane to slowly scan the prostate from the levator ani on the left to the levator ani on the right. Depending on the field of view, this may need to be done at several positions along the axial length of the prostate. Oftentimes there may be a need to angle the probe up to examine the right side of the gland and down to examine the left. Images of the right lateral longitudinal, left lateral longitudinal, and midsagittal planes should be captured for documentation.
As in many urologic applications of sonography, color Doppler can add valuable information. Inflammatory disease processes result in increased vascularity that is well demonstrated with transrectal ultrasound. In addition, the sensitivity for the detection of neoplastic processes can be increased with the use of color Doppler [1]. Therefore, the sonographer should document the vascularity of the gland and any abnormal vascular patterns. Make sure to label and document each view.
The bladder should also be evaluated with measurements of the wall thickness, size, and location of any diverticula, calculi, or other abnormalities. Again, color Doppler adds another dimension. Ureteral jets can be evaluated with color or power Doppler confirming patency of the ureteral orifices. Bladder volume and post-void residual (PVR), if appropriate, should also be measured and documented.
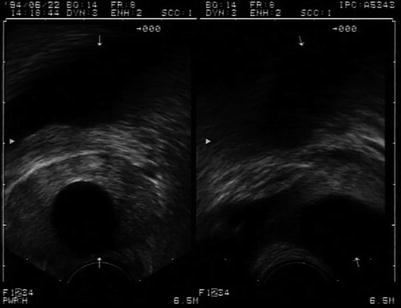
The rectal wall thickness must be evaluated and documented, as well as any other notable findings. The appearance of rectal abnormalities (Fig. 6.8) should be documented and should prompt referral to the appropriate medical specialist.
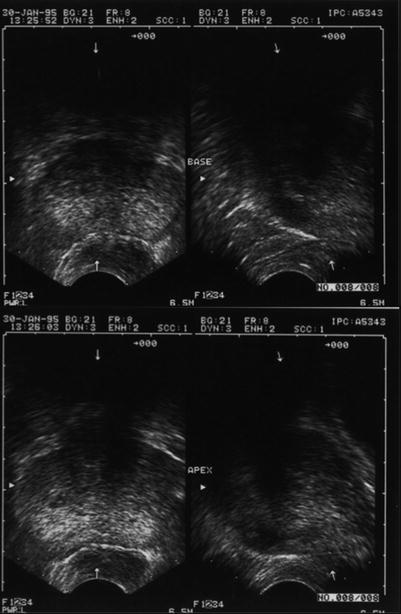
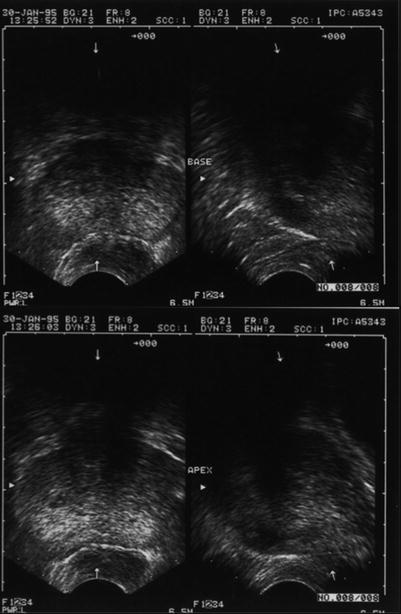
Fig. 6.8
A 62-year-old male with BPH found to have rectal mass. The mass is demonstrated as a thickening of the rectal wall on TRUS. The lower arrows on each panel point to the mass
The following are suggested images. They should be saved in a permanent medium, appropriately labeled, and attached to the written report:
1.
Transverse view of the prostate at the base
2.
Transverse view of the prostate at mid-gland with the mid-transverse anterior-posterior and width measurements indicated on the image
3.
Transverse view of the prostate at the apex
4.
Transverse view of the seminal vesicles
5.
Transverse view of the bladder with the mid-transverse anterior-posterior and width measurements indicated on the image
6.
Longitudinal (sagittal) view at midplane with the midsagittal longitudinal measurement indicated on the image
7.
Longitudinal (sagittal) view of right side 30° to 45° from midline
8.
Longitudinal (sagittal) view of left side 30° to 45° from midline
9.
Longitudinal view of the seminal vesicles
10.
Longitudinal view of the bladder with the midsagittal longitudinal measurement indicated on the image
Proper documentation of the ultrasound evaluation is an essential part of the examination. The goal is to provide a report that depicts what was observed and documents the features supporting the observations.
The report should include:
1.
Patient identification.
2.
Date of examination.
3.
Measurement parameters and anatomical findings of the examination.
4.
The indication for performing the examination is clear and provided on the report. The report is signed by the physician who performed the ultrasound examination.
Images should include the following:
1.
Patient identification.
2.
Date and time of each image.
3.
Clear image with clearly labeled orientation and measurements.
4.
Labeling of anatomy and any abnormalities.
5.
Images should be attached to the report.
Disinfection of Probes
An important aspect of patient safety is the disinfection of the ultrasound probes. Low-level disinfection is for probes that come into contact with intact skin such as those used for renal and bladder ultrasound. Intermediate-level disinfection is used for some critical and some non-critical indications and includes transducers used for ultrasound of the scrotum. High-level disinfection is for semi-critical items that come in contact with mucous membrane or intact skin. This would include transvaginal and transrectal ultrasound when no biopsy is performed. Critical-level disinfection is used on materials that will enter tissues or when blood will flow through them. This would include intraoperative transducers as well as endorectal probes with biopsy guides and their attachments. Manufacturer’s recommendations must be followed.
Indications for Prostate Ultrasound
Indications for prostate ultrasound are listed in Tables 6.1 and 6.2. It should be emphasized that these indications do not include routine screening.
Table 6.1
Indications for prostate ultrasound
1. Measurement of prostate volume for determination of PSA density |
2. Abnormal digital rectal exam |
3. Prostatic assessment with sonographic controlled biopsy |
4. Cysts |
5. Evaluation for and aspiration of prostate abscess |
6. Assessment for suspected congenital abnormality |
7. Lower urinary tract symptoms |
8. Pelvic pain |
9. Prostatitis/prostadynia |
10. Hematospermia |
11. Infertility |
(a) Azoospermia |
(b) Low-volume or poorly motile specimen |
(c) Cysts |
(d) Hypoplastic or dilated seminal vesicle |
(e) Impaired motility |
(f) Antisperm antibodies |
Table 6.2
Indications for transrectal ultrasound-guided biopsy
To investigate an abnormal PSA or DRE |
To follow up a biopsy with inconclusive or premalignant findings (e.g., ASAP, HGPIN) |
To diagnose local recurrence after primary treatment for prostate cancer |
Measurement of Prostate-Specific Antigen Density (PSAD)
Benign prostatic hypertrophy (BPH) occurs in most men and results in a rise in PSA not related to prostate cancer. PSAD is the blood PSA (ng/ml) level divided by the volume of the prostate, as determined by TRUS. With most ultrasound software packages, the sonographer inputs the PSA and then measures the prostate with the mathematics performed electronically. With benign disease (BPH), the PSAD should not be more than 0.15 ng/ml/cm3 of prostatic tissue. PSA levels exceeding 0.15 ng/ml/cc indicate the need for further evaluation.
Congenital Abnormality
Prostate Cysts
Most prostate cysts are benign. The location often defines the etiology (Fig. 6.9). Müllerian cysts do not communicate with the urethra, while utricle cysts are the fused caudal ends of the Müllerian ducts or urogenital sinus remnant and can communicate with the urethra. As with prostatic cysts, seminal vesicle cysts are suspected when ejaculate volume is low. They can also be seen with adult polycystic kidney disease.
Get Clinical Tree app for offline access
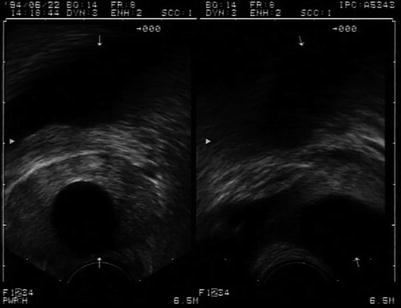
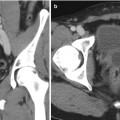
Fig. 6.9
Prostate cyst demonstrated in the midline prostate with transverse (left panel) and longitudinal (right panel




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree