Trauma
Main etiology
Mechanism
Main injuries
Blunt
Motor vehicle collision (MVC) fall from height
Direct impact
Direct-impact forces transmitted along the trajectory of the “force vector”
Extremity injuries, head and thoracoabdominal parietal and parenchymal injuries
Compression
Collision of the tissues with a fixed object
Thoracic injuries (flail chest, tracheobronchial tree injuries), abdominal parenchymal (spleen, liver injuries) and pelvic injuries
Acceleration/deceleration
Stretching of the organ at the fixed points of attachment
Vessel, mesenteric, tracheobronchial tree injuries
Combined compression and deceleration (airbag/seat belt injuries)
Sternal fractures, spinal trauma, bowel and mesenteric injuries
Penetrating
Stab wound
Tissue disruption
Direct injury to a focal area with tissue penetration
Depend on the involved anatomical region
Gunshot wound
Blast
Improvised explosive devices (IEDs)
Barotrauma
High-pressure blast wave followed by sudden drop in pressure
Lung contusions, mesenteric and bowel injuries
Penetrating trauma
Depend on the involved anatomical region
Combined blunt and penetrating
Bone fractures, as well as visceral injuries and closed head injuries
Thermal and inhalation injuries
Thermal and chemical exposure of the respiratory mucosa
Respiratory mucosa and lung injuries
A rapid overview of the situation to establish a tailored appropriate therapeutic strategy is mandatory, as survival rate after trauma is influenced by the preclinical and clinical trauma management within the first hour after an injury, known as “the golden hour” [2].
Notoriously clinical evaluation of patients who suffered high-energy trauma may be unreliable [3].
Physical examination of those patients is indeed often insidious as they may show multiple concomitant injuries, thereby diverting the responding “physician’s” attention, or because of an altered state of consciousness due to drug or alcohol intoxication.
In this context, as a member of the trauma team, the radiologist has the major role of promptly recognizing (or to exclude) critical injuries requiring immediate treatment and also identifying the mechanisms of injury that may suggest subtle associated lesions that could be easily overlooked (Fig. 2.1) [4]. Actually, MDCT has revolutionized the management of trauma patients, representing the most useful screening tool to quickly assess injuries [1, 2, 5].


Fig. 2.1
Contrast-enhanced MDCT shows a large traumatic pseudoaneurysm of the descending thoracic aorta (a, arrows) with typical location and morphology (a–c straight arrows) with a large mediastinal hematoma displacing and compressing the carina, in a patient after high-energy blunt trauma. Note also a sternal fracture (b, curved arrow)
Modern technologies allow fast evaluation of traumatic injuries with the maximum concentration of time, which has a great impact on the results in terms of resuscitation and safety [6, 7].
This chapter will discuss the most common mechanisms of injuries and related imaging findings, focusing on the importance for radiologists to look for anatomic sites at risk of lesion according to direction of forces with the aim to individuate expected but also unexpected injuries.
2.2 Mechanisms of Lesions
Forensic medicine distinguishes two main transfers of kinetic energy, blunt or penetrating traumas (Table 2.1) [1]. Blunt trauma is considered as an injury in which tissues are not penetrated by external objects; it occurs most frequently in the context of road traffic accidents and is classified according to whether the primary mechanism of injury is related to a compression or deceleration forces [8] (Fig. 2.1).
As this trauma is usually the result of motor vehicle crushes (MVCs), it is the most frequent cause in the western countries.
Conversely, penetrating injuries result from an object entering the body and sometimes exiting the body, causing damage along its path (Table 2.1) [1].
Commonly the object penetrates the fascia and injures underlying structures resulting in “open” injuries (Fig. 2.2).


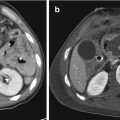
Fig. 2.2
Contrast-enhanced MDCT in sagittal (a), coronal (b), and axial (c, d) views showing the entry point of a penetrating trauma (a, straight arrow) involving the uncinate process of the pancreas (a, curved arrow; b, straight arrows) and the fifth liver segment (c, d, arrows) with hemoperitoneum (c, asterisk)
Penetrating trauma involves a disruption of the skin and underlying tissues in a small, focused area (Fig. 2.2).
The severity of a stab wound depends on the area involved, depth of penetration, blade length, and angle of penetration.
Firearms are the primary mechanism resulting in penetrating trauma.
One point to consider is that every penetrating event results in open injuries, but not all open injuries are caused by penetrating mechanisms. For example, an open fracture from motor vehicle collision (MVC) is by definition a blunt trauma in which bone fragments become secondarily exposed by an indirect mechanism, due to the high energy of the trauma (Fig. 2.3).


Fig. 2.3
Contrast-enhanced MDCT and MIP reconstruction in the axial plane (a) showing multiple displaced rib fractures in more than one-point “flail chest.” Pulmonary window in the axial plane (b) shows multiple lung contusions, hemothorax, pneumothorax, and subcutaneous emphysema. Multifragmentary fracture of the acetabulum (c) with displacement of the femoral head (c, d)
Nowadays a particular mechanism of trauma is injury resulting by the use of improvised explosive devices (IEDs) such as the ones encountered in terrorist attacks. As the terrorism represents a matter of big concern in modern countries, radiologists working in a trauma center have to be aware of “blast injury patterns”. Recent evidence emerged from the victims of Boston marathon bombing has underlined the role of imaging in the evaluation of foreign bodies and skeletal trauma in blast injuries [9].
2.3 Imaging
MDCT represents “the cornerstone” of the decision-making process in polytrauma patients, and the emergency radiologist is the leader of this process, who must be present in CT room 24/7 to provide a continuous coverage [2, 4]. Nowadays, modern CT scanners allow enhanced image resolution with a marked reduction of the time needed for scanning, thereby allowing examination of the whole body within a few minutes. Motion artifacts can be minimized with this shorter acquisition time. Moreover the location of CT scanner next to the emergency unit allows rapid examination even in patients with some degree of hemodynamic instability [4, 10]. Wurmb et al. demonstrated in their study that direct whole-body CT accelerated diagnostic interval from a median of 70 to 23 min and decision-making process interval from 82 to 47 min [4, 11].
As mentioned above, clinical examination is often unreliable, as patients may be unconsciousness due to the trauma or due to altered mental status; thus hollow visceral or vessel injuries may be easily overlooked in the presence, for example, of multiple bone fractures, differing time to treatment with life and cost consumption.
2.4 Blunt Trauma
As previously mentioned blunt trauma represents the most frequent mechanism of injury in modern countries [1]. It recognizes two major situations: motor vehicle collisions (MVCs) and falls.
2.5 MVC
Motor vehicle collisions are the leading cause of trauma death in all age groups from 1 to 65 years [1].
The injuries produced from MVC strongly depend from the energy of the impact, the direction of the forces, and also the presence of restraint devices. Frontal collision determines a moving forward of the occupant, if unrestrained, as long as the patient impacts the stationary vehicle chassis. Often the first site of the impact is represented by the extremities, resulting in arm and leg fractures; then injuries may occur to the head and spine, also because of torsional forces. Conversely in lateral collisions, the victim is moved away from the side of the vehicle; it determines more often compressive pelvic and thoracoabdominal injuries. With the wide use of restraint devices (i.e., airbags, seat belts), there has been in last years a drastic reduction of both morbidity and mortality from crashes but a corresponding increase in the number of injuries attributable to these devices [12].
Airbags are responsible of injuries to upper extremities, the face, and the neck; corneal abrasions; and cervical hyperflexion injuries if the victim is seated too close to the restraint.
Seat belt injuries may vary from simple chest and/or abdominal abrasion at the site of seat belt contact to sternal fractures, spinal trauma (Fig. 2.4), and injuries to the bowel and mesentery (Figs. 2.5 and 2.6) [13].




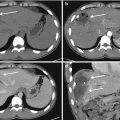
Fig. 2.4
Contrast-enhanced CT in the arterial phase in axial (a, b) and sagittal planes (c) after a seat belt injury. Note a spot of active bleeding (a, b arrows) within the anterior abdominal wall and a fracture of the fifth lumbar vertebra (c, arrow) along the same force vector

Fig. 2.5
Contrast-enhanced MDCT in arterial phase in axial (a, c), coronal (b), and oblique views (d) after a seat belt injury. Note the lumbar transverse process fracture (a, arrow) and a pooling of active bleeding in the mesentery (c, d arrows)

Fig. 2.6
Multiphasic contrast-enhanced MDCT in a seat belt injury shows increasing amount of active mesenteric bleeding in the arterial (a), venous (b), and late phases (c)
It is a well-known issue that motorcyclists are at substantially higher risk of dying from crashes than car occupants.
Globally, motorcyclists account for nearly a quarter of all road traffic deaths (WHO 2015). In 2014, in the United States, motorcyclists accounted for less than 1% of person per miles traveled but more than 13% of the total mortality from motor vehicle crashes [14]. Most of the injuries are to the head, so these are often critical injuries, as in the final ground impact deceleration/acceleration mechanisms are strongly involved.
2.6 Falls
Falls represent one of the most common mechanisms of trauma across all age groups, varying from simple ground-level falls to falls from significant height, the latter resulting in severe injuries [1].
Simple ground-level falls often do not require any diagnostic imaging, but may be dangerous in the elderly, as the bones are more fragile, and bone injuries, as lumbar, femoral, and radial fractures, as well as subdural hematomas are quite common. Injuries from falls from significant heights may be intentional or not (work-related accidents); almost all these patients show multiple lesions, and the musculoskeletal system is often involved [1, 15]. Falls from a height result in an axial load, and injury patterns depend on several factors: the height of the fall, the landing position of the victim, the surface of the impact, as well as age and comorbidities of the patient. For example, landing on the feet can result in calcaneus and long bone fractures (Figs. 2.7 and 2.8), with secondary involvement of the lumbar and thoracic spine as the kinetic energy travels up the body [1].



Fig. 2.7
Plain film views (a, b) and CT volume rendering (c) of bilateral calcaneal fractures (a, b, arrow) due to a fall from height

Fig. 2.8
Plain film views (a, b), CT in sagittal plane (c), and volume rendering CT (d) of a proximal tibia (a, arrow) and astragalo-calcaneal fractures (b, c, arrows and d) due to a fall from height
The American College of Surgeons recommend that patients injured in falls from heights greater than 20 ft need to be taken to a trauma center, as the height is a factor exponentially related to the energy produced, resulting in life-threatening injuries [15].
2.7 Mechanisms of Blunt Trauma
Blunt trauma resulting injuries essentially depends from changes in pressure and shear forces produced by three main mechanisms [16–19]: (a) direct-impact, (b) compression, and (c) rapid acceleration/deceleration injuries (Table 2.1) [2].
2.7.1 Direct Impact
Direct-impact injuries are generally considered less dangerous, resulting, more often, in minor injuries, such as rubbings, ecchymosis, and/or hematomas that sometimes do not even require any imaging evaluation. In some cases, however, direct-impact injuries resulting from a motor vehicle accident, fall, or a direct blow from a moving object can lead to localized wall injuries, such as fractures of the skull, ribs, and sternum and sternoclavicular joint dislocation. Depending on the high kinetic energy, direct-impact forces may be transmitted through the body to the deeper tissues and organs, such as the brain, lungs, heart, liver, and spleen along the trajectory of the “force vector.” In these cases, for example, a direct blow to the chest wall may cause significant vascular injuries requiring immediate treatment, even in the absence of skeleton fractures. Therefore, according to the energy delivered by the injury, a direct impact may evolve into a compression mechanism, as internal organs may be secondarily involved by compression/shearing forces. An example of direct injury is extra-axial brain hematoma (epidural, subdural, and subarachnoid/intraventricular) and intra-axial injury (cortical contusion, intracerebral hematoma) (Figs. 2.9 and 2.10). In blunt brain injuries, cortical contusion may occur when the brain is pushed against the irregular inner surfaces of the skull at the time of impact at the coup site or, more commonly, at the opposite site. This last is produced by the impact of the moving brain to a fixed point, and it is more dangerous when the blow occurs to the occiput, due to the irregular surfaces of the anterior and central skull base, with characteristic hemorrhagic contusions seen in the inferior frontal and temporal lobes (Fig. 2.9) [20]. In the acute setting, a direct trauma to the skull, especially in elderly patients, requires a non-contrast CT scan, which represents the modality of choice, as it promptly allows depiction of intracranial traumatic lesions.



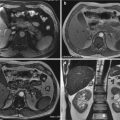
Fig. 2.9
MDCT scan in a patient underwent a direct trauma to the skull. Note the occipital fracture (a) in the site of the direct impact and the typical hemorrhagic contusions in the opposite site (frontal lobe) (b)

Fig. 2.10




MDCT scan in axial planes (a–c) and volume rendering (d) in a patient underwent a direct head trauma. There is a subgaleal (a, arrow) and epidural hematomas (b, straight arrow) in the site of impact and brain contusion on the opposite site (b, curved arrow). Note also a subarachnoid hemorrhage on the left side (c). Finally, volume rendering image demonstrates the parietal fracture (d, arrow)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree