Ultrasound-Guided Interventions
Ronald S. Adler
INTRODUCTION
The real-time nature of ultrasound makes it ideally suited to providing guidance for a variety of musculoskeletal interventions.1,2,3,4,5,6,7,8,9 Continuous observation of the needle ensures accurate needle placement and appropriate distribution of the injected and/or aspirated material. Needles can be positioned close to neurovascular bundles without damaging nerves or vessels. The potential deleterious effects of not attaining proper needle placement during corticosteroid administration are well documented10,11,12,13,14,15,16,17 and are discussed later.
The current generation of high-frequency small parts transducers allows excellent depiction of soft tissue details and articular surfaces, particularly in the hand, wrist, foot, and ankle,18 facilitating exact needle insertion into non-distended structures, such as joints, tendon sheaths, or bursae. Injected fluid produces a contrast effect, which improves delineation of adjacent structures (e.g., labral morphology) and shows the distribution of the injected material.19,20 The advent of newer technology that permits image registration to other modalities, such as computed tomography or magnetic resonance imaging (MRI), is expected to enhance further the role of ultrasound in performing a broad variety of interventions.21 Ultrasound guidance to target sites of maximal tendon and/or muscle pathology has been used to administer growth factors using platelet-rich plasma (PRP) or autologous blood.22,23,24,25,26 A brief discussion of these newer applications will be included. Ultrasound guidance does not involve ionizing radiation, and this is an advantage in the pediatric population and during pregnancy.
Following a discussion of sonographic technique, ultrasound-guided interventions in the musculoskeletal system will be reviewed with particular attention to injections of joints, tendon sheaths, bursae, and ganglion cysts, with an emphasis on the most commonly requested procedures. Newer applications will also be discussed, such as perineural injections/ablations and intratendinous therapy. Finally, the utility of ultrasound guidance in performing soft tissue biopsies will be discussed.
ULTRASOUND-GUIDED THERAPEUTIC INJECTIONS/ASPIRATIONS
The most common clinical indication for ultrasound-guided injections generally relates to pain that has failed to respond to conservative measures, regardless of the anatomic site. The pain may be the result of a chronic repetitive injury in the work environment, a sports-related injury, or injury from an underlying inflammatory disorder, such as rheumatoid arthritis. This chapter presents illustrative examples of the most relevant studies, without dwelling on the specific clinical entities.
TECHNICAL CONSIDERATIONS
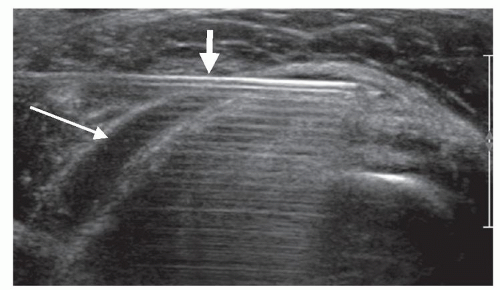
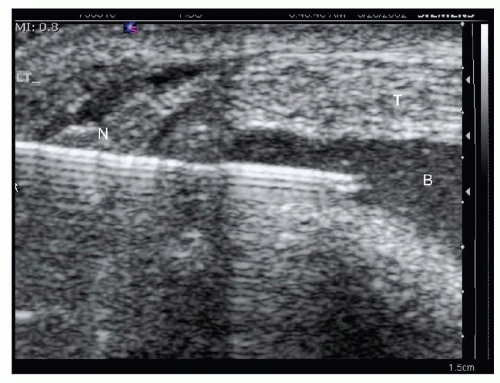
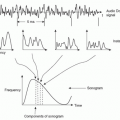
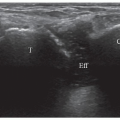
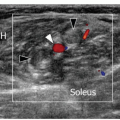
Diagnostic examinations and subsequent therapeutic interventions are often performed using either linear or curved phased array transducers, depending on depth and local geometry. Needle selection is based on specific anatomic conditions (i.e., depth and size of the region of interest). I employ a freehand technique in which the basic principle is to ensure that the needle is visualized as a specular reflector.7,8 This relies on orienting the needle to be perpendicular (or nearly so) to the insonating beam (Fig. 14.1). The needle then becomes a specular reflector, often having a strong ringdown artifact. Needle guides are available and may be of value, but I have found that a freehand technique allows greater flexibility in adjusting needle position. Needle visualization can be enhanced by injecting a small amount of anesthetic and observing the consequent moving echoes in either grayscale or color flow imaging.1
Patient positioning to ensure comfort and optimal visualization of the anatomy should first be assessed. Tendons are anisotropic27; therefore, the transducer should be oriented to maximize tendon echogenicity to avoid misinterpretation as tendinopathy, complex fluid, or synovium. An offset may be required at the skin entry point of the needle relative to the transducer
to provide appropriate needle orientation. Deep structures such as deep flexor tendons of the hip are often better imaged using a curved or sector transducer, operating at center frequencies of approximately 3.5 to 7.5 MHz. Superficial, linearly oriented structures, such as tendons in the wrist or ankle, are best approached using a linear array transducer with higher center frequencies (>10 MHz). Transducers with a small footprint (“hockey stick”) are particularly well suited to superficial injections. These factors should be assessed prior to skin preparation.
to provide appropriate needle orientation. Deep structures such as deep flexor tendons of the hip are often better imaged using a curved or sector transducer, operating at center frequencies of approximately 3.5 to 7.5 MHz. Superficial, linearly oriented structures, such as tendons in the wrist or ankle, are best approached using a linear array transducer with higher center frequencies (>10 MHz). Transducers with a small footprint (“hockey stick”) are particularly well suited to superficial injections. These factors should be assessed prior to skin preparation.
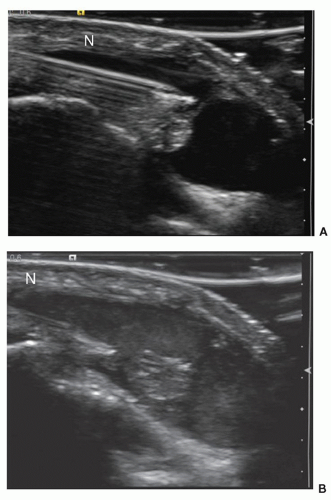
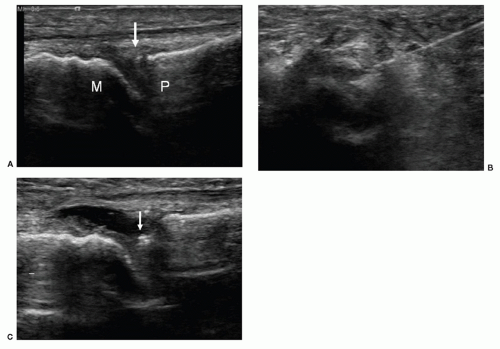
The immiscible nature of the steroid-anesthetic mixture may produce temporary contrast effect (Fig. 14.2). In vitro experiments suggest that this property is due to alterations in acoustic impedance by the scattering material formed by the suspension of steroid in an aqueous background, resulting in an approximate increase in echo intensity of 20 dB.20 This increases the conspicuity of the delivered agent during real time and helps to define the distribution of the delivered agent during the injection.
Tip:
Choose transducer geometry and entry site to visualize the needle as a specular reflector.
Orient transducer to maximize tendon echogenicity (anisotropy).
Injected corticosteroid/anesthetic suspension often displays a contrast effect, which can help localize injected mixture.
INJECTION TECHNIQUE
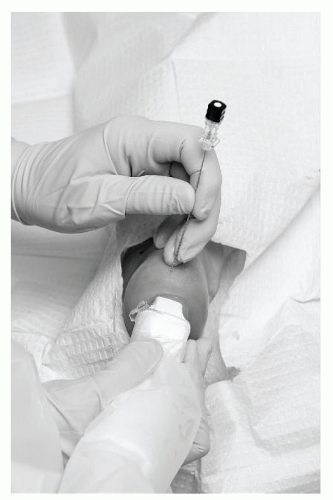
Sterile technique is essential. The skin is cleaned with an iodine or alcohol-based solution and may be covered with a sterile drape (Fig. 14.3). The transducer is immersed in iodine-based solution and surrounded by a sterile drape or placed into a sterile probe cover. A drape can also be placed over portions of the ultrasound unit, although many radiologists keep drapes to a minimum or avoid them completely. One percent lidocaine is used for local anesthesia. Once the needle is in position, the procedure is undertaken while imaging in real time. Depending on anatomic location and personal preference, a 1.5″ blue (25G), brown (22G), or green (21G) needle, or a 22G spinal needle with a stylet is used to administer the anesthetic/corticosteroid mixture, generally consisting of long-acting anesthetic and one of the standard injectable corticosteroid derivatives. Several steroid solutions with different properties regarding duration in the soft tissues and potential untoward effects are available (see below).
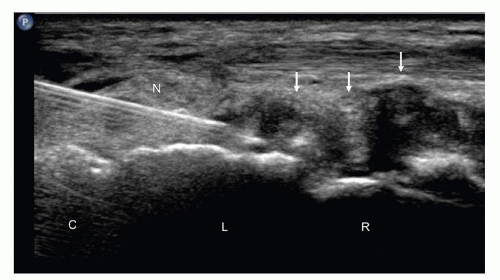
It is convenient to distinguish two separate approaches to performing injections, long axis and short axis, which relate to needle orientation relative to the structure to be injected. The long-axis approach refers to needle placement in the plane parallel to the structure of interest (Fig. 14.4). Examples include longitudinal imaging of the hip to display a hip effusion and employing this as the plane in which to direct the needle for ultrasound-guided aspiration. The short-axis approach refers to needle entry in the plane perpendicular to the long axis of a structure (Fig. 14.5). Examples include injecting the retrocalcaneal bursa using a lateral approach. The short-axis approach works well when performing injections/aspirations in small joints and tendon sheaths of the hand and foot. The long-axis approach appears better suited to deep joint injections, such as the hip or shoulder. It is important to recognize, however, that such approaches serve merely as guidelines and that there is no unique method that necessarily applies to any specific injection.
INJECTION MATERIALS
Most injections use long-acting corticosteroid in combination with local anesthetic in relatively small volumes. A detailed review of these agents is beyond the scope of the current chapter. Injectable steroids usually come in crystalline form, associated with a slower rate of absorption, or a soluble form, characterized by rapid absorption.27,28,29,30 Examples of the former are triamcinolone and methylprednisolone, whereas commonly used examples of the latter are betamethasone and dexamethasone. Because of their rapid resorption, soluble preparations may be preferable in superficial structures where subcutaneous fat atrophy and/or skin depigmentation are potential complications. In the case of the crystalline agents, a reactive inflammatory response or flushing response may occur, and patients should be warned that they may experience severe pain in the 2 to 3 days following the injection. The soluble forms are not typically associated with these complications, but crystalline forms are usually preferred because they are long-acting. A painful steroid “flare” is less likely with
triamcinolone than methylprednisolone, but skin depigmentation and fat atrophy are more likely with triamcinolone. Patients with diabetes should be cautioned that they may develop transient hyperglycemia that can last for 5 to 10 days.
triamcinolone than methylprednisolone, but skin depigmentation and fat atrophy are more likely with triamcinolone. Patients with diabetes should be cautioned that they may develop transient hyperglycemia that can last for 5 to 10 days.
The most significant complications associated with injectable steroid use in the musculoskeletal system relate to chondrolysis (when used in weight-bearing joints), skin depigmentation, fat necrosis, and impaired healing response (when used in soft tissues). The latter has been associated with tendon, ligament, and plantar fascia rupture.10,11,12,13,14,15,16,17 As the most commonly used mixtures contain insoluble particles, a systemic injection could theoretically result in an embolic phenomenon, and this has been implicated as a mechanism for neurological complications associated with transforaminal injections.31 I have not encountered this as a complication when performing injections in the appendicular skeletal system.
The most commonly used anesthetics are lidocaine and bupivacaine (i.e., Marcaine).17,31,32 They are both local injectable anesthetics, but differ in the onset and duration of action. Lidocaine has rapid onset (seconds) and short duration (1 to 2 hours). Bupivacaine becomes effective in 5 to 10 minutes and generally lasts 4 to 6 hours. Potential adverse reactions include neurotoxicity, cardiotoxicity, and allergic reactions,30 but are rare when used in small doses under image guidance and avoiding intravascular injection. Recent studies also report that bupivacaine is associated with chondrolysis when used for intra-articular applications. This effect has only been seen during constant infusions at arthroscopy and in vitro. Chondrolysis is not likely to be an issue when used in the small volumes typically employed during injections in the musculoskeletal system, although 0.5% ropivacaine would provide a potentially safer alternative.
Tip:
Patients should be warned that they may experience severe pain in the 2 to 3 days following the injection (flare response) with crystalline-based corticosteroid.
Patients with diabetes should be cautioned that they may develop a transient hyperglycemia that lasts 5 to 10 days following steroid injection.
INJECTION OF JOINTS
Injection techniques are also discussed in the appropriate anatomical chapters.
Small Joint Injections
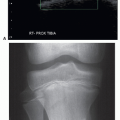
A high-frequency linear transducer is used for hand, wrist, elbow, foot, and ankle injections.5,6,33 A short-axis approach is often technically easier for small joints. The needle should enter the skin parallel to the plane of the joint space. Superficial joints usually appear as separations between the normally continuous specular echoes produced by cortical surfaces. As is true in other fluidcontaining structures, the presence of an effusion is a helpful feature in visualizing the needle as it enters the joint.
The short-axis approach entails scanning across the joint and looking for the transition from one cortical surface to the next, marking the skin (with a surgical marker), then placing a needle into the joint using ultrasound guidance. When imaging the joint in long axis, using this approach, the needle is seen in cross section (Fig. 14.6). If the needle does not appear within the joint, it may be necessary to “walk” the needle tip into the joint. It is important to recognize that the skin entry site acts as a fulcrum. Moving the needle hub proximally results in the tip moving caudally. Ideally, adjustments should require only minimal needle excursions. Needle position is confirmed by injecting a small amount of local anesthetic that should run away from the needle tip and distend the joint with fluid and echoes. If fluid pools around the needle tip, it is unlikely to be intra-articular. Small joints generally accommodate 0.5 to 1 mL; therefore it is important not to inject too much local anesthetic before the therapeutic mixture. It is convenient to employ a mixture of 1 mL (40 mg) of triamcinolone or methylprednisolone with 1 mL of long-acting anesthetic. Alternatively, the two are injected separately with a small volume of local anesthetic first to show that the needle is intra-articular, then the steroid. In this way the amount of injected corticosteroid is controlled. For small joints, 10 to 15 mg (0.5 to 0.75 mL) is usually adequate. For medium-sized joints (e.g., radiocapitellar joint), a larger volume (1 to 2 mL) of this mixture is often beneficial. When betamethasone or dexamethasone is used, one should be cognizant of dose equivalents. Betamethasone usually is distributed in multidose vials with concentrations of 6 mg/mL. Two milliliters of betamethasone has similar efficacy to 1 mL of triamcinolone or methylprednisolone. Dexamethasone is distributed in 1 mL vials (4 mg/mL), equivalent to 40 mg of either triamcinolone or methylprednisolone.
The short-axis approach works well in the metatarsophalangeal (MTP)/metacarpophalangeal and interphalangeal joints, midfoot, ankle, and elbow. Occasionally, a long-axis approach may be efficacious, as in the radiocarpal joint, lateral gutter of the ankle (Fig. 14.7), and dorsal midfoot when it is possible to insert the needle tip just deep to the joint capsule without having to incline the needle steeply. Ultrasound guidance helps to negotiate osteophytes and joint bodies. It allows identification of capsular outpouching, thereby affording a more convenient indirect approach into a joint than slipping a needle into a small joint space.
Large Joint Injections
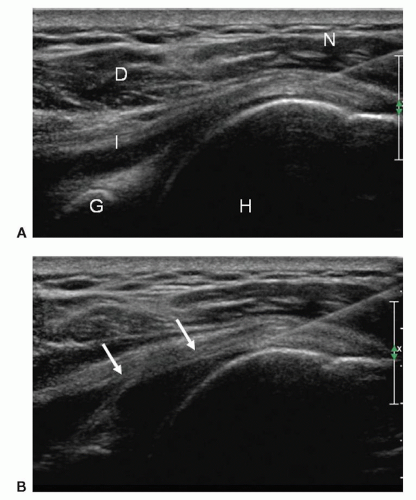
Shoulder
A long-axis approach and a 22G spinal needle are used when performing injections of large joints such as the shoulder or hip (Fig. 14.8).34,35 A greater volume is usually injected, typically 5 mL of the steroid/anesthetic mixture. In most cases the injectate contains 1 to 2 mL (40 to 80 mg) of triamcinolone or methylprednisolone. In the case of adhesive capsulitis, significantly larger volumes of local anesthetic (5 to 10 mL) may be added to provide additional joint distension (hydrodistention), which may promote lysis of focal adhesions. A posterior approach to the glenohumeral joint with the patient in a decubitus position, the shoulder to be injected upward, and the arm placed in cross adduction is generally used. An intermediate frequency linear or curved transducer suffices in the majority of cases. A linear transducer often results in better anatomic detail than curved arrays. The posterior recess of the glenohumeral joint is usually well seen with the patient in the decubitus position. The hypoechoic articular cartilage overlying the humeral head, echogenic posterior labrum, thin echogenic posterior capsule, and overlying infraspinatus muscle belly are identified. I use a long-axis approach with the needle directed from superolateral toward the joint and deep to the echogenic joint capsule. Others prefer the opposite direction. A test injection with 1% lidocaine shows bright echoes filling the posterior recess or distributed along
the articular cartilage if the needle is intra-articular. Pooling of fluid at the needle tip indicates an extra-articular injection, and the needle should be repositioned.
the articular cartilage if the needle is intra-articular. Pooling of fluid at the needle tip indicates an extra-articular injection, and the needle should be repositioned.
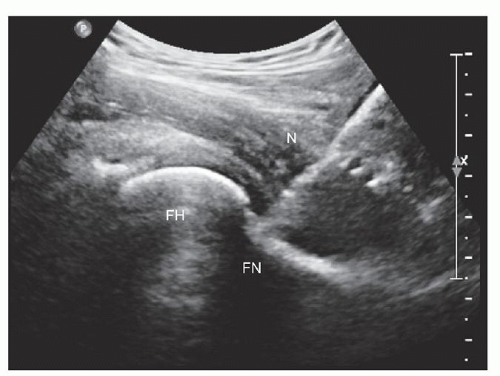
Hip
The hip is also approached in long axis with the transducer placed over the proximal anterior thigh at the level of the joint (Fig. 14.4), similar to the approach looking for an effusion. Ideally, the anterior capsule is imaged at the head-neck junction of the femur. In this approach, the scan plane is lateral to the neurovascular bundle. The needle is directed into the joint while maintaining its position in the scan plane of the transducer. A test injection of 1% lidocaine confirms the intra-articular needle position, and the therapeutic injection follows, using a similar mixture to the shoulder.
Fibrous Joints
Fibrous joints, such as the acromioclavicular joint, can be injected using ultrasound guidance (Fig. 14.9).34 A short-axis technique is employed similar to that in the foot. The transducer is placed sagittally on the clavicle and then moved laterally until the echogenic clavicle is replaced by the hypoechoic disc of the joint. The majority of fibrous joint injections are performed using a 1.5″ hypodermic needle. The joint has a small capacity and will accept only 0.5 to 1 mL of fluid. The volume of the test injection should therefore be minimal otherwise it may not be possible to inject the full therapeutic dose of 10 to 20 mg corticosteroid. This approach is also useful in the sternoclavicular joint and pubic symphysis.
Tip:
Most small joints of the hand and foot can be injected using a short-axis approach with 10 to 15 mg long-acting corticosteroid.
Shoulder and hip joints can be injected using a long-axis approach with 40 to 80 mg of long-acting corticosteroid.
Hydrodistention in combination with corticosteroid may be of value in adhesive capsulitis.
Superficial Peritendinous/Periarticular Injections
Peritendinous injections of anesthetic and long-acting corticosteroid are effective in tenosynovitis in the hand, foot, and ankle. The tendons are superficial and well-imaged on ultrasound. Ultrasound guidance is effective in ensuring that the injection is correctly placed. Bursae and ganglia can also be injected.
Foot and Ankle
The most commonly requested peritendinous injections in the foot and ankle are for chronic achillodynia or medial or lateral ankle pain due to posterior tibial or peroneal tendinosis/tenosynovitis, respectively.33 Less commonly, patients are referred to differentiate the pain of posterior impingement from stenosing tenosynovitis of the flexor hallucis longus (FHL) tendon, which may be difficult to distinguish clinically. Patients with plantar foot pain due to plantar fasciitis or forefoot pain from Morton neuroma are also frequently referred for ultrasound-guided injections.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree