Trauma
Over the past 30 years, trauma surgeons in Europe and Japan have demonstrated the proficient use of ultrasonography in evaluating blunt trauma patients.1–9 During the 1990s, emergency physicians and trauma surgeons in North America have prospectively evaluated the applications of ultrasonography in trauma and have presented results comparable with those of other investigators worldwide.10–18
The focused assessment with sonography for trauma (FAST) examination is a bedside screening tool to aid clinicians in identifying free intrathoracic or intraperitoneal fluid. The underlying premise behind the use of the FAST examination is that clinically significant injuries will be associated with the presence of free fluid accumulation in dependent areas. The FAST examination was originally developed as a limited ultrasound examination, focusing primarily on the detection of free fluid, and was not designed to universally identify all sonographically detectable pathology. Over the last decade many groups have proposed additions or modifications to the standard FAST examination. However, the essence of the FAST examination is identifying findings that can be interpreted by clinicians within a clinical context. As this approach has grown to the extent that some propose integrating ultrasound completely within the advanced trauma life support (ATLS) sequence,19 the challenge for the future is to capitalize on the information point-of-care ultrasound provides, while not delaying critical interventions.20
 CLINICAL CONSIDERATIONS
CLINICAL CONSIDERATIONS
The rapid and accurate diagnosis of injuries sustained by trauma patients can be difficult, especially when they are associated with other distracting injuries or altered mental status from head injury or drug or alcohol use. In the United States, the three generally accepted diagnostic techniques for evaluating abdominal trauma patients are diagnostic peritoneal lavage (DPL), CT of the abdomen, and ultrasonography. Each of these diagnostic modalities has its own advantages and disadvantages.
DPL remains an excellent screening test for evaluating abdominal trauma. Table 5-1 reviews the advantages and disadvantages of DPL.
 TABLE 5-1. ADVANTAGES AND DISADVANTAGES OF DIAGNOSTIC PERITONEAL LAVAGE
TABLE 5-1. ADVANTAGES AND DISADVANTAGES OF DIAGNOSTIC PERITONEAL LAVAGE
Advantages
Sensitivity for detecting hemoperitoneum
Availability of equipment
Relative speed with which it can be performed
Low complication rate with an experienced operator
Ability to detect early evidence of bowel perforation
Disadvantages
Potential for iatrogenic injury
Misapplication for evaluation of retroperitoneal injuries
Lack of specificity
CT of the abdomen has a greater specificity than DPL, thus making it the initial diagnostic test of choice at all trauma centers. IV contrast material should be given to provide optimal resolution. Table 5-2 reviews the advantages and disadvantages of CT.
 TABLE 5-2. ADVANTAGES AND DISADVANTAGES OF CT
TABLE 5-2. ADVANTAGES AND DISADVANTAGES OF CT
Advantages
Ability to precisely locate intra-abdominal lesions preoperatively
Ability to evaluate the retroperitoneum
Ability to identify injuries that may be managed nonoperatively
Noninvasive
Disadvantages
Expense of the study
Time required to perform the study
Need to transport the trauma patient to the radiology suite
Need for contrast materials
Ionizing radiation exposure to patient
Ultrasonography offers several advantages over DPL and abdominal CT. Numerous studies have demonstrated that the FAST examination, like DPL, is an accurate screening tool for abdominal trauma. – 1– – 18 Advantages of the FAST examination are that it is accurate, rapid, noninvasive, repeatable, and portable, and involves no nephrotoxic contrast material or radiation exposure to the patient. There is limited risk for patients who are pregnant, coagulopathic, or have had previous abdominal surgery. The average time to perform a complete FAST examination of the thoracic and abdominal cavities is 4.0 minutes or less.12 However, investigators have demonstrated that a massive hemoperitoneum may be quickly detected with a single view of Morison’s pouch in 82–90% of hypotensive patients, – 18,21 and this required an average of only 19 seconds in one study. – 18 One major advantage of the FAST examination compared with DPL or abdominal CT is the ability to also evaluate for free pericardial or pleural fluid and for pneumothorax. The main disadvantage of the FAST examination compared with CT has been the inability to determine the exact etiology of the free intraperitoneal fluid. This limitation has the potential for significant change as a growing number of studies have reported the utility of contrast-enhanced ultrasonography for the identification and treatment of solid organ injuries.22–24 Other potential disadvantages of the FAST examination are the operator-dependent nature of the examination, the difficulty in interpreting the images in patients who are obese or have subcutaneous air or excessive bowel gas, and the inability to distinguish intraperitoneal hemorrhage from ascites. The FAST examination also cannot evaluate the retroperitoneum as well as CT, making these complementary rather than competing technologies when time permits and the potential benefits of CT outweigh the risks.
In light of the evolving nonoperative approach to certain types of solid-organ injuries, a positive DPL by itself is becoming less of an indication for immediate exploratory laparotomy than the amount of hemorrhage and the clinical condition of the patient. Since the FAST examination can reliably detect small amounts of free intraperitoneal fluid and can be used to estimate the rate of hemorrhage through serial examinations, ultrasonography has essentially replaced DPL for blunt abdominal trauma in the majority of North American trauma centers.
 CLINICAL INDICATIONS
CLINICAL INDICATIONS
Generally accepted clinical indications for performing the FAST examination include
 acute blunt or penetrating torso trauma,
acute blunt or penetrating torso trauma,
 trauma in pregnancy,
trauma in pregnancy,
 pediatric trauma,
pediatric trauma,
 subacute torso trauma, and
subacute torso trauma, and
 undifferentiated hypotension.
undifferentiated hypotension.
 ACUTE BLUNT OR PENETRATING TORSO TRAUMA
ACUTE BLUNT OR PENETRATING TORSO TRAUMA
At Level 1 trauma centers, the primary utilization of the FAST examination has been for the rapid detection of free intraperitoneal fluid in patients who have sustained significant blunt torso trauma. More recently, trauma programs have begun to incorporate the FAST examination into the primary patient assessment for detecting the presence, amount, and location of intracavitary hemorrhage in general. It is likely that these indications will greatly expand as an ever-increasing numbers of clinicians adopt resuscitative ultrasound into their daily practice. This will increase the responsibility for these clinicians to ensure the use of ultrasound as an adjunct will expedite, and not delay, therapy.
With blunt trauma, the FAST examination is particularly useful for patients who (1) are too hemodynamically unstable to leave the ED for CT scanning; (2) have a physical examination that is unreliable secondary to drug intoxication, distracting injury, or central nervous system injury; and (3) have unexplained hypotension and an equivocal physical examination.
With penetrating trauma patients, the FAST examination should be performed when it is not certain that immediate surgery is indicated. In patients with multiple wounds, the FAST examination can be used to quantify and locate the source of internal hemorrhage. When the trajectory of a penetrating wound is uncertain, the FAST examination may quickly identify the course by the presence of free fluid within the compartments involved. This is particularly helpful when the entry location is the precordium, lower chest, or epigastrium. Inappropriate surgical sequencing has been reported to occur in 44% of patients with wounds in multiple body cavities.25 In a review of patients with injuries to both the thoracic and abdominal cavities, the investigators regretted their limited use of early FAST examinations in directing surgical sequencing and strongly recommended its increased use in the initial patient evaluation. – 25 The FAST examination can therefore be used to prioritize such lifesaving interventions as pericardiocentesis, pericardiotomy, thoracostomy, thoracotomy, laparotomy, or sternotomy. The FAST examination is useful in evaluating patients who have sustained stab wounds to the abdomen where local wound exploration indicates that the superficial muscle fascia has been violated. Also, the FAST examination may be useful in confirming a negative physical examination when tangential or lower chest wounds are involved.
In non-Level 1 trauma centers, emergency physicians and surgeons may lack the immediate availability of CT scans and formal two-dimensional (2D) echocardiograms. The use of bedside ultrasonography by physicians trained to perform the FAST examination in these settings will significantly improve patient evaluation, initial treatment, consultation, and the timely transportation of patients to trauma centers when indicated. When the FAST examination demonstrates intracavitary fluid in these settings, surgeons and operating room personnel can be consulted immediately and/or transportation to a Level 1 trauma center can be initiated. When the diagnostic imaging personnel and surgeons are out of the hospital, and the severity of the patient’s injuries is not clinically evident, a positive FAST examination could save up to an hour or more of time to definitive surgical treatment.26–28
Although the FAST examination is used most commonly to detect free intraperitoneal fluid, it may also aid in the rapid identification of pneumothorax and free pericardial or pleural fluid, and the evaluation of the fetus in the pregnant trauma patient. In addition, the FAST examination has been evaluated in the management of pediatric trauma patients and can be utilized in patients who present with subacute trauma but with a significant mechanism of injury or concerning physical examination.
DETECTION OF FREE INTRAPERITONEAL FLUID
By the latter half of the 1990s, for patients who had sustained blunt or penetrating abdominal trauma, the FAST examination’s utility for detecting free intraperitoneal fluid had been universally recognized. While CT remained the gold standard for detecting specific intraabdominal pathology, the FAST examination had gained acceptance as a rapid screening tool for identifying free intraperitoneal fluid.
During the 1980s, surgeons in Germany developed bedside utilization of ultrasonography for evaluation of trauma patients. Although excellent results were reported in early studies, with the sensitivity ranging from 84% to 100% and the specificity from 88% to 100%, these findings went largely unnoticed in the United States as the articles were not initially translated into English.2–7
In the 1990s, a number of prospective studies (with study sizes greater than 100 patients) had been reported on this issue in the English literature. – 1,8– – 18 The majority of these studies focused on the FAST examination for the evaluation of free intraperitoneal fluid in blunt abdominal trauma patients only. These studies reported the sensitivity and the specificity to range from 69% to 90% and 95% to 100%, respectively.
Tiling and colleagues were the first investigators to suggest that the FAST examination could provide comprehensive evaluation for significant areas of hemorrhage, including pericardial, pleural, intraperitoneal, and retroperitoneal. Their prospective study of 808 blunt trauma patients found a sensitivity of 89% and a specificity of 99% for free intraperitoneal fluid. Their clinical algorithm incorporates the FAST examination during the initial patient evaluation. – 1
One of the first North American trauma ultrasound studies demonstrated the FAST examination to have an overall sensitivity of 79% and specificity of 95.6%. They concluded that appropriately trained surgeons could rapidly and accurately perform and interpret FAST examinations and that ultrasound was a rapid, sensitive, and specific diagnostic modality for detecting intraperitoneal fluid and pericardial effusion. – 10 Ultrasound has been used as the primary adjuvant modality to detect hemoperitoneum and pericardial effusion in injured patients (Figure 5-1). After finding that the FAST examination had an 81.5% sensitivity and 99.7% specificity, the investigators stated that ultrasound should be the primary adjuvant instrument for the evaluation of injured patients because it was rapid, accurate, and potentially cost-effective.11
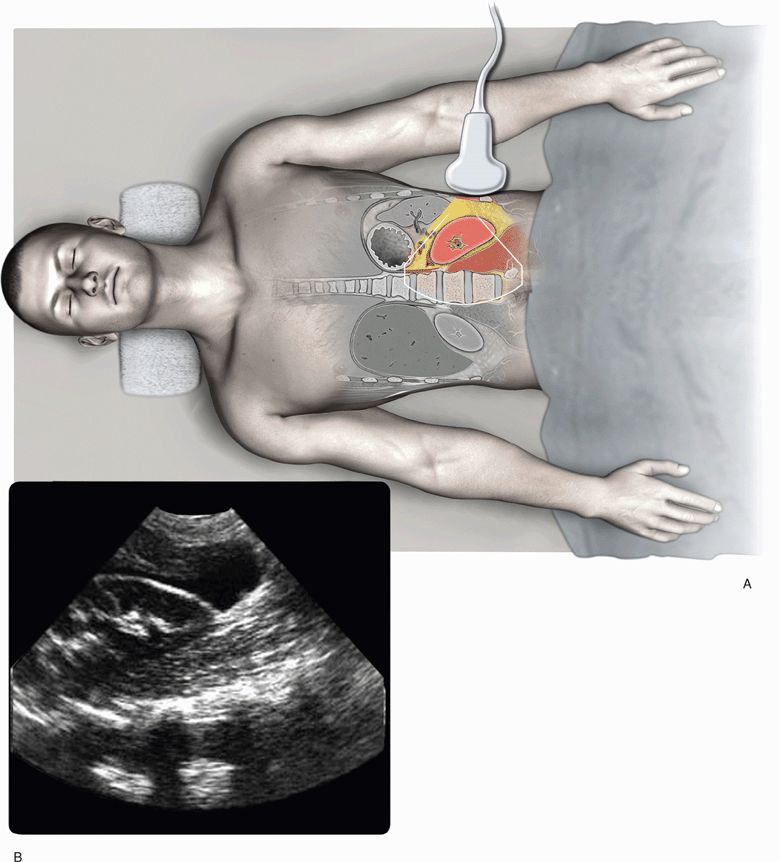
Figure 5-1. Examination of the abdomen to assess for free intraperitoneal fluid. Transducer position for the coronal view of the left upper quadrant (A) and corresponding ultrasound image (B) with free fluid in the paracolic gutter adjacent to the lower pole of the kidney.
In 1995, Ma and Mateer prospectively demonstrated that the FAST examination could serve as a sensitive, specific, and accurate diagnostic tool in the detection of free intraperitoneal and thoracic fluid in patients who had sustained major blunt or penetrating trauma. Overall, the FAST examination had a sensitivity of 90%, specificity of 99%, and accuracy of 99%. In evaluating the subgroup of blunt trauma patients, which consisted of 165 of the 245 patients, the FAST examination was 90% sensitive, 99% specific, and 99% accurate. In evaluating the subgroup of penetrating trauma victims, which consisted of 80 of the 245 patients, the FAST examination was 91% sensitive, 100% specific, and 99% accurate.12 Since emergency physicians performed all the FAST examinations, it became the first prospective study to support that appropriately trained emergency physicians could accurately perform and interpret FAST examinations. The results reiterated that a FAST examination of the entire torso could successfully provide early and valuable information for the presence of free fluid in both the peritoneal and thoracic cavities. In addition, the FAST examination was found to be equally sensitive, specific, and accurate for both blunt and penetrating torso trauma. Penetrating trauma patients could benefit from the rapid and accurate information yielded by ultrasonography. – 18 The identification and localization of significant hemorrhage in penetrating trauma patients would allow physicians “to prioritize resources for resuscitation and evaluation.” – 10 Most studies have utilized a multiple-view FAST examination for evaluation of trauma patients. Some investigators have employed a single-view technique, examining only Morison’s pouch for free intraperitoneal fluid.29–31 In one study, all patients were placed in the Trendelenburg position and the perihepatic (Morison’s pouch) was the single area examined. The results of this technique were reported to be 81.8% sensitive, 93.9% specific, and 90.9% accurate.29
The single-view (perihepatic) imaging technique was compared with the multiple-view technique of the FAST examination for the identification of free intraperitoneal fluid in patients who had sustained major blunt or penetrating torso trauma. For detecting free intraperitoneal fluid, when comparing the multiple-view FAST examination of the abdomen to the gold standard, the multiple-view FAST examination technique had a sensitivity of 87%, a specificity of 99%, and an accuracy of 98%. When comparing the perihepatic single view of the abdomen to the gold standard, the single-view FAST examination technique had a sensitivity of 51%, a specificity of 100%, and an accuracy of 93%.13 Based on this and other studies, the more sensitive and accurate FAST examination method for detecting free intraperitoneal fluid was determined to be the multiple-view technique.13
DETECTION OF SOLID ORGAN INJURY
The use of contrast-enhanced ultrasonography may help clinicians identify specific organ injuries on the FAST examination.32–35 Contrast-enhanced ultrasonography is the application of ultrasound contrast agents to complement or augment traditional sonography. Newer second-generation ultrasound contrast agents contain perflutren microbubbles that when administered IV can pass through the pulmonary circuit into the systemic vasculature. The microbubbles vibrate strongly at the high frequencies used in diagnostic ultrasonography, which makes them several thousand times more reflective than normal body tissues. This characteristic allows microbubbles to enhance both gray scale images and flow-mediated Doppler signals. Although an initial FDA black box warning has slowed widespread utilization in the United States, microbubble contrast agents have subsequently been found to be as safe as conventional agents used in radiography and magnetic resonance imaging.22–24
Contrast-enhanced ultrasonography has been shown to be a promising tool for detecting solid organ (liver and spleen) injuries after blunt abdominal trauma. When an ultrasound contrast agent was administered immediately before performing the traditional FAST examination, the examination has correlated appreciably better than unenhanced sonography for detecting hepatic and splenic injuries and estimating the extent of their injuries.32–34 One study reported their 5-year experience with 133 blunt abdominal trauma patients. When compared with CT, contrast-enhanced ultrasonography had a sensitivity and specificity of 96.4% and 98%, respectively. The authors concluded that “contrast enhanced ultrasonography is an accurate technique for evaluating traumatic lesions of solid abdominal organs …. is able to detect active bleeding and vascular lesions, and avoids exposure to ionizing radiation.”23
Another study analyzed 392 patients with liver and/or spleen injuries and demonstrated no significant difference in detection rate for active bleeding between contrast-enhanced ultrasonography and contrast CT.24 As clinicians continue to explore the uses for contrast-enhanced ultrasonography in trauma, there is great potential for reducing the costs and radiation exposure associated with CT while identifying patients requiring immediate operative intervention compared with those who may benefit from nonoperative management of solid organ injuries.
CLINICAL ALGORITHMS
Clinical pathways and protocols have been derived from the use of the FAST examination and incorporated with other diagnostic methods commonly used for trauma evaluation in North America (Figure 5-2). Inclusion of the FAST examination into a protocol for the management of patients sustaining torso trauma has been found to decrease time to operative intervention and improve resource utilization by reducing CT usage, hospital days, and total patient charges.36 Another ultrasound-based key clinical pathway has been shown to reduce the number of DPL procedures and CT scans required to evaluate blunt abdominal trauma without increased risk to the patient (Figure 5-3). Cost savings were estimated to be $450,000 per year using this key clinical pathway.37 The issue of cost savings of the FAST examination has also been addressed in another study. For blunt trauma patients, the FAST examination was found to be more efficient and cost-effective than CT scanning or DPL. There was a significantly shorter time to disposition at approximately one-third the cost in the ultrasonography group.38
Figure 5-2. Suggested algorithm for the use of ultrasonography in the evaluation of the patient with blunt abdominal trauma. (From Rozycki GS, Shackford SR: Ultrasound: what every trauma surgeon should know. J Trauma 40:2, 1996, with permission.)
Figure 5-3. Key clinical pathway for the evaluation of blunt abdominal trauma. (From Branney SW, Moore EE, Cantrill S, et al.: Ultrasound-based key clinical pathway reduces the use of hospital resources for the evaluation of blunt abdominal trauma. J Trauma 42:1086–1090, 1997, with permission.)
An ultrasound-based scoring system has been developed to quantify the amount of intraperitoneal blood in blunt abdominal trauma patients and to assess the need for therapeutic exploratory laparotomy. Scores ranged from 0 to 8. The system assigned two points for significant fluid collections ≥2 cm and one point for fluid collections ≤2 cm. A score of 3 correlated with 1000 mL of fluid. In the study, of those patients who had a score of 3 or more, 24 of 25 patients (96%) required therapeutic laparotomy. Of those who had a score of less than 3, therapeutic laparotomy was required in only 9 of 24 patients (38%). The FAST examination was found to be a useful adjunct in helping to make clinical decisions during the resuscitation period.39 In another study evaluating the role of the FAST examination in determining the need for therapeutic laparotomy, none of the patients with negative FAST examination results died or sustained identifiable mortality as a consequence of their negative scans.40
DETECTION OF PERICARDIAL FLUID
In the hypotensive patient who has sustained penetrating trauma to the torso, the echocardiographic portion of the FAST examination may prove to be the most beneficial aspect. Echocardiography remains the gold standard diagnostic procedure for detecting pericardial effusions. The classic physical examination findings of acute cardiac tamponade—distended neck veins, hypotension, and muffled heart tones—are present in less than 40% of patients with surgically proven cardiac tamponade.41 Timely ED procedures and expeditious transportation of the patient to the operating room may be accomplished by ultrasound diagnosis of hemopericardium.
In 1992, Plummer and coinvestigators evaluated the effect of bedside echocardiography performed by emergency physicians on the outcome of 49 patients with penetrating cardiac injuries over a 10-year period. Compared with a retrospective control group, the use of bedside echocardiography significantly reduced the time of diagnosis and disposition to the operating room from 42.4 ± 21.7 minutes to 15.5 ± 11.4 minutes while the actual survival improved from 57.1% to 100%.42
The accuracy of point-of-care ultrasound has been evaluated after it was introduced into five Level I trauma centers for the diagnosis of acute hemopericardium. Surgeons or cardiologists (four centers) and technicians (one center) performed pericardial ultrasound examinations on patients with penetrating truncal wounds. By protocol, patients with positive examinations underwent immediate operation. In 261 patients, pericardial ultrasound examinations were found to have a sensitivity of 100%, specificity of 96.9%, and accuracy of 97.3%. The mean time from ultrasound to operation was 12.1 ± 5 minutes. This further demonstrated that ultrasound should be the initial modality for the evaluation of patients with penetrating precordial wounds because it is accurate and rapid.43
Over the years, numerous studies have examined the role of echocardiography in blunt cardiac trauma. The utility and role of ultrasound, particularly with the diagnosis of cardiac contusion, remain unclear (see Chapter 6, “Cardiac,” for a comprehensive review of this topic).
DETECTION OF PLEURAL FLUID
Since patients who have sustained major trauma routinely present to the ED immobilized on a long spine board, clinicians may have difficulty identifying bilateral hemothoraces or a small unilateral hemothorax on the initial supine chest radiograph. The FAST examination can detect hemothorax before the completion of a chest radiograph or can be used as additional information when the chest radiograph is equivocal. Thus, tube thoracostomy for trauma patients may be expedited with the use of ultrasonography.
Ma and Mateer demonstrated that the FAST examination could serve as a sensitive, specific, and accurate diagnostic tool in detecting hemothorax in major trauma patients. When comparing the FAST examination and the chest radiograph with the criterion of standard definitions, both diagnostic tests had an equal sensitivity (96.2%), specificity (100%), and accuracy (99.6%) for detecting pleural fluid. They concluded that ultrasonography was comparable to the chest radiograph for identifying hemothorax.44
Ultrasonography can detect smaller quantities of pleural fluid than the chest radiograph. It is estimated that an upright chest radiograph can accurately detect a minimum of 50–100 mL of pleural fluid45 and that a supine chest radiograph can detect a minimum of 175 mL of pleural fluid.46 By contrast, it is estimated that ultrasonography can detect a minimum of 20 mL of pleural fluid.9 Also, ultrasonography can help differentiate between pleural fluid and pleural thickening or pulmonary contusion when the supine chest radiograph is equivocal.
Although the FAST examination cannot completely replace the chest radiograph, it can complement chest radiograph findings by rapidly identifying hemothorax in the supine patient. Of the six anatomic areas scanned by the FAST examination, only two are required to identify the presence of free pleural fluid in the two pleural cavities. By utilizing the FAST examination to initially identify hemothorax, the standard chest radiograph of the trauma patient can be performed after tube thoracostomy, thereby sparing the patient an additional chest radiograph.
DETECTION OF PNEUMOTHORAX
Not only can the FAST examination detect a hemothorax, it can also identify a pneumothorax before the completion of a chest radiograph. This is especially relevant since the reported proportion of pneumothoraces that are occult compared with those actually seen on the chest radiograph ranges from 29% to 72%.47–52 The concept of using ultrasound to exclude the presence of a pneumothorax relies on the simple premise that if the two pleural surfaces are normally in apposition, then an intrapleural collection of air (pneumothorax) cannot be separating them. The focused goal is to identify the contiguity of the visceral and parietal pleura using simple sonographic signs to exclude the presence of a pneumothorax. This diagnostic test is considered to be an extended FAST (E-FAST) examination.51 With experience and always appreciating the clinical setting, a pneumothorax can be expeditiously excluded in the vast majority of cases.53
Detecting a pneumothorax with ultrasound may initially appear to be paradoxical since air has the highest acoustic impedance of normal body substances, with almost complete reflectance of sound waves at commonly used frequencies.54 Thus, only artifacts are normally seen deep to the pleural interface in the normal lung.55 Both hemothoraces and pneumothoraces, however, are superficial pleural-based diseases and, therefore, lend themselves to sonographic examination (Figure 5-4).
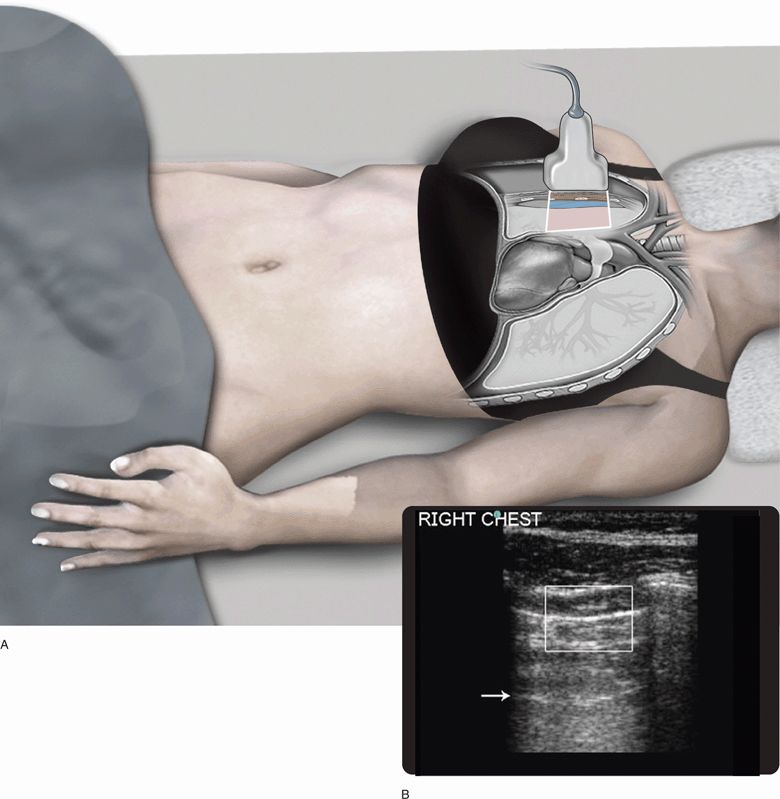
Figure 5-4. Examination of the pleural interface to assess for pneumothorax. Transducer position on the anterior chest with the patient in the supine position (A). Ultrasound image of the pleural interface (bright horizontal line in center of box) and normal A-line artifact (arrow) deep to the pleural interface (B).
Unless there are pleural adhesions from previous disease or injury (a condition that reduces the risk of pneumothorax), normal respiration is associated with a physiologic sliding of the two pleural surfaces upon one another. The most common normal sign on sonography is lung sliding, which in essence excludes the presence of a pneumothorax in the area that has been imaged.48,51,53 For this physiologic “lung sliding” along the visceral–parietal pleural interface to be seen, both surfaces must be accessible for imaging and must be either contiguous or separated by a layer of fluid.50,51,56 Conceptually, this sign represents the visual depiction of breathing. It does not comment upon ventilator adequacy or exclude serious pulmonary pathology other than ruling out a pneumothorax; it simply indicates that the patient has ventilatory efforts when it is seen. This movement is better visualized at the lung bases and less so at the apices.53 It is important to consider that free air within the thorax will usually seek the point of maximum elevation, so that a normal sliding sign seen in the lung bases cannot exclude a partial pneumothorax in a supine patient (the anterior and apical areas must be imaged as well). A notable exception for viewing a normal sliding sign is when subcutaneous emphysema superimposes itself between the skin and the parietal pleura, but this clinical situation is also associated with a specificity of 98% for underlying occult pneumothorax and is usually evident on physical examination.57
Examining the pleural interfaces with the color power Doppler mode can enhance the depiction of this sliding movement due to power Doppler’s ability to detect motion, a finding that has been designated the “Power Slide.”49 Power Doppler is superior to conventional color Doppler in determining the presence or absence of flow at the expense of direction and speed information and thus has the ability to identify low-velocity and low-volume flow (or motion).49,58,59 It also documents a real-time physiologic process in a single still image, allowing for simpler archiving and tele-transmission. In a similar way, the use of M-mode imaging documents either the presence of lung sliding (“seashore sign”) or its absence when a pneumothorax is present (“stratosphere sign”) since the pleural movement will normally generate a homogenous granular pattern in this mode.53,60 An intermediate sign that is best documented in M-mode is the “lung point” sign, which is visualized when the lung intermittently contacts the parietal pleura with inspiration, thus alternating between the seashore and stratospheric signs.
Other commonly seen artifacts are B-lines, which are also referred to as the comet-tail artifact. This is a reverberation artifact thought to arise from distended water-filled interlobular septae under the visceral pleura. Comet-tail artifacts are presumed to be the ultrasound equivalents of Kerley B-lines seen on a chest radiograph.53,61 Thus, this sign represents the visual equivalent of hearing lung crepitations. Being related to the visceral pleura, B-lines can be seen only when the visceral pleura is in apposition to the parietal pleura. When a pneumothorax is present, the intrapleural air will separate the two pleural surfaces, and B-lines will be absent. Instead, the only artifacts that will appear to be deep to this level are horizontal reverberation artifacts, which are often seen as a “mirror image” of the chest wall.
Lichtenstein and coworkers have described a standardized, but hierarchal thoracic examination whose scope depends on the clinical status and mobility of the patient. They designate the A-line as a brightly echogenic line between the rib shadows recurring at an interval that exactly replicates the interval between the skin and pleural line, and represents the horizontal reverberation artifact generated by the parietal pleura.53
If both lung sliding and B-lines are present, then the clinician can confidently exclude the presence of a pneumothorax. If lung sliding and B-lines are not visible, then the examiner should suspect the presence of a pneumothorax, a suspicion further heightened by the presence of the horizontal reverberation artifact (A-line).62,63 The absence of lung sliding alone had 100% sensitivity, but only 78% specificity for diagnosing an occult pneumothorax. When an A-line was seen with absent lung sliding, there was 95% sensitivity and 94% specificity for diagnosing an occult pneumothorax.60 The presence of a lung point had 100% specificity for an occult pneumothorax. This is a critical distinction. No sliding does not mean a pneumothorax is present, only that a pneumothorax might be present. The pleura will not “slide” normally when there is pleural symphysis from adhesions or there is apnea, either voluntary or induced, such as with paralysis. Thus, if lung sliding is not seen, then B-lines are sought next. If these are not seen, then a lung point should be sought by progressively scanning laterally on the supine chest or inferiorly on an upright chest. Clinical context is always important. The lung point implies intermittent contact of the underlying lung against the parietal pleura, meaning a so-called “partial pneumothorax.” If there is a very large pneumothorax, the lung will never contact the parietal pleura and no lung point will be detected. Thus, diagnosis requires interpretation within the clinical context, which is what empowers point-of-care sonography in the clinician’s hands.64
Kirkpatrick and coinvestigators prospectively evaluated a handheld ultrasound device in the real-time resuscitation of critically ill patients.51 This study focused on the most difficult-to-diagnose subset of pneumotho-races, as any patient with a clinically evident pneumothorax was treated without any imaging and those patients with clear-cut pneumothoraces on chest radiograph were excluded as well. In the remaining clinically stable patients, when comparing E-FAST directly with chest radiography, the E-FAST examination was more sensitive for the detection of occult pneumothoraces after trauma (49% versus 21%). Using CT corroboration, there were 22 false negative studies with E-FAST compared with 34 with chest radiography.51 Another study analyzed 176 patients by systematically examining four thoracic locations, ranging from the 2nd intercostal space in the midclavicular line to the 6th intercostal space at the posterior axillary line. The authors searched for lung sliding, supplemented by color power Doppler when lung sliding was not easily detected, and assessed the relative size of the pneumothorax by correlating the relative topography of lung sliding. Overall, the sensitivity and specificity of ultrasound were noted to be 98% and 99%, respectively, compared with 76% and 100%, respectively, for chest radiography in this setting.65
Reflecting on basic principles, the E-FAST technique has an inherent advantage over chest radiography due to the physiologic behavior of pneumothoraces in the supine patient. Because of the effect of gravity, the supine lung tends to hinge dorsally, with free air collecting anteromedially.66–69 Supine pneumothoraces are reported to be most commonly located at the anterior (84%), apical (57%), basal (41%), medial (27%), lateral (24%), and never posterior (0%) lung locations.70 The standard imaging anatomic sites for the E-FAST were chosen to correspond to the recommended auscultatory locations from the ATLS course.71
Despite the fact that pneumothoraces are often a dynamic process, clinical management is often based on the perceived size of a pneumothorax. Allowing for other factors such as the need for transport and positive pressure ventilation, many small pneumothoraces are managed expectantly, whereas larger ones are more aggressively treated. Thus, it is pertinent to ask whether ultrasound may be of help in determining the size of pneumothoraces. While it was once believed that sonography was of no use in determining the volume of a pneumothorax,55 it is now suggested that sonography may actually have utility in determining not only the presence but also the actual extent of a pneumothorax.68
The presence of a “lung point” sign is not only 100% specific for pneumothorax but also the location of this sign roughly correlates with the radiographic size of the pneumothorax.63 A “partial sliding” sign has been described to represent the same phenomenon whereby smaller or occult pneumothoraces might be detected.72 Also, a good correlation between the estimates of pneumothorax size and CT findings using the relative thoracic topography of lung sliding has been noted.64
 TRAUMA IN PREGNANCY
TRAUMA IN PREGNANCY
Trauma continues to be one of the leading causes of nonobstetrical mortality in pregnant patients.73 Moreover, it contributes to fetal death more frequently than maternal death.74–78 Ultrasonography may be a valuable adjunct for rapid diagnosis of traumatic injuries for both the mother and the fetus.79–81
The pregnant trauma patient presents unique diagnostic and management issues for the emergency physician and trauma surgeon. Maternal shock carries a high fetal mortality rate.77 Although there are two lives at stake, proper assessment and stabilization of the mother will provide the best opportunity for fetal stability. Therefore, rapid assessment of the pregnant trauma patient is essential for early identification of life-threatening injuries. The FAST examination clearly may play a role in the timely assessment of pregnant trauma patients.
In this setting, ultrasonography offers several advantages over abdominal CT scan and DPL. The FAST examination may aid in the timely identification of pregnant trauma patients who need exploratory laparotomy immediately, and may help avoid delays in management while other diagnostic tests are obtained. The FAST examination can be performed at the bedside and involves no contrast material or radiation exposure to the mother or the fetus. Sonography can rapidly assess the pregnant trauma patient for hemoperitoneum and intrathoracic hemorrhage, and can assess the fetus for fetal heart tones, activity, and approximate gestational age. While ultrasonography is useful for identifying fetal heart tones and fetal movement, it is not as accurate in diagnosing uterine rupture or placental abruption, and it may be more technically difficult for advanced third-trimester pregnancy.82
The identification of free intraperitoneal fluid may be related to hemorrhage from solid organ injuries or amniotic fluid from uterine rupture or both. Ultrasonography should not be considered a reliable method for the specific identification of uterine rupture. The presence of an intrauterine organized hematoma and/or oligohydramnios, however, may suggest this diagnosis. Finally, although ultrasonography can be utilized to confirm immediate fetal viability, it cannot be used to rule out fetal–placental injury. While ultrasonography is used as an adjunct for the diagnosis of placental abruption, it is not sufficiently sensitive to exclude this diagnosis.82 Continuous cardiotocographic monitoring, which has been demonstrated to accurately detect significant placental abruption, should be utilized as early as possible for all pregnant patients with significant blunt trauma.83 (Please see Chapter 15, “Second- and Third-Trimester Pregnancy,” for further reading.)
PEDIATRIC TRAUMA
The role of the E-FAST examination in evaluating pediatric trauma patients is discussed in Chapter 20, “Pediatric Applications.”
 SUBACUTE TORSO TRAUMA
SUBACUTE TORSO TRAUMA
Patients occasionally present one or more days after the traumatic event with complaints of chest or abdominal pain. The issues of evolving hemothorax, hemoperitoneum, or subcapsular organ hemorrhage should be considered. When solid organ injuries are strongly considered, CT scanning is the preferred diagnostic method. When the index of suspicion is lower, bedside ultrasonography can be utilized to confirm the absence of unexpected abnormalities. A common scenario is a patient with suspected left-sided rib injuries who has left upper quadrant abdominal tenderness on examination. With subacute trauma, a splenic injury is likely to have evolved to the point where it could be detected by ultrasonography. The confirmation of a normal perisplenic ultrasound examination (without hemoperitoneum or subcapsular hemorrhage) would validate the clinician’s suspicion of an isolated rib cage injury. In this case, an unexpected abnormal ultrasound examination would significantly alter the patient’s treatment and disposition. It is likely that contrast-enhanced ultrasonography will be utilized in the future as an adjunct for identifying patients with occult injuries from subacute trauma.
UNDIFFERENTIATED HYPOTENSION
The role of the E-FAST examination in evaluating undifferentiated hypotension is discussed in Chapter 8, “Critical Care.”
 ANATOMIC CONSIDERATIONS
ANATOMIC CONSIDERATIONS
The shape of the peritoneal cavity provides three dependent areas when a patient is in the supine position. These areas are divided by the spine longitudinally and the pelvic brim transversely. The site of accumulation of intraperitoneal fluid is dependent on the position of the patient and the source of bleeding.13 Free intraperitoneal fluid has the propensity to collect in dependent intraperitoneal compartments formed by peritoneal reflections and mesenteric attachments (Figure 5-5).
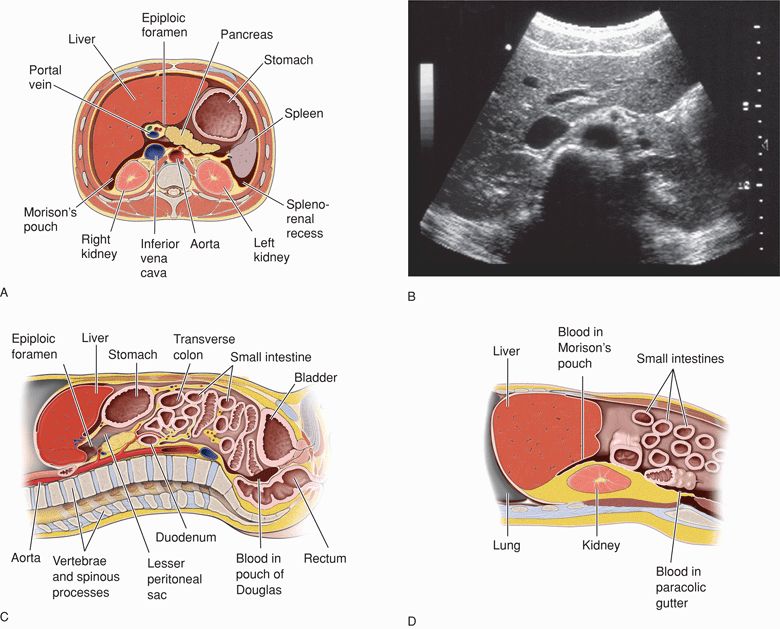
Figure 5-5. Transverse illustration of the upper abdomen that demonstrates the dependent compartments where free intraperitoneal fluid may collect (A). A transverse ultrasound view of the normal upper abdomen is depicted for comparison (B). Longitudinal illustration of the midline (C) and right paramedian abdomen (D) demonstrate the dependent compartments where free intraperitoneal fluid may collect. A longitudinal ultrasound view of the normal right upper abdomen is depicted for comparison (E). (B, E: Courtesy of Gulfcoast Ultrasound; A, C, D: Adapted from Mark Hoffmann, MD)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 CLINICAL CONSIDERATIONS
CLINICAL CONSIDERATIONS CLINICAL INDICATIONS
CLINICAL INDICATIONS ACUTE BLUNT OR PENETRATING TORSO TRAUMA
ACUTE BLUNT OR PENETRATING TORSO TRAUMA TRAUMA IN PREGNANCY
TRAUMA IN PREGNANCY SUBACUTE TORSO TRAUMA
SUBACUTE TORSO TRAUMA ANATOMIC CONSIDERATIONS
ANATOMIC CONSIDERATIONS GETTING STARTED
GETTING STARTED TECHNIQUE AND NORMAL ULTRASOUND FINDINGS
TECHNIQUE AND NORMAL ULTRASOUND FINDINGS COMMON AND EMERGENT ABNORMALITIES
COMMON AND EMERGENT ABNORMALITIES COMMON VARIANTS AND SELECTED ABNORMALITIES
COMMON VARIANTS AND SELECTED ABNORMALITIES PITFALLS
PITFALLS CASE STUDIES
CASE STUDIES