Key Points
- •
The EFAST (Extended Focused Assessment with Sonography in Trauma) exam includes rapid assessment for intra-abdominal hemorrhage (right upper quadrant (RUQ), left upper quadrant (LUQ), and pelvic windows), hemopericardium (subxiphoid window), and pneumothorax and hemothorax (thoracic and pleural ultrasound).
- •
Only five anatomic locations are capable of accumulating sufficient blood in blunt trauma to produce instability: chest , belly , pelvis , femurs , and floor (external hemorrhage). Hemorrhage into the pelvis can be more challenging to diagnose, and ultrasound has a low sensitivity to identify retroperitoneal hemorrhage.
- •
A negative EFAST exam is a key component of the complex decision-making process regarding the need for computed tomography (CT) imaging in patients with low-risk abdominal trauma, especially in young patients in whom exposure to ionizing radiation from CT imaging should be minimized.
Background
Many studies have demonstrated the utility of ultrasound in thoracoabdominal trauma. Evidence and techniques for pleural and cardiac assessments have been covered in previous chapters. This chapter presents the Extended Focused Assessment with Sonography in Trauma (EFAST) exam and describes clinical scenarios to synthesize techniques into comprehensive algorithms for the four main types of trauma:
- 1.
Unstable penetrating trauma
- 2.
Unstable blunt trauma
- 3.
Stable penetrating trauma
- 4.
Stable blunt trauma
General Principles
Principles of advanced trauma life support (ATLS) remain the guiding and unifying language of trauma care. In the current ATLS guidelines, ultrasound is considered an adjunct to the primary survey. Given the exponential dissemination of point-of-care ultrasound techniques and technology, coupled with its obvious superiority to traditional primary survey techniques, such as chest auscultation, ultrasound should be integrated within rather than in addition to the primary survey. Cases and approaches presented below assume that ultrasound is fully integrated into the ABCs of the primary survey.
Differentiation of trauma as “stable” versus “unstable” is critical yet contentious. For the purposes of this chapter, “unstable” refers to symptomatology of life-threatening conditions (stridor, severe dyspnea, dense coma, significant external hemorrhage), or unresponsive states of hemodynamic compromise. The impact of ultrasound in trauma has shown to be different between the stable and unstable populations. In unstable patients, ultrasound directs immediate decision making and interventions and can potentially save lives, whereas in stable patients, ultrasound expedites care, reduces unnecessary ancillary testing, and can educate providers.
The FAST (Focused Assessment with Sonography in Trauma) exam was originally designed to assess for both intra-abdominal hemorrhage (RUQ, LUQ, and pelvic windows), as well as hemopericardium (subxiphoid window). Over time, the examination has expanded to include assessment for pneumothorax (PTX) and hemothorax (HTX). This composite examination, involving assessment of life-threatening traumatic conditions in the pleural, pericardial, and peritoneal spaces, has been designated as the extended FAST or EFAST exam. The following four cases highlight the integration and interpretation of the EFAST exam into the care of critically injured patients.
Case Studies
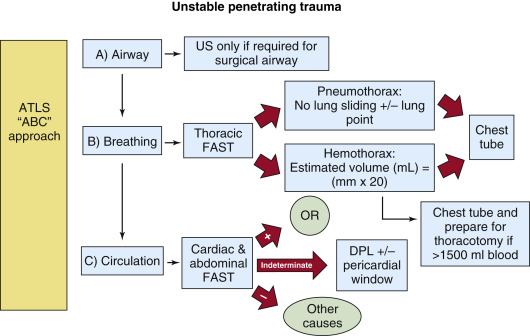
Unstable Penetrating Trauma
A 23-year-old man presents directly to the emergency department (ED) after being stabbed in the epigastrium. His blood pressure on presentation is 90/40 with a heart rate of 115. He is alert and oriented, speaking in full sentences ( Figure 41.1 ).

A (Airway)
Prophylactic intubation can be considered given the predicted course. Delayed airway management is preferred given the hemodynamic consequences of induction medications and positive-pressure ventilation. Ultrasound is not essential in airway management but has been well described for both confirming endotracheal tube (ETT) placement or in the rare assessment for surgical airway.
B (Breathing)
Ultrasound provides critical information immediately on arrival of the patient without waiting for a portable chest x-ray. PTX can be ruled in by the presence of lung point and ruled out by the presence of normal lung sliding ( ![]() ), or by any non-A pattern of pulmonary parenchyma (see Chapter 9 for more information on lung ultrasound). Other conditions can cause absence of lung sliding (bullae, adhesions), but in the setting of trauma, absence of lung sliding calls for liberal use of tube thoracostomy (TT), and in an unstable patient the absence of sliding should lead directly to TT, with or without prior needle decompression depending on provider comfort and preference. Additionally, HTX can be detected and quantified in milliliters by multiplying a rough measurement of the distance from the diaphragm to the inferior aspect of the lung by 20 ( Figure 41.2 ). This approximation of HTX volume is clinically useful when a massive HTX (>1500 mL) is anticipated. Providers may begin the process to transfuse blood and plasma, prepare an autotransfusion device, and discuss the need for thoracotomy while the chest tube is in the process of being inserted.
), or by any non-A pattern of pulmonary parenchyma (see Chapter 9 for more information on lung ultrasound). Other conditions can cause absence of lung sliding (bullae, adhesions), but in the setting of trauma, absence of lung sliding calls for liberal use of tube thoracostomy (TT), and in an unstable patient the absence of sliding should lead directly to TT, with or without prior needle decompression depending on provider comfort and preference. Additionally, HTX can be detected and quantified in milliliters by multiplying a rough measurement of the distance from the diaphragm to the inferior aspect of the lung by 20 ( Figure 41.2 ). This approximation of HTX volume is clinically useful when a massive HTX (>1500 mL) is anticipated. Providers may begin the process to transfuse blood and plasma, prepare an autotransfusion device, and discuss the need for thoracotomy while the chest tube is in the process of being inserted.

C (Circulation)
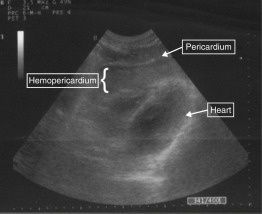
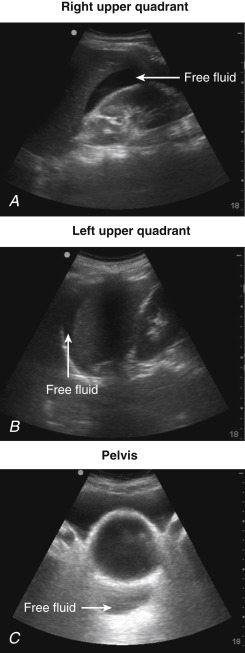
Epigastric wounds, such as the one pictured in Figure 41.1 , are equally prone to lacerate the liver or myocardium. The EFAST exam can differentiate these two sources of bleeding. The presence of pericardial fluid (blood) is an indication for immediate thoracotomy or sternotomy ( Figure 41.3 and ![]() ). False-negative findings for cardiac injury may occur when a hemopericardium is draining into a left HTX. Detection of abdominal free fluid in any of the three abdominal views mandates immediate laparotomy ( Figure 41.4 ). Equivocal findings for either pericardial or abdominal aspects of the EFAST exam should be followed by invasive testing, subxiphoid pericardial window, or diagnostic peritoneal lavage (DPL), respectively, but in more stable patients, a CT scan may be obtained. Negative findings on both abdominal and pericardial components of the EFAST exam should lead to consideration of alternative causes of instability, including retroperitoneal blood loss (see algorithm, Figure 41.5 ).
). False-negative findings for cardiac injury may occur when a hemopericardium is draining into a left HTX. Detection of abdominal free fluid in any of the three abdominal views mandates immediate laparotomy ( Figure 41.4 ). Equivocal findings for either pericardial or abdominal aspects of the EFAST exam should be followed by invasive testing, subxiphoid pericardial window, or diagnostic peritoneal lavage (DPL), respectively, but in more stable patients, a CT scan may be obtained. Negative findings on both abdominal and pericardial components of the EFAST exam should lead to consideration of alternative causes of instability, including retroperitoneal blood loss (see algorithm, Figure 41.5 ).