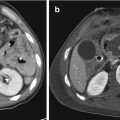
Fig. 12.1
Normal CT anatomy of the anterior, posterior, and lateral/costal part of the diaphragm. (a, b) Axial MDCT images show the anterior diaphragmatic component (arrowheads) and the crura (arrows). (c, d) Axial MDCT scans of the lateral/costal part of the diaphragm show incomplete detection of the muscle where it abuts structures of similar attenuation, such as liver and spleen (arrows in c, d). The diaphragm is well appreciated when it is defined by peritoneal, retroperitoneal, or extraperitoneal fat (arrowheads in c)

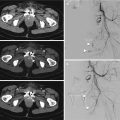
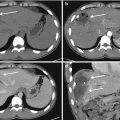
Fig. 12.2
Normal CT anatomy. Coronal (a) and sagittal (b) MPR images contribute to the evaluation of the diaphragmatic profile (arrows). Note the poor visualization of the muscle in the portions next to the liver and the spleen
The pattern and site of TDIs may be influenced by some typical regions of muscular weakness that predisposes to injury and are directly related to embryological development. These points of weakness are located where groups of muscle fibers from different embryological origins meet: the right and left sternocostal triangles and the lumbocostal triangles. Indeed, the majority of injuries occur in the posterolateral areas of the left diaphragm between lumbar and costal muscular attachment, where the pleuroperitoneal membrane finally join with the septum trasversum during embryogenesis [1, 15, 16]. On the right side, the diaphragm is more protected by liver parenchyma from blunt traumatic injuries.
12.1.2 Mechanism of Injury
The most common mechanisms of TDI include blunt and penetrating diaphragmatic trauma: the former results from considerable force and most often occur in high-energy vehicular impact, a fall from a height or a crushing blow; the latter is variable and largely dependent on the nature, velocity, and path of the weapon or projectile [1, 4].
The pattern of a blunt TDI is partially determined by the direction of impact. A lateral impact distorts and elongates anterior-posteriorly the chest wall, shears the stretched dome of the diaphragm, and results in avulsion of its peripheral attachment. A frontal impact leads to a sudden and abrupt increase of the abdominal pressure, with rise of the diaphragmatic gradient and transmission of force to the diaphragm through the abdominal viscera, resulting in a large rupture. In the context of a blunt thoracoabdominal trauma, the diaphragm may also be injured by fractured or fragmented ribs that penetrate the muscle [4, 8, 17, 18].
The penetrating thoracoabdominal wounds, at risk for a diaphragmatic involvement, generally occur anteriorly beneath the fourth intercostal space, laterally beneath the sixth intercostal space and posteriorly beneath the eighth intercostal space [19].
Once the diaphragmatic tear has occurred, the positive pressure gradient, that exists between the peritoneal and pleural spaces, induces abdominal viscera herniation into the thoracic cavity [20].
The mechanism of injury is also influenced by other important factors like the respiratory phase and the position of the patient at the time of the impact, preexistent and congenital alterations of the diaphragm, volume and fullness of abdominal viscera [19].
The knowledge of the mechanism of injury and of the circumstances of trauma, as well as imaging signs, represents an important contribution to the detection of TDIs and helps to avoid a misdiagnosis.
12.1.3 Patterns and Site of Injury
A blunt TDI is generally large, measuring 5–15 cm, and most often occurs in the posterolateral aspect of the muscle, with spread in a radial direction toward the central tendon, following the structurally weak area, corresponding to the embryologic origin of the pleuroperitoneal membrane. Other blunt ruptures of the diaphragm can occur in its central portion and at the costal attachment spreading in a transverse direction. The peripheral diaphragmatic detachment is the least frequent type of rupture observed at surgery (Fig. 12.3) [1, 3, 4, 17].


Fig. 12.3
A drawing showing sites and patterns of diaphragmatic injuries: radial (A), transverse (B), central (C) ruptures, and peripheral detachment (D)
A penetrating trauma, due to stab or gunshot wounds, causes a diaphragmatic injury along the trajectory of the weapon, so it is more variable in location and are usually shorter, measuring 1–4 cm, unless associated with blast injuries. These small defects may be easily missed on the initial MDCT (and even intraoperatively) unless deliberately sought for, especially when accompanied by other more threatening injuries [3, 4, 21]. A left-sided blunt diaphragmatic injury occurs three times more frequently than right-sided one, and this is due to multiple factors. First of all, the liver protects the right diaphragm preventing transmission of increased intra-abdominal pressure generated by the trauma and acting as a sort of buffer. Furthermore, the area between the lumbar and intercostal tendinous attachment represents a congenital structural weakness of the left diaphragm to which contributes the presence of the esophageal hiatus. The relative minority of right-sided injuries may also be associated with the missed diagnosis: indeed, a correct detection of right diaphragmatic lesions results more difficult because the radiologic signs may be subtle, the breach may be obscured by the liver and the herniation may be delayed or absent [1, 8, 20, 22, 23]. Even if an equal incidence of left- and right-sided TDIs is expected from penetrating trauma, the left injuries result to be predominant because most people are right handed [8].
12.1.4 Associated Injuries
The anatomic site of the diaphragm, its adjacency to thoracic and abdominal organs, and the severity of the trauma represent the reason why a blunt diaphragmatic trauma rarely occurs as an isolated lesion and results in a high percentage of associated life-threatening injuries (44–100% of patients) [1, 4, 8, 20]. The most common injuries, associated with a left-sided blunt TDI, involve the spleen, while liver lesions are more frequent with right-sided blunt diaphragmatic injuries. Rib fractures, pneumothorax, and pleural effusion are present in 90% of cases. Associated renal and aortic lesions and pelvic or spine fractures are less frequently encountered [1, 4, 8, 18, 24].
Emergency radiologists have to keep in mind the importance of suspecting a diaphragmatic rupture, especially in cases of high-energy trauma with multiple severe thoracoabdominal injuries.
Concerning penetrating trauma, the occurrence of associated injuries is variable and mainly dependent on the kind of weapon or projectile, on its velocity and trajectory [4, 18]. Anyway, it is fundamental to exclude a TDI before a chest tube placement (in example to drain a pneumothorax) in order to avoid iatrogenic perforations of the herniated viscera, especially in case of a left diaphragmatic rupture.
12.2 Imaging Evaluation and Findings
As previously mentioned, the role of imaging is to identify the abnormality as soon as possible to avoid acute or delayed severe complications that can result from a missed diagnosis. However, the radiologic interpretation is often difficult. The CXR is performed as initial screening study to evaluate the patient in the emergency room, but most radiographic features, concerning a TDI, are often subtle and nonspecific. The MDCT examination represents the second-level imaging necessary to stage a traumatized hemodynamically stable patient; particularly, it allows an accurate evaluation of the injuries, because of the higher quality of axial and MPR images compared to conventional single-slice CT, that showed a lower diagnostic accuracy for the TDI [7, 25–27].
12.2.1 X-Ray Signs
Despite its technical limitations, which include the supine positioning, the use of portable radiography, and the limited patient’s cooperation, a CXR remains valuable as first radiological examination in the acute phase for the detection of a TDI [4]. It is generally performed only in the supine position and frequently it is acquired on the long spine board (LSB) in the shock room. For these reasons, the CXR has a relatively poor sensitivity and specificity, resulting normal or nonspecific in 20–50% of cases of a traumatic TDI, due to the high range of initially unrecognized injuries. Generally, the diagnosis or the suspicion of a left-sided injuries is easier (with detection sensitivity up to 60% of patients) than for right-sided injuries (18–33%) [8, 26, 28]. Indeed, a right TDI is more difficult to detect on CXR, as the liver blocks herniation of abdominal contents into the lower right side of the chest. Moreover, herniation of the liver is often overlooked and differentiation of a herniated liver through a TDI, from other causes of elevated diaphragm, such as atelectasis, pleural effusion, or pulmonary contusion or laceration, remains difficult [4].
The following two are the main radiographic findings that are specific of TDI:

the presence of intrathoracic gastrointestinal air due to the herniation of abdominal viscera into the lower thorax (stomach, small bowel, or colon), with or without an associated focal constriction of the herniated mass at the site of the diaphragm tear, the so-called collar sign (Fig. 12.4)
the visualization of the nasogastric tube above the left diaphragm, when stomach has herniated, with an abnormal U-shaped course [29]

Fig. 12.4
Diaphragmatic rupture: specific CXR signs. Left diaphragmatic elevation associated to abdominal viscera above the diaphragm (arrow in a) and to the presence of intrathoracic gastrointestinal air (arrow in b). Left hemithorax mostly occupied by a gas-filled herniated stomach, associated with a focal constriction at the site of the diaphragmatic tear, indicative of collar sign (arrow in c)
Other common and suggestive, but nonspecific findings of TDI on CXR are:


a diaphragmatic elevation (4–6 cm, or more, above the level of the contralateral diaphragm), especially when the right one is involved (Fig. 12.5)
an obliteration or distortion of the diaphragmatic contour (Fig. 12.6)
a pleural effusion (when the TDI develops a pleural effusion, the underlying diaphragmatic injury may be masked, particularly with small tears not associated with the herniation of abdominal content) [30]

Fig. 12.5
Right diaphragmatic elevation with undefined diaphragmatic contour (black arrow in a), pulmonary atelectasis, and left mediastinal shift, consistent with right TDI and liver herniation, then confirmed by MDCT (white arrow in b). In this case, a right chest tube was improperly positioned, in shock room, to drain a pneumothorax, before having excluded a diaphragmatic rupture

Fig. 12.6
Left diaphragmatic rupture. (a) Supine CXR on spinal board shows nonspecific signs: opacification of the left hemithorax base with lack of visualization of the left diaphragm (black arrow). (b) MDCT: a coronal MPR image clearly demonstrates the left diaphragmatic rupture with hollow abdominal viscera and mesenteric fat herniation (white arrow)
It is important to underline how concurrent pulmonary abnormalities, related to the trauma, such as hemothorax, pulmonary contusion or laceration, atelectasis, and phrenic nerve palsy may mimic or mask a TDI on CXR. In addition, the positive pressure of ventilatory support may delay herniation of abdominal contents through a torn diaphragm. Therefore, the rate of a missed TDI on CXR ranges from 12 to 66%, with the potential risk of a late visceral herniation through the diaphragmatic defect. Anyway, in the presence of both specific and nonspecific CXR findings a MDCT examination is warranted in hemodynamically stable patients to confirm a TDI to assess potential associated injuries and to guide clinical management [1, 4].
12.2.2 CT Signs
The MDCT is nowadays considered the gold standard imaging study for the assessment of a TDI, with a specificity of 76–99% and a sensitivity of 61–100%, considerably higher if compared with the single-layer CT era [8, 10, 20, 32]. Indeed, the improvement of the MDCT technology, such as the use of multilayer scanners, with higher spatial resolution and speed, reduces artifacts and produces high quality MPR images, which are fundamental for diagnosis [33]. If a TDI is suspected, on a clinical and/or a radiographic basis, the hemodynamically stable patients should undergo a whole-body MDCT examination, whereas hemodynamically unstable patients (or patients with signs of acute peritonitis) must be directed to a surgical exploration as soon as possible [6, 20, 34]. The MDCT protocols vary depending upon the type of scanner available, the institution, and the patient’s clinical conditions. Usually, a whole-body MDCT, with intravenous (IV) contrast is performed. In our emergency department, the MDCT examination is composed by three phases: a first non-enhanced phase, from the thoracic inlet through the symphysis pubis to appreciate hyperdense features (such as calcification or blood), an arterial phase (for which it is advisable to use high-flow IV contrast, by means of a power injector) to detect arterial lesion and a venous phase for visualization of parenchymal injuries. The arterial and portal venous scan can be acquired using, respectively, delays of 30 and 70 s, but, for the arterial phase, a bolus tracking or a smart prep technique is preferred. The images should have a thin collimation (2.5–3 mm) and they might afterwards be reconstructed at 0.625–1 mm for the interpretation and post-processing.
Several MDCT findings have been described over the years, which have been classified into three groups [10]: direct and indirect evidence of rupture; uncertain-controversial signs; and associated signs, according to Table 12.1. These signs are highly specific but the sensibility is lower because, in the setting of penetrating trauma, the herniation might be of small size and it might be overshadowed by more critical and severe traumatic injuries. The fundamental role of MDCT is to establish the best therapeutic management for patients with TDI giving clear indications to the emergency clinician and surgeon. As summarized in Table 12.2, the findings specific for a diaphragmatic rupture directly refer the patient to the operating room, while nonspecific findings need a radiological follow-up [8].
Table 12.1
Summary of the TDI findings, classified in three groups, according to their radiological meaning: direct evidence of diaphragmatic rupture, indirect signs hiding the presence of a diaphragmatic lesion, and uncertain/associated findings suspected for a diaphragmatic involvement
Direct signs |
Discontinuity of diaphragmatic profile |
Segmental non-visualization of diaphragm |
Dangling sign |
Indirect signs |
Intrathoracic visceral herniation |
Collar sign |
Hump sign and band sign |
Dependent viscera sign |
Contiguous injury on either side of the diaphragm |
Elevated abdominal organs |
Signs of uncertain-controversial origin or associated signs |
Thickening of the diaphragm |
Hypoattenuated diaphragm |
Fractured rib |
Diaphragmatic/peridiaphragmatic contrast extravasation |
Table 12.2
Management of the TDI
Specific findings | ||
Fat/abdominal viscera thoracic herniation |  | Surgery |
Collar sign | ||
Dependent viscera sign | ||
Nonspecific findings | ||
Diaphragm thickening |  | X-ray/CT follow-up |
Discontinuity of the diaphragmatic profile | ||
Segmental non-visualization of diaphragm | ||
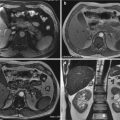
Discontinuity of the diaphragmatic profile. It is the most frequent and important sign of a TDI since it represents the direct evidence of the tear of the musculotendinous component, which can be located both centrally and peripherally (Fig. 12.7). This sign is observed in almost 96% of all traumatic diaphragmatic hernia, and it is considered to be very significant since its sensitivity has been reported to be 58–82.7% and its specificity 88–95%. The free edges of the ruptured diaphragm are usually thickened by post-traumatic edema, hemorrhage, or muscle retraction [10, 20].


Fig. 12.7
Coronal (a, c) and sagittal (b) MPR images show right diaphragmatic rupture characterized by a large interruption of the muscle profile with concomitant intrathoracic herniation of fat, part of the colon, and small bowel (arrows). Sagittal MPR view shows also the dangling sign: the free edge of the diaphragm at the level of the traumatic tear bends outwards the abdominal cavity (arrowhead)
Segmental non-visualization of diaphragm. It is an isolated absence of a part of the diaphragm in the site of the injury. This sign has a sensitivity of 86% and a specificity of 68% since it may be falsely positive in elderly patients, in whom the non-visualization of a section of diaphragm might be a normal variant, or when the outline of the diaphragm is blurred due to retroperitoneal hematoma, hemothorax, pulmonary contusion, or atelectasis of pulmonary bases [20].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree