16 Ultrasound of hemodialysis access
INTRODUCTION
Ultrasound has an important role in planning temporary and permanent hemodialysis access, for examining permanent access fistulas and grafts prior to first use, and in the investigation of complications in these fistulas and grafts. Ultrasound may be used for routine monitoring of access flow, although other methods are also available.
HEMODIALYSIS ACCESS
Chronic renal failure
Once chronic end-stage renal failure is identified, measurement of the patient’s creatinine levels and estimated glomerular filtration rate (eGFR) are used to determine the impending need for dialysis. Ideally, as the prospect of dialysis approaches, permanent access is planned and surgery undertaken so that the access is ready in time for first use.
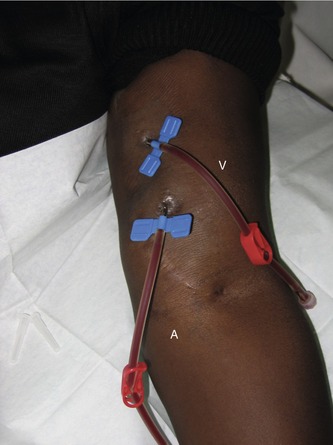
Permanent access, through a fistula or graft, requires high flows through a superficial vein or graft that can be repeatedly needled (Fig. 16.1), is easy to keep clean, and is comfortable for the patient during periods of dialysis – typically 4 hours three times a week. American and European reviews and guidelines have been produced and are regularly updated to foster good hemodialysis practice (National Kidney Foundation 2006; Tordoir et al. 2007). Both contain comprehensive bibliographies. Amongst challenges for the clinical teams that may involve ultrasound investigation are the need to increase the number of patients with a permanent access in place when they first present for dialysis, identifying the most appropriate access site for patients, and maintaining effective surveillance to reduce the incidence of complications and access failure.
Access sites
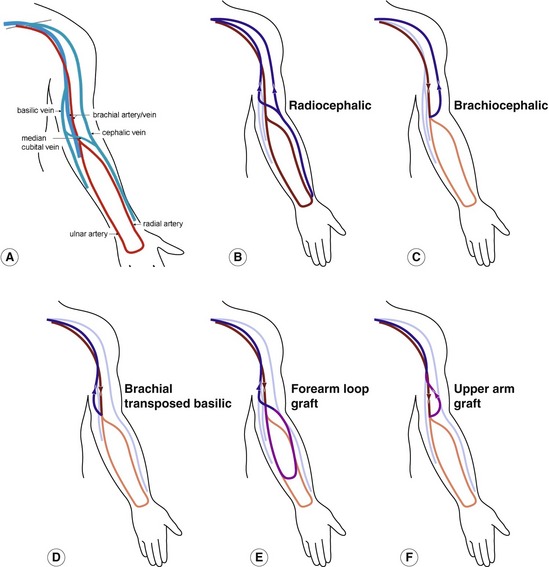
The main sites for fistulas and grafts are listed in Box 16.1 and shown diagrammatically in Figure 16.2. The nondominant arm is generally used initially. Box 16.1 shows an approximate order of preference; the choice for an individual patient depends on many factors. For example, a young patient with good peripheral arm vessels may be a better candidate for a radiocephalic fistula whereas an elderly patient with diabetes and known peripheral vascular disease might start dialysis with a more proximal access. A major advantage of a peripheral fistula is that it may leave more proximal vessels available for future access.
BOX 16.1 Main sites for arteriovenous fistulas and grafts in approximate order of preference
• Radial–cephalic fistula (ulnar basilic is possible in some patients)
• Brachial–cubital or brachial–cephalic fistula
• Brachial artery–transposed basilic vein fistula
• Forearm graft from radial artery–cubital fossa vein or looped graft from brachial artery–cubital fossa vein
• Upper-arm graft brachial artery–axillary vein
Temporary access – role of ultrasound
Ultrasound is useful to assess central veins to ensure patency for emergency central dialysis catheter placement in patients with acute renal failure or failed permanent access. The patient should be lying flat so that the central veins are not collapsed. The internal and external jugular veins are examined using a low-frequency (4–8 MHz) linear array in B-mode and with color and pulsed Doppler to ensure patency and normal venous flow patterns. The subclavian veins may be imaged in long section either supraclavicularly or infraclavicularly (Fig. 16.3). The subclavian vein often collapses during the cardiac cycle or in response to breathing. The right and left proximal internal jugular vein and subclavian veins may be difficult to image with a linear array due to clavicle, sternum, and ribs which restrict ultrasound access. A small footprint phased or tightly curved array (Fig. 16.4) aids in color flow imaging of these veins (Fig. 16.5) and the brachiocephalic veins, although B-mode images are poor and compression of all these veins, to rule out deep-vein thrombosis, is impossible.
PERMANENT ACCESS
Preassessment
Technique for assessing arm veins and arteries
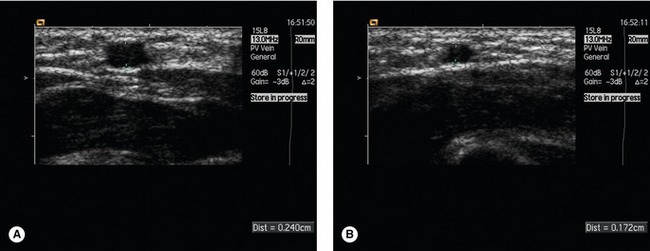
The arm to be imaged is supported comfortably with the palm of the hand uppermost (Fig. 16.6). For the superficial veins, a high-frequency (for example, 8–14 MHz) linear array is used. A tourniquet is applied proximal to the measurement sites to occlude venous return and the veins are allowed to expand (Fig. 16.7).
It is important to use very light pressure; even with a tourniquet, veins are readily compressed and the diameter may be underestimated. The veins are measured in transverse section and are scanned through their length to check for patency, narrowing, particularly near confluences/bifurcations, anatomical variations (for example, large veins communicating with the deep veins), and continuity of flow. The proximal cephalic vein may be compressed extrinsically by surrounding tissue just before its insertion to the subclavian vein. This is sometimes relieved by relaxation of the arm.
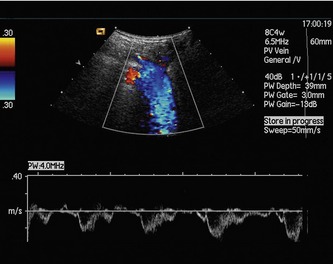
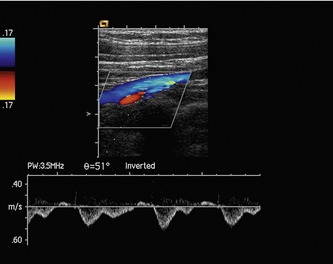
The deep veins are imaged to ensure patency for the outflow of the fistula. For the proximal arm veins, axillary and subclavian veins, a lower-frequency transducer may be required. Color filling of the deep veins is helpful where compression is impossible (Fig. 16.5). Flow waveforms in the proximal veins should show phasicity with respiration (Fig. 16.8). Lack of or reduced phasicity is an indication of possible proximal occlusion or stenosis; compare the waveforms with those on the contralateral side. A phased or curvilinear array may be helpful to determine central vein patency.
The arteries should be examined for normal pulsatile flow to wrist level. Radial artery internal diameter should be measured and note is taken of arterial disease, including general calcification in the arm arteries. Even moderate stenoses should be noted as they can become more hemodynamically significant with the larger flow volumes after fistula creation. It is important to identify the brachial bifurcation level if surgery in the cubital fossa is contemplated. For patients with evidence of arterial disease, measurement of right and left brachial artery blood pressure may reveal proximal disease.
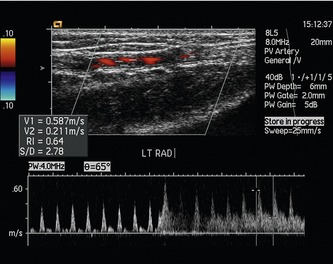
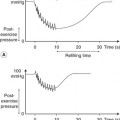
For radiocephalic fistulas, it has been suggested that measurement of flow waveform changes in an induced hyperemic response in the radial artery prior to surgery is a good measure of the likelihood of success of the fistula. A low resistance index (< 0.7) in the initial period of hyperemia was associated with a markedly improved outcome when compared with fistulas formed from arteries with an index ≥ 0.7 (Malovrh 2002) (Fig. 16.9), although others have been unable to show the same discrimination between fistula success and failure (Lockhart et al. 2004).
A checklist of observations and measurements made is given in Box 16.2.