Case presentation
A 15-year-old male presents with left scrotal pain and swelling for the past 5 hours. He states that he was jumping on a trampoline just prior to presentation and afterward, he experienced his symptoms. He denies genital trauma. He has not had fever, back pain, dysuria, hematuria, penile discharge, abdominal pain, or vomiting. He denies being sexually active.
Physical examination reveals a well-appearing pleasant adolescent in some discomfort. He is afebrile but he is mildly tachycardic with a heart rate of 110 beats per minute; his respiratory rate is 16 breaths per minute; his blood pressure is 125/65 mm Hg. He has a nontender abdominal examination without rebound, guarding, or masses. His genital examination demonstrates a Tanner IV male, without obvious erythema or masses. There are no signs of trauma. He has tenderness to the left epididymis and to the left scrotum in general. The testicles feel normal but he has pain with examination of the left side and the left testicle appears to lie slightly higher than the right. There is mild left scrotal swelling. He is circumcised. There is no discharge from the penis. There are no lesions.
Imaging considerations
Plain radiography
While plain radiography of the abdomen may be utilized in cases of abdominal pain, it is not indicated as a first-line imaging study in patients who have suspected testicular pathology.
Ultrasound (US)
Readily available and without ionizing radiation exposure, US is an excellent means by which to visualize the scrotum and its contents. It is the imaging modality of choice across all age groups when ruling out testicular torsion, particularly duplex examination including color and spectral Doppler sonography, with sensitivity and specificity both approaching 100%. US can also detect other entities that may mimic symptoms of testicular torsion, including epididymo-orchitis, hydroceles, varicoceles, and testicular masses.
A high-frequency transducer is used to scan the testicle in its entirety in both the transverse and longitudinal planes. Gray-scale and color Doppler images should be obtained. Both venous and arterial flow may be compromised. A lack of normal arterial blood flow is suspicious for testicular torsion; however, the phenomenon can be partial or intermittent, and the presence of normal or decreased Doppler arterial flow cannot completely rule it out. A sonographic finding that is definitive for testicular torsion is the “whirlpool sign,” in which there is an abrupt change in the course of the spermatic cord with a spiral twist at the external inguinal ring or in the scrotal sac. A “torsion knot” may also be seen by US, in which redundant, tortuous spermatic cord twists, often around a small, reactive hydrocele. Normally, the testes have a vertical lie. A horizontal lie, or bell clapper deformity, can occur from abnormal attachment of the tunica vaginalis and is associated with intermittent testicular torsion. A US demonstrating horizontal or oblique lie, especially in the setting of diminished or absent intratesticular flow, is concerning for testicular torsion.
US is the diagnostic imaging modality of choice for all patients when testicular torsion is suspected, but the presence of vascular flow by Doppler alone cannot be exclusively relied upon to exclude this condition in patients whose symptoms and examination are consistent with testicular torsion. The clinician should also consider the history, clinical examination, and other US findings when interpreting sonography results, and if overall suspicion is high, emergent urological consultation is warranted.
Computed tomography (CT)
CT scan is generally not indicated in the work-up of testicular torsion. However, there is literature suggesting that perfusion CT scanning may be considered as a secondary method of diagnosing testicular torsion in indeterminate cases. It should not be utilized as a first-line imaging modality due to radiation exposure.
Magnetic resonance imaging (MRI)
While also not a first-line imaging modality for patients with testicular pain, MRI is considered to be highly sensitive for testicular torsion. Specifically, the dynamic contrast-enhanced (DCE)–subtraction technique can demonstrate changes in testicular perfusion by assessing testicular contrast enhancement. MRI, however, is not a practical choice to diagnose testicular torsion given its limited availability, length of study, and cost.
Scrotal scintigraphy
Scrotal scintigraphy is a nuclear study in which a radioisotope is used to demonstrate testicular blood flow. Although it used to be widely utilized starting in 1971, it has been replaced by ultrasonography, which is readily available and does not require exposure to ionizing radiation. Scintigraphy may still play a role when testicular torsion has not been ruled out and US is inconclusive.
Near-infrared spectroscopy (NIRS)
NIRS has been proposed as a potentially useful modality in ruling out testicular torsion because it is noninvasive, portable, easily accessible for bedside use, and easy to interpret. It uses light transmission and absorption to measure tissue oxygen saturation in superficial body layers up to several centimeters deep. In testicular torsion, the affected testicle is predicted to have significantly lower tissue oxygen saturation than the unaffected contralateral testicle. Although promising in theory, there is not enough evidence to support routine use of NIRS in the work-up of testicular torsion. ,
Imaging findings
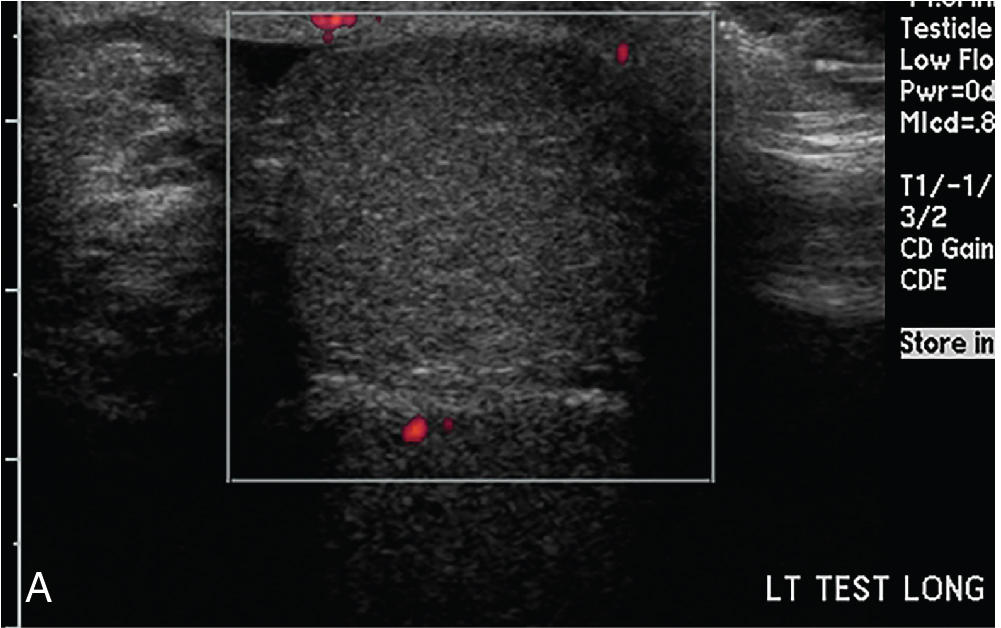
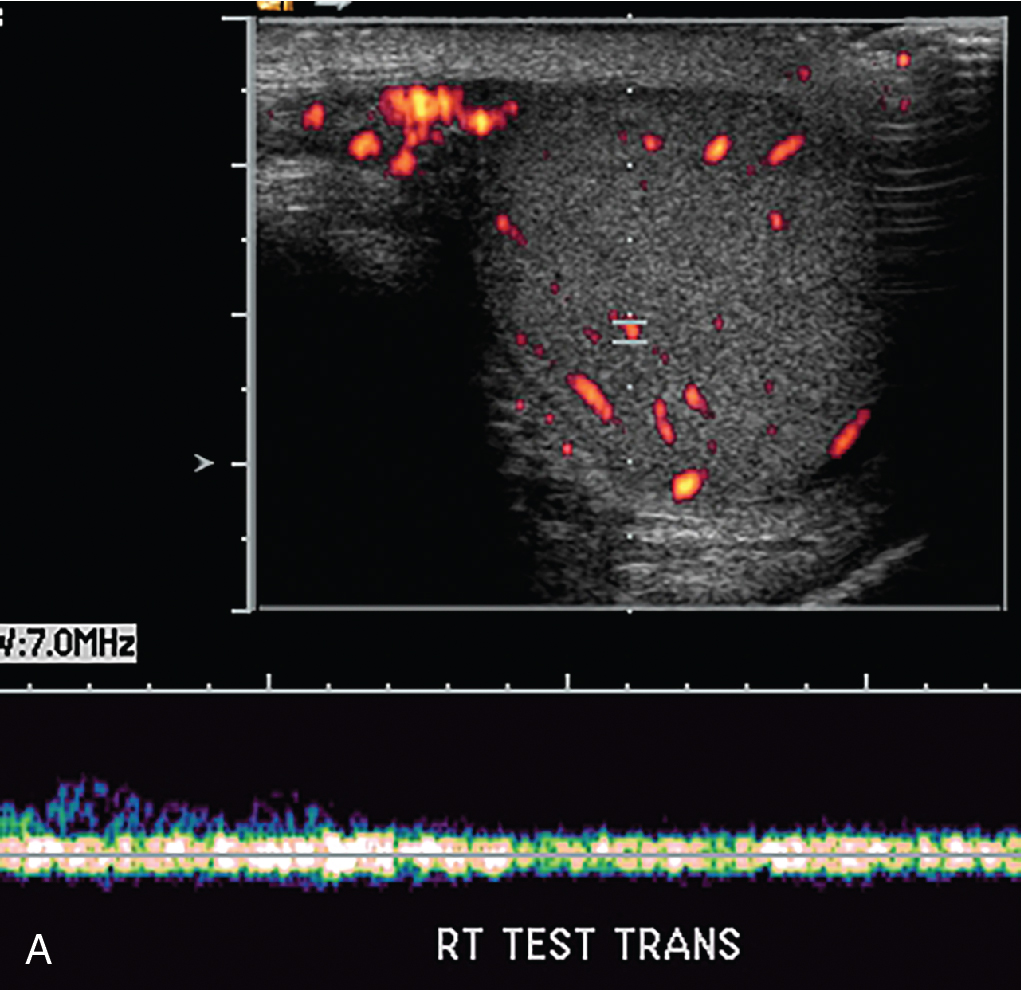
The patient had grayscale and color and spectral Doppler ultrasonography performed. Selected images from that study are noted here. While the right epididymis and testis are normal in appearance and have normal color and spectral arterial flow, the left testis is heterogeneous and slightly hyperechoic. There is no demonstrable Doppler flow to this testis. These findings are highly suggestive of left testicular torsion ( Figs. 21.1–21.3 ).