Grade I
Contusion
Any size
Laceration
Skin and subcutaneous tissue
Fracture
<3 adjacent ribs
Nondisplaced clavicle
Grade II
Laceration
Skin, subcutaneous, and muscle
Fracture
>3 adjacent ribs
Open or displaced clavicle
Nondisplaced sternum
Scapular body
Grade III
Laceration
Full thickness including pleura
Fracture
Displaced or flail sternum
Unilateral flail segment <3 ribs
Grade IV
Laceration
Avulsion of chest wall tissues with underlying rib fractures
Fracture
Unilateral flail chest >3 ribs
Grade V
Fracture
Bilateral flail chest
More than two-thirds of cases of chest wall trauma are the result of a motor vehicle collision (MVC). Other causes include falls from height, sport injuries, motorcycle/bike accident, or of blows from blunt objects.
Imaging plays an important role in the diagnosis. CXR is typically used as the first and, in most cases, as the only diagnostic technique. Multi-detector computed tomography (MDCT) must be performed in stable polytrauma patients or in doubtful cases at initial plain film study and has a very high sensibility and specificity; it can demonstrate significant disease in patients with negative initial CXR images, thus changing their clinical management [4].
11.2 Anatomy of the Chest Wall
11.2.1 Bones
The rib cage surrounds the thoracic cavity and supports the pectoral girdle (shoulder girdle, scapulae, and clavicles), enclosing the thoracic organs and with its muscle being a component of the human respiratory system.
In its normal shape, the human thoracic cage consists of 12 pair of ribs, the sternum, and the 12 thoracic vertebrae.
11.2.1.1 Ribs
About 1 in 200–500 people have an additional cervical rib, with female predominance. Bifid ribs (with the sternal end cleaved in two) occur in about 1.2% of the population. An extra cervical rib, from the seventh vertebra is also a common variant, which may mechanically interfere with the nerves (brachial plexus) going to the arm.
Ribs that articulate directly with the sternum are called true ribs (the first seven), whereas those that connect indirectly via cartilage are termed false ribs.
The last two pair of ribs are called floating rib, attached only to the vertebrae, not to the sternum.
Between the ribs there are the intercostal spaces, containing the intercostal muscles, nerves, arteries, and veins.
Each rib consists of a posterior head and neck, attached posteriorly to the thoracic vertebrae (the insertion point of the longissimus dorsi muscle), a body and a cartilaginous anterior part articulating with the sternum.
Ribs body has a flattened shape with a lateral convex face and a concave medial face, two margins: a smooth superior one and an inferior one, where there is a rut due to the passage of the intercostal nerves and vessels.
11.2.1.2 Thoracic Spine
Dorsal vertebrae, in number of 12, compose the middle segment of the vertebral column, between cervical and lumbar spine.
They are distinguished from the other ones by the presence on either side of the bodies of two semi-facets articulating with the ribs heads and the presence of complete facets on the transverse processes, except for the 11th and 12th one, joining them with the ribs tubercula.
Pedicles and laminae are broad, thick, and directed backward and slightly upward.
Spinous processes are long and triangular shaped, directed obliquely downward, arising from the lamina with a pointed end.
Superior and inferior articular processes arise at the junction between pedicles and laminae, articulating the vertebrae with the one below and above.
Posterior to the latter ones the transverse processes arise, directed obliquely backward and laterally.
11.2.1.3 Sternum
The sternum is a flat bone, forming the middle portion of the front of the thorax. It consists of three parts, from the top: manubrium, body, and xiphoid process.
The manubrium is the upper part of the sternum. It has a quadrangular shape, with a superior jugular notch, located in the middle part of the manubrium; its lateral surface presents two clavicle notches, articulating with the medial parts of the clavicles and the costal notches, articulating with the first pair of ribs.
The manubrium, in his lower part, articulates with the body of the sternum, with a synarthrosis, (the angle between the manubrium and the body is named angle of Louis) laterally at this point there is the attachment of the second pairs.
The sterno-pericardial ligament attaches the pericardium to the posterior side of the manubrium.
The body of the sternum, the longest part, is flat with a front and back surface. Laterally, there are the costal notches, articulating with the ribs.
The xiphoid process is located at the inferior end of the body of the sternum and might remain cartilaginous also in the elderly people.
11.2.1.4 Clavicle
Clavicle or collarbone is a long bone between the scapula and the sternum, with a body, a medial and a lateral end. Clavicle body is flat, forming a superior and posterior face with two margins; the superior and posterior face gives attachment to many muscles: deltoid, trapezius, subclavius, pectoralis major, sternocleidomastoid, and sterno-hyoid muscles.
11.2.1.5 Scapula
The scapula is a flat bone with a lower apex and a triangular shape, attached to the rear face of the rib cage, forming the shoulder skeleton, articulating with humerus at its lateral margin with the glenoid cavity.
It has an anterior and a posterior face, with three margins: a medial, a lateral, and an upper one. The anterior face is concave, with the attachment of the subscapular muscles.
The posterior one is divided into two parts due to a bone process, named spine, dividing it into a small supraspinous fossa and in the larger infraspinous fossa.
The spine becomes more prominent assuming a triangular shape, constituting the so-called acromion, articulated with the clavicle.
The superior margin has a bone process called coracoid process, giving attachment to ligaments and muscles (biceps and pectoralis minor muscle) [5].
11.2.2 Muscles
Chest muscles may be divided into intrinsic and extrinsic according to their origin and insertion entirely in the thorax. Intercostal, levatores costarum and transversus thoracis muscles are the only intrinsic chest muscles.
11.2.2.1 Intrinsic Muscles
Intercostal muscles are a group of three muscles, located between the ribs in order to reduce or increase the size of the rib cage during respiration. They are the external intercostal, internal intercostal, and the innermost intercostal muscles.
External intercostal muscles are obliquely oriented, from the lower edge of a rib to the upper part of the lower one and functioning to elevate the ribs as an inspiratory muscle. The internal intercostal muscles are oriented postero-inferiorly and functions to depress the ribs, as an expiratory muscle. The innermost intercostal muscles are a thin layer of fibers oriented similarly to those of the internal intercostal, separated from them by the intercostal neurovascular bundles.
The intercostal blood supply is derived from the posterior intercostal branches of the aorta and the anterior intercostal branches of the internal thoracic artery.
Other intrinsic muscles are the levatores costarum muscles: they are 12 in number on either side, with a triangular shape, lateral to the spine, originating from the transverse processes of the vertebrae ending on the upper edge of the rib below, with the role of helping in inspiration.
Another intrinsic muscle is the transversus thoracic muscle that is a flat muscle, originating from the body and the xiphoid process of the sternum, ending on the cartilaginous part of the ribs from the second to the sixth, helping in expiration.
11.2.2.2 Extrinsic Muscles
Extrinsic muscles include thoracoappendicular, spinoappendicular, spinocostal muscles, and the diaphragm.
The pectoralis major is a fan-shaped muscle, originating from the medial clavicle, the antero-lateral surface of the sternum, the costal cartilages (from second to sixth ribs) and inferiorly from rectus muscle fibers and the aponeurosis of the external oblique muscle; inserting on the lateral lip of the bicipital groove of the humerus. Its actions are to flex, adduct, and rotate the arm medially.
The pectoralis minor muscle is located deep to the pectoralis major and mainly acts as an inspiratory muscle, also stabilizing the scapula. It originates from the outer face and the posterior margin of the third, fourth, and fifth ribs, near the costal cartilages. Its fibers are obliquely oriented superiorly and converge at the apex of the coracoid process of the scapula.
The serratus anterior is located on the side of the chest wall; this muscle is embedded in the vertebral border of the scapula and originates from the first ten ribs. It is usually divided, given its size, in three parts depending on where the fibers originates from the ribs and where they fit exactly in the shoulder bone. This muscle mainly acts abducting and externally rotating the scapula as well as make it adhere to the chest (the latter action coupled to the rhomboids and trapezius muscles). It lowers the shoulder blades with his lower beams, raises them with the upper beams. If taken as a fixed point elevates the coasts participating in the forced inspiration (inspiratory accessory muscle) [6].
11.3 Mechanisms of Injury
Four main mechanisms of injury are responsible for chest wall injury: direct chest impact, thoracic compression, rapid acceleration/deceleration, and blast injury.
Direct impact injuries are normally less risky, affecting mainly only the soft tissues and muscles of the chest wall (hematomas, bruises, cuts, and scratches). On occasion, a localized injury to the osseous part may occur, mainly rib fractures, but also sternal fracture and sternoclavicular dislocation. Rarely direct impact forces may be transmitted through the chest wall to the deeper organs, causing serious injury to the heart, lung, or large mediastinal vessels.
In the thoracic compression injuries, the chest wall is put against a fixed anatomical bone structure, anteriorly the ribs or sternum and posteriorly the vertebrae causing deep organs laceration, contusion, or rupture. Thoracic compression may cause contusion or laceration of lung parenchyma, pneumothorax or hemothorax, tracheobronchial fractures as well as rupture of the diaphragm.
In acceleration/deceleration injuries, the production of shearing forces causes direct compression against fixed points. This type is the most common and potentially lethal injury, may causing major tracheobronchial disruption, cardiac contusions, aortic, and diaphragmatic rupture [7].
Blast injuries are increasing recently, resulting from the sudden conversion of a solid or liquid material into gas after activation of explosive material. A primary blast injury results from the creation of a blast pressure wave, applying pressure differentials, mostly at air-tissue interfaces within the chest wall, affecting mainly the pulmonary and gastrointestinal systems.
11.4 Anterior Rib Fractures, First Rib and Lateral Rib Fractures
11.4.1 Pattern of Injury
Rib fractures are the most common injury after blunt chest trauma which occurs in approximately 50% of patients. It is important to consider the specific location of rib fractures because this is an important indicator of related injury. Rib fractures can be studied as three distinct patterns according to their location: (1) fractures of the first rib and those of the second to fourth ribs, (2) fractures of the fifth to ninth ribs, and (3) fractures of the 10th to 12th ribs. These three distinct patterns of rib fractures represent different pathophysiology and associated morbidity. A rib score has been proposed to predict adverse pulmonary outcomes [10].
A high-energy trauma is necessary to result in fracture of the first, second, or third ribs because these ribs are well protected by the scapulae, clavicles, and musculature. The presence of this fracture should prompt the evaluation of vascular thoracic injuries, brachial plexus injury, or subclavian vascular injuries [11].
Isolated first rib fractures are seen in association with cranial and maxillofacial injuries and are probably secondary to avulsion of the first rib by its muscular attachment rather than direct trauma to the rib, which is relatively protected.
Fractures of the fourth up to the eighth ribs are the most common [12].
The compression of the rib cage with associated fracture of the 10th, 11th, or 12th rib might cause internal abdominal organs injuries, of course fractures of the right lower ribs are more often associated with hepatic injury, fractures of the left lower ribs with splenic injury, and fractures of the posterior portion of the lower ribs with renal injury.
Injury to the liver might result in tearing, intraparenchymal or subcapsular hematoma, active bleeding, or there might be injury of major liver vessels. Injury of the spleen or kidney might result in subcapsular hematoma or abdominal rupture in greater force impact. Even hemorrhage around and within the adrenal glands represents a risk that is associated with fractures of the lower ribs.
Fracture of any rib can be associated with pneumothorax, hemothorax, or extrapleural hematomas. Although lung trauma is generally seen immediately, the occurrence of a pneumothorax and hemothorax may be delayed for hours after the injury. Hemothorax of a significant degree secondary to rib fractures is usually the result of laceration of an intercostal artery rather than bleeding from the lung. It is important in the evaluation of rib fractures to check in particular the lower sulcus of the ribs where the intercostal arteries are located; fractures that involve the sulcus are more prone to hematomas and the hemothorax resulting from a laceration of an intercostal artery can be life threatening.
The risk of intra-abdominal or intrathoracic injury increases if two or more rib fractures are present at the same level [13–15]. These injuries should always be ruled out by MDCT [16].
Elderly individuals are prone to rib fractures because of decreased rib cage compliance; limited respiratory movement may cause an increased prevalence of atelectasis and subsequent pneumonia which lead to pulmonary insufficiency, even from single rib fractures, that may increase morbidity and mortality [11, 17].
A study showed that in elderly people more than three rib fractures may indicate the need to transfer to a trauma center, and the more ribs broken, the greater the death rate [18].
In contrast, children’s bones are immature and more compliant, due to the greater pliability of children’s ribs, greater force is required to produce a fracture and rib fractures in this group of patients are indicative of high-energy transfer trauma [4, 9].
Anyway in elderly and not elderly people, knowing the number of ribs fractured might influence treatment decisions and might change morbidity and mortality.
A single blow may cause rib fractures in multiple places. At the level of the rib cage, the typical pattern of fractures varies depending on the site of compression: if the compression comes from the front we usually observe sternal compression fractures and antero-lateral rib fractures; if the compression comes from the back we usually observe posterior rib fractures; if a lateral force occurs, we usually observe posterior fractures and detachment from the costochondral cartilage or anterior fractures.
If the compression is anterior and posterior, lateral rib fractures occur on the lateral cortical margins; if the force is laterally direct to the ribs, internal cortical rib fracture might occur (Fig. 11.1).


Fig. 11.1
Chest trauma: different mechanisms of injury secondary to different axial load force (arrows). (a) Lateral impact. (b) Anterior-posterior impact
Traumatic fractures most often occur at the site of impact or the posterolateral bend, where the rib is the weakest. Both displaced and nondisplaced fractures can be seen in adults and children.
Fractures might be anterior; there might be lateral fracture with rib cage deformation and posterior fractures occasionally involving the costovertebral joint; it is important to note that buckle fractures are easy to overlook even at CT and additional coronal image scan be helpful in the diagnosis of rib fractures that are not seen on axial images [19, 20].
11.4.2 Imaging Evaluation and Findings
11.4.2.1 Plain Radiography
A standard CXR is almost always the initial study for the evaluation of non-traumatic chest pain and for traumatic injuries. If rib fractures are suspected clinically, a rib plain film series might be performed; this radiograph consists of oblique views and optimization of the X-ray parameters by the technologist to highlight bony detail. The decision to image a rib fracture in the absence of other underlying abnormalities or associated injuries depends on the clinical scenario.
Even in the absence of associated injuries, radiographic confirmation of a rib fracture can help prevent complications such as atelectasis and is particularly important in patients with comorbidities such as chronic obstructive pulmonary disease, cardiac disease, hepatic disease, renal disease, dementia, and coagulopathy.
11.4.2.2 MDCT
MDCT is the study of choice to fully evaluate trauma-associated injuries and bony details; it is the most sensitive technique for imaging rib fractures since it can help determine the site and number of fractures. It is however relatively costly, time-consuming, not always 24 h available, and exposes the patient to a significant amount of radiation [21].
With the help of reconstructed maximum intensity projections (MIP) and volume-rendered (VR) images, MDCT depicts with great detail the number and sites of rib fractures [12].
MDCT angiography plays a crucial role in the evaluation of the vascular injuries associated with chest trauma and should be considered in stable patients with first rib fractures if there are absent or decreased upper extremity pulses, if regional hemorrhage, and/or brachial plexus injury are present. Additional criteria for angiographic MDCT include displacement of bone fragments and multiple thoracic injuries.
11.4.2.3 US
Ultrasonography (US) can be used to look for broken ribs and costal cartilage fractures, in cases in which they occur in an accessible thoracic point, especially in pediatric population and in young women. Unfortunately, US is unable to adequately assess certain portions of the thorax such as the first rib under the clavicle, and the upper ribs under the scapula.
Other limitations include subcutaneous emphysema and the pain at the site of the transducer compression, making it difficult in traumatized patients; and its results depend greatly on the skill of the performer [23]. Even if with these limitations, US might demonstrate cortical discontinuity, linear edge shadow (Fig. 11.2), and acoustic reverberation artifacts in accessible points and associated injuries such as pneumothorax and hemothorax; abdominal organ injuries might be evaluated too.


Fig. 11.2
US imaging showing interruption of cortical margins and a 2.9 cm hematoma after chest wall trauma (calipers)
Studies have found it to be much more sensitive than plain radiography in detecting rib fractures, whereas other studies have suggested that it is only equally sensitive or slightly better, but it should be underlined that US is not as panoramic as plain radiography and MDCT.
11.4.2.4 MRI
Magnetic resonance imaging (MRI) has not yet a role in rib fracture evaluation and is not considered appropriate for evaluating rib fractures, due to the fact that it is time-consuming and not easily available in trauma centers. However, it may be useful if there is concern about soft-tissue or vascular abnormalities [21].
11.4.3 Natural History and Mortality
Pain from rib fractures can be severe for several days following the injury and even if most of them heal within 6 weeks, many patients are able to resume daily activities much sooner. Follow-up CXR after the injury are not routinely recommended and should be performed only if indicated by clinical findings or if in complicated cases [24]. Clinical signs of worrisome might be unilateral decreased breath sounds suggesting pneumothorax or persistent pain suggesting difficult consolidation or nonunion. A follow-up examination 6–8 weeks after the injury is reasonable to assess the patients, if they are unable to return to sports or work by that time.
The number of displaced rib fractures and fracture location could be a significant predictor for developing pulmonary and other organs complications. For patients with fewer than three rib fractures without rib displacement and initial lung or other organ injuries, conservative management could be safe and efficient [25].
As the number of rib fractures increases, morbidity and mortality grows substantially in all age groups owing to major risk of complications such as pneumothorax, pneumonia, and acute respiratory distress syndrome (ARDS).
Other associated injuries such as concomitant great vessel injury might happen in 3% of traumatic injuries to the first rib that affect prognostic outcome. Pneumothorax occurs in about 14–35% of rib fractures, hemopneumothorax in 20–25%, pulmonary contusions in 17%, and a flail chest in 5.8%.
Chest wall injuries in older people should not be dismissed. Older patients have twice the morbidity and mortality compared with younger people; for every increase in the number of ribs fractured, mortality increases by 19% while the risk of pneumonia increases by 27%.
11.4.4 Treatment
Simple rib fractures themselves are usually not significant in isolation and are treated symptomatically. They have a good prognostic outcome and are rarely life threatening [12].
Virtually, all non-pathologic rib fractures heal well with conservative management. Some patients are able to return to work within a few days, depending on their occupation. One small case series suggests that some patients experience prolonged pain and disability [26]. It found that patients with an isolated rib fracture regain pain-free function at a mean of 51 days.
11.5 Costochondral Injuries
Costochondral injuries refer to the fracture at the joints between each rib and its costal cartilage. They are primary cartilaginous joints and represent the demarcation of the unossified and ossified part of the rib. There is no movement at these joints. Costal cartilages form part of the thoracic cage and anterior chest wall. There are ten costal cartilages, one for rib 1–10, each of which forms a costochondral joint. Costal cartilages 1–7 articulate with the sternum at sternocostal joints, and costal cartilages 8–10 are attached to each other via small interchondral synovial joints forming the costal margin.
11.5.1 Patterns of Injury
Costal cartilage fractures are rare lesions, which may be located at the chondrocostal or chondrosternal junction.
While in adult patient pain is the primary complaint, in young children, a costal cartilage fracture may present as a thoracic wall mass associated with pain.
Costochondral injuries might occur in three locations: costochondral, midchondral, and sternochondral. Disruptions or fractures of costal cartilage might result in an unstable rib cage and may expose thoracic contents, such as the heart, to injury.
While the more fixed first and second rib seems to be easily subjected to costochondral separation, the lower ribs can suffer costal cartilage fracturing more frequently.
11.5.2 Imaging Evaluation and Findings
11.5.2.1 Plain Radiography
Fractures of the costal cartilages are challenging to establish on physical examination and on plain radiographs, where they are easily overlooked. However, when there is severe calcification of the cartilage, a traumatic interruption might be displayed at this level [27, 28].
CXR is indicated to show associated findings such as pneumothorax, hemothorax, pulmonary contusion, and subcutaneous emphysema.
11.5.2.2 MDCT
11.5.2.3 US
US is a reliable method to diagnose costal cartilage fractures and can increase the sensitivity of their detection when used together with MDCT scanning. US is preferable in a pediatric population, in young or pregnant women and for follow-up examinations [30].
In pediatric population, US examination might be useful when costal cartilage fracture presents as a chest wall mass associated with pain to exclude neoplasm or post-traumatic hematoma.
Furthermore, it is suggested an US examination when there is a high clinical suspicion and other modalities have not demonstrated an injury.
Sonographic signs of a cartilage damage include a fracture line, disruption of the anterior echogenic margin, a step-off deformity or gas located at the costochondral junction [27, 31].
Pitfalls in US examination include false fractures that might be produced when the probe overlies the rib and partly the intercostal space. Also costal cartilage calcifications, running parallel to the rib margin, at the costochondral junction, may give rise to the false identification of a fracture due to normal sharp indentation (less likely in pediatric population) [32].
11.5.2.4 MRI
MRI can easily demonstrate costal cartilage fractures and, like US, doesn’t result in radiation exposure.
Costal cartilage injuries are detected on MRI due to the high T2 signal from the surrounding edema, and they are often more easily detectable than on MDCT. Even in cases of remote injury, persistent high T2 signal at the site of fracture might be seen, presumably due to nonunion in persistent clinical symptoms.
When costochondral injury is suspected, a fat-saturated T2-weighted or STIR sequence in the coronal view are recommended [33].
11.5.3 Natural History and Mortality
Costochondral fractures slightly increases mortality rate as they may determine rib cage instability and flail chest, impairing respiratory function [34].
11.5.4 Treatment
These injuries are usually treated like the osseous rib fractures, typically with nonsurgical management involving ice, nonsteroidal anti-inflammatory medications and taping of the ipsilateral chest wall or use of a rib belt; in addition, athletes are restricted from sport for 3 weeks or longer [33, 35, 36].
However when returning to sports, especially contact sports at risk for direct trauma (e.g., hockey, rugby), a protective padding may be used to allow for further healing while reducing the risk of any repeated injury.
11.6 Flail Chest
A flail chest deformity may be a severe consequence of multiple rib fractures. It occurs when three or more contiguous ribs are fractured in two site, or five or more contiguous ribs are fractured in one site with or without associated sternal fractures [37].
With regard to injury mechanism, such trauma may be caused by MVC, falls, and assaults in younger, healthy patients.
The initial diagnosis of flail chest is performed with physical examination, when paradoxical or reverse motion of a chest wall segment is detected while spontaneously breathing. This pattern of injury gives the rib cage an unstable dynamic of motion because a segment can act as a flail segment. The movements of this segment are opposite to the expected in the dynamic of the rib cage motion: in inspiration the unstable segment of the rib cage is attracted towards the pleura and in expiration it goes away from it. In this pattern of fracture in a non-ventilated patient, this segment of the rib cage movement is contrary to the expected and is called paradoxical. The segment of the chest wall that is flail is unable to contribute to lung expansion. This abnormal movement hinders the creation of negative intrathoracic pressure during inspiration and positive airway pressure during expiration.
The force that is needed to produce a flail chest varies on the structure on which it impacts, if the structural components (i.e., the ribs) are weakened for any reason (i.e., osteoporosis, total sternotomy, and multiple myeloma, as well as individuals with congenital absence of the sternum), then much lower force may be required. Mechanically, however flail chest generally requires a significant traumatic energy diffused over a large area (i.e., the thorax) to create multiple anterior and posterior rib fractures.
The motion of the flail segment is usually limited by the surrounding structural components, the intercostalis, and the surrounding musculature. This mechanical limitation of motion affects the actual size of the changes in thoracic volume and patient-generated tidal volume. Underlying pulmonary or cardiac disease determines the physiologic perturbations to respiration caused by the flail segment.
Although the diagnosis of flail chest is initially clinical, it always requires radiological studies including CXR and MDCT.
11.6.1 Patterns of Injury
The chest wall is inherently stable, with 12 ribs attaching posteriorly to the spinal column and anteriorly to the sternum. Intercostal muscles with fascial attachments, coupled with other muscle groups, including the trapezius and the serratus groups, add further strength to the bony cage around the thoracic organs.
Borrelly and Aazami [38] reported that contraction of the serratus anterior muscle digitations pulls the flail segment posteriorly and superiorly. Canine flail chest experiments have also shown that the degree of inward inspiratory displacement is related to force differences between intrapleural pressure and parasternal muscle activity [39].
Frontal and lateral impact may result in multiple anterior and posterior rib fracture points. Severe anterior compressive forces may cause sternochondral disruption and a subsequent sternal flail.
Flail chest can be subdivided into anterior and posterior flail chest depending on the presence of fractures along the anterior or posterior rib angles, respectively [40]. Flail segment might include the sternum with ribs on both sides of the thoracic cage fractured.
The rib cage is a flexible ring-like structure; the arch design of the ribs allows some flexing in trauma. The rib cage is less compliant in adults rather than in children and in the latter can absorb small amounts of blunt kinetic energy. Consequently, flail chest in children is observed with lower frequency, rather than injury to the underlying structures. Contrary in an adult, a transfer of significant kinetic energy in blunt trauma to the rib cage or a crushing rollover injury is the most frequent cause of flail chest.
11.6.2 Imaging Evaluation and Findings
Patients with flail chest, resulting from a high-energy trauma, need to be considered at risk for severe associated injuries such as massive pulmonary contusion or laceration, pneumothorax with subcutaneous emphysema, hemothorax (which are the major contributors to respiratory insufficiency) and vertebral fractures.
11.6.2.1 Plain Radiography
CXR is the first examination performed in case of acute chest trauma and the strict definition of three ribs broken in two or more places, or more than five contiguous ribs injured can be confirmed eventually by means of specific ribs plain films too. The inherent structural stability of the chest wall due to the ribs and intercostal muscles usually does not show abnormal or paradoxical motion without three or more ribs involved.
11.6.2.2 MDCT
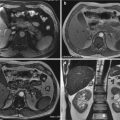
CXR is less sensitive than MDCT for the diagnosis of flail segments, and thoracic MDCT is routinary performed in case of severe trauma with paradoxical chest movements to exclude associated complications, such as pulmonary contusions, usually subjacent to the point of impact or on the counterpoint; lung laceration frequently masked by the surrounding pulmonary contusion; pneumothorax that is very common, but might be not clearly evident on supine CXR; hemothorax; pneumomediastinum; subcutaneous emphysema; mediastinal hemorrhage; and major vascular injuries (Figs. 11.3, 11.4, 11.5, 11.6, 11.7, and 11.8).







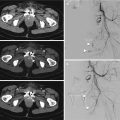
Fig. 11.3
CT scout of a patient underwent to a severe chest trauma after MVA, showing subcutaneous emphysema (long arrow in a, arrow in b) of the left thoracic wall, lung contusions (short arrow in a and in b). Left scapular fracture (arrowhead in a). Not dislocated fracture of the proximal part of the first right rib of the same patient (arrowhead in c). Subcutaneous emphysema in the left neck (arrow in c). Chest wall hematoma without active bleeding (arrowhead in d)

Fig. 11.4
3D reconstruction (a. Left lateral view; b. Left posterolateral view) of a patient underwent to a severe chest trauma, after a MVA, showing flail chest with fractures, in two points, from the second to seventh rib (arrowheads). Left scapular fracture (arrow). Chest, endotracheal, and nasogastric tube placement

Fig. 11.5
Chest X-ray performed in shock room in supine position on the spinal board, in a patient who underwent a severe chest trauma after a MVA, showing subcutaneous emphysema of the right chest wall, multiple rib fractures (arrows), lung contusions (arrowhead). Endotracheal tube placement

Fig. 11.6
CT axial imaging of the same patient showing subcutaneous emphysema (arrow) of the right chest wall, lung contusions (curved arrow). Right pneumothorax (black arrowhead). Chest tube placement (star)

Fig. 11.7
MPR images (a, b) of the same patient showing lung contusions and subcutaneous emphysema (black arrow in b) of the right chest wall and lower portion of the neck (short black arrow in a). Multiple rib fractures (arrowhead in b) and T12 vertebral fracture (long black arrow in a)

Fig. 11.8
3D reconstruction (a. Right posterolateral view; b. Posterior view) of the same patient showing flail chest with fractures from the seventh to twelfth rib. Chest drainage, endotracheal tube, venous catheter placement
11.6.3 Natural History and Mortality
The incidence of flail segments is 10–15% in major thoracic trauma and might be associated with cranial, thoracic, and abdominal injuries.
Early mechanical ventilatory assistance is provided to patients with severe concomitant injuries. The paradoxical movements of the flail segment disappears after intubation with positive pressure ventilation.
Patients may demonstrate only the paradoxical chest wall motion, with minimal respiratory insufficiency, although they usually show some tachypnea with a notable decrease in resting tidal volume due to painful fractures. The impairment of respiratory function is typically related to the underlying lung injury and loss of negative intrathoracic pressure, rather than the chest wall abnormality. It can cause the development of atelectasis and adult respiratory distress syndrome secondary to impaired pulmonary drainage, with progressive hypoxemia, elevated airway pressures, and a progressive infiltrate in the affected lung [41].
Flail chest can lead to severe respiratory failure and requires prompt intensive respiratory ventilation, sometimes also for prolonged periods in more than 50% of cases [12, 37].
Flail chest has a reported mortality rate between 10 and 15% that is primarily caused by associated injuries.
The mortality rate of patients with severe associated injuries may be decreased from 50% to 6% if mechanical ventilation is instituted within 24 h of injury; on the opposite, the mortality rate can exceed 90%, however, when there is hypotension and hypoxia for a period of more than 24 h [40].
Prolonged mechanical ventilation and pulmonary contusion are associated with the development of pneumonia and a poor outcome.
11.6.4 Treatment
Flail chest is usually managed supportively, with adequate analgesia and chest physiotherapy to assist volume expansion and secretion management, and to prevent secondary complications of atelectasis and pneumonia. Adequate analgesia is of paramount importance and may contribute to the return of normal respiratory mechanics.
Chest tube insertion might be necessary in case of complications such as hemo- or pneumothorax.
Posterior flail segments are easier to manage clinically because of the presence of strong muscular and scapular support and because of a patient’s natural tendency to lie with his or her back against the mattress.
The surgical management has traditionally been reserved for the following indications: flail chest who require thoracotomy for other intrathoracic injuries, severe chest wall instability, persistent pain secondary to fracture malunion, and persistent or progressive loss of pulmonary function [40]. Surgical stabilization can effectively reduce the duration of mechanical ventilatory support and facilitating a shorter intensive care unit (ICU) stay and quicker recovery. The long-term benefits include restoration of normal chest wall geometry and improved pulmonary function testing.
Open fixation is also indicated for flail chest when thoracotomy is performed for other concomitant injuries. Rarely, severe rib injuries (e.g., flail chest) may be treated with open reduction internal fixation (ORIF), often in the setting of other severe traumatic injuries and in the hope that respiratory function will improve [12].
11.7 Sternal Fractures, Sterno-chondral Injuries, and Sternoclavicular Dislocation
11.7.1 Sternal Fractures
Sternal fractures usually occur in patients who involved in high-speed motor vehicle collision, with an incidence of 8–10%. Their importance lies in the high frequency of associated injuries such as fractured ribs, pulmonary and cardiac trauma, cranio-cerebral injuries, thoracic and lumbar spinal fractures, whiplash, and lower-extremity injuries [42].
Sternal fractures have associated mediastinal injuries in more than 50% of cases and a mortality of 22% due to cardiac and great vessel lesions.
11.7.1.1 Patterns of Injury
Fractures may occur in any segment of the sternum but most commonly affect the upper third of the sternal body and the manubrium. In 18% of cases, fractures occur at the manubriosternal joint. The fractures of the manubrium, rather than the ones at the sternal body, require higher force [43, 44].
The degree of displacement is proportional to the energy of the impact and, thus, to the likelihood of concomitant injuries.
The most common mechanism of sternal injuries is a direct impact between the sternum and the steering wheel or seat belt or air bag as a result of sudden deceleration. These injuries are more common in front-seat and/or restrained passengers and in frontal collisions.
Fractures may be displaced or undisplaced: an isolated undisplaced sternal fracture is considered a benign entity not associated with appreciable morbidity [45].
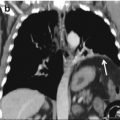
On the contrary, a sternal fracture with displacement or multisystemic trauma may alert the clinician to search for possible associated serious injury. In these cases, displaced fragments are often associated with soft-tissue and cardiothoracic damage due to the posterior shift of the lower fragment. The manubrial fractures may be associated with aortic and brachiocephalic vessel injuries, while the depressed sternal body fractures may determine myocardial injuries in 1.5–6% of patients. A general rule is: the more displaced the fracture, the higher the association with additional chest injuries.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree