14 Treatment of Adhesive Capsulitis
♦ Background and Indications
• Approximately 40% of individuals diagnosed with adhesive capsulitis may experience prolonged immobility despite noninvasive treatment, such as physical therapy and nonsteroidal anti-inflammatory drugs. Approximately 15% of such individuals ultimately develop disability.1
• Studies on ultrasound-guided injection techniques, such as glenohumeral joint (GH) injection with intra-articular steroid, suprascapular nerve blocks (SSNB), and the glenohumeral brisement procedure for the management of adhesive capsulitis, have yielded mixed results.2
• A protocol involving a combination of previously studied treatments (SSNB, intraarticular steroid injection, brisement volume dilation, immediate manipulation of the shoulder, and a subsequent 8 weeks of physical therapy) was shown to improve shoulder range of motion (flexion and abduction) immediately after intervention and at 2 months’ follow-up.2
1 Binder AI, Bulgen DY, Hazleman BL, Roberts S. Frozen shoulder: a long-term prospective study. Ann Rheum Dis 1984;43(3):361-364 and Burbank KS. Chronic shoulder pain: part 1. Evaluation and diagnosis. Am Fam Phys 2008;15(77):453-460.
2 Mitra R, Harris A, Umphrey C, Smuck M, Fredericson M. Adhesive capsulitis: a new management protocol to improve passive range of motion. PM R 2009;1(12):1064-1068.
Suprascapular Nerve Block
♦ Setup
• The patient should be seated with the hand on the contralateral shoulder or be lying prone with the arm hanging down (Fig. 14.1).
• A high-frequency linear array transducer should be used with the depth set to 3 to 5 cm.
• A 22-gauge, 2.5- to 3.5-inch needle should be used, depending on body habitus.
♦ Landmarks
Two landmarks should be noted:
• Spine of the scapula
• Supraspinatus
♦ Probe Positioning
• The probe should be positioned over the supraspinatus muscle (Fig. 14.2).
• The probe should be parallel to the spine of the scapula (scapular plane).

Fig. 14.1 The patient is seated with the hand on the contralateral shoulder.

Fig. 14.2 The spine of the scapula is palpated, and the probe is placed over the supraspinatus, parallel and superior to the spine of the scapula.
♦ Normal Anatomy
• The suprascapular nerve (SSN) is formed from the upper trunk of the brachial plexus (C5-C6 nerve roots) (Fig. 14.3).
• The SSN courses under the transverse scapular ligament in the suprascapular notch then under the supraspinatus and through the spinoglenoid notch.
• Branches of the SSN include the superior articular branch, which innervates the coracohumeral ligament, subacromial bursa, and posterior acromioclavicular joint; the inferior articular branch, which innervates the posterior joint capsule; and branches to the supraspinatus and infraspinatus.

Fig. 14.3 Course of the suprascapular nerve through the suprascapular and spinoglenoid notches.
♦ Pathologic Anatomy
• Except in cases of space-occupying lesions, pathology is rarely seen in ultrasoundguided SSNB.
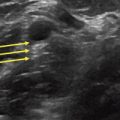
• The SSN is visualized as a round, hyperechoic structure located close to the cortical line of the supraspinatus fossa, close to the suprascapular notch and deep to the superior transverse scapular ligament (STSL) (Fig. 14.4).
• In the area of the suprascapular notch, power Doppler can be used to identify the suprascapular artery above the STSL, with the nerve located below the STSL.
♦ Image-Guided Injection
• Injection is performed using the long-axis (longitudinal) view in the scapular plane.
• The needle should be oriented in the plane with the transducer using a medial to lateral approach.
• The operator should aim for the SSN at the level of the suprascapular notch or fossa.
• A heel-toe maneuver should be used for better needle visualization.
• The suprascapular artery must be avoided.

Fig. 14.4 Using the long axis, the needle is inserted (blue line) in line with probe with a medial to lateral approach. The suprascapular nerve (SSN, indicated by the yellow arrow) is visualized under the superior transverse scapular ligament (at the tip of needle path [head of the blue arrow]). CP, Coracoid process; SS, supraspinatus; SS notch, suprascapular notch; Tr, trapezius.
Glenohumeral Brisement Procedure
♦ Setup
• Setup is identical to that for the glenohumeral intra-articular steroid injection.
• The patient should be placed in the lateral recumbent position with the affected side up (Fig. 14.5).
• The glenohumeral joint (GHJ) is best visualized in the long axis using a low-frequency curvilinear array transducer.
• A 22-gauge to 25-gauge, 2- to 3.5-inch needle should be used, depending on body habitus.
♦ Landmarks
Two landmarks should be noted:
• Scapular spine
• Infraspinatus