Introduction
Muscle is probably one of the most difficult tissues in the musculoskeletal system to assess with ultrasound. There are a variety of reasons for this, including the complex anatomy of the structures involved, the isotopic nature of muscle, the different functional bundles present within muscles and compartments, and the varied site and appearance of muscle lesions.
Once the examining sonographer appreciates the level of difficulty involved, muscle ultrasound becomes a more viable clinical tool. Increasing levels of exercise in the general population and an emphasis on imaging of sports-related injuries in athletes has resulted in an increase in requests for muscle ultrasound. Developments in ultrasound technology have also resulted in the development of more mobile ultrasound services with many professional clubs now employing diagnostic ultrasound as part of their regular medical services.
Technique
An ultrasound scan is part of a clinical assessment and therefore each examination should begin with a brief history and sometimes even a physical examination of the patient.
| The presence of bruising is important; the site of muscle damage frequently lies immediately proximal to the site of subcutaneous ecchymosis. |
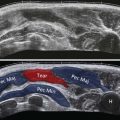
The sonologist should use the highest-frequency probe to give sufficient depth of penetration to allow assessment of the entire muscle under interrogation. In general high-frequency linear array probes (for example, 7–13 MHz and 5–17 MHz) can be used to assess muscle injury even in large compartments such as the thigh or hamstring. This is achieved by a combination of lowering the frequency of the probe to give sufficient penetration and by using electronic curvilinear field of view to give greater tissue coverage. Extended field of view scanning is useful in muscle ultrasound as it gives the examiner an appreciation of the overall muscle architecture and the degree of damage present. This is different to the use of extended field of view scanning in other areas where frequently it is only of value in demonstrating abnormalities for clinicians; in muscle ultrasound it helps with the grading and identification of muscle tears.
The focus of this chapter is limited to ultrasound imaging of muscle injury. Inflammatory conditions of muscles are, in the opinion of the author, best assessed with MRI and have not been considered in this chapter.
Muscle Anatomy
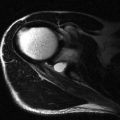
Muscle has a hierarchical internal structure with hypoechoic myofibrils separated by thin internal septa. This structure produces the typical ultrasound appearances of muscle tissue with hypoechoic tissue separated by thin hyperechoic parallel lines. This parallel orientation of the myofibrils renders muscle anisotropic, resulting in differing ultrasound properties dependent on the incident angle of the ultrasound beam. In transverse this produces the classic starry sky appearance with bright septa seen as dots within the hypoechoic dark surrounding myofibrils ( Fig. 33.1 ). The echogenicity of the surrounding myofibrils varies with probe angle, either accentuating or decreasing this appearance. When examined in the longitudinal plane, muscle anisotropy is easier to appreciate by angling the probe or beam steering ( Fig. 33.2 ). Within any single muscle there are usually separate functional bundles, especially in large muscles crossing two joints more prone to injury. This results in fibres tracking in different directions within muscles themselves, complicating even further the ultrasound assessment of muscle.


An understanding of myotendinous junction (MTJ) anatomy is vital to successful imaging of muscles ( Fig. 33.3 ).
In young skeletally mature athletes, the MTJ represents the weak point in the kinetic chain most prone to injury.

The anatomy of the MTJ can be complicated and requires detailed assessment. Muscles with multiple heads usually have more complex MTJ anatomy and are unfortunately the most commonly injured muscles requiring imaging.
| The junction between a muscle and a tendon can be either epimysial (at the periphery of the muscle) or via a central aponeurosis with a gradual thickening of the aponeurosis/epimyseum as the rounded tendon forms. |
Anatomy of Commonly Injured Muscles
Quadriceps Anatomy
The quadriceps muscle comprises four components, vastus lateralis, vastus medialis, vastus intermedius and rectus femoris. This muscle is responsible for knee extension and is commonly injured during kicking. The vastus intermedius contains a high proportion of slow twitch fibres and, as it originates on the anterior femoral shaft, it only crosses one joint. As such it is rarely injured in exercise-related sprinting injury, though is prone to contusion, mainly as a result of its close proximity to the femoral shaft. Vastus medialis and lateralis also only cross one joint.
The vastus lateralis is the largest part of the quadriceps femoris. It arises by a broad aponeurosis, which is attached to the upper part of the intertrochanteric line and the upper half of the lateral lip of the linea aspera. The distal tendon forms from an aponeurosis on the deep surface of the lower part of the muscle: this aponeurosis forms part of the quadriceps tendon and inserts on the superolateral border of the patella.
The vastus medialis arises from the lower half of the intertrochanteric line, the medial lip of the linea aspera and the tendons of the adductor group. Its fibres attach to an aponeurosis that lies on the deep surface of the muscle and forms part of the quadriceps tendon. The most inferior portion of vastus medialis lies directly adjacent to the femoral shaft and as such is prone to contusion. This inferior portion has a more horizontal fibre orientation and inserts onto the medial retinaculum of the patella. This portion of the muscle is sometimes referred to as vastus medialis obliquus and is prone to injury during patellar dislocation and contusion.
Rectus femoris arises from the two proximal tendons: the direct (or sometimes called the straight) head and the indirect (reflected) head. These merge 2 to 3 cm below their origins to form the conjoint tendon. The direct head arises from the anterior inferior iliac spine with the indirect head arising from the iliac bone just posterior and inferior to the direct head origin. The direct head forms the anterior portion of the tendon and forms an anterior epimysial MTJ terminating in the proximal thigh. The indirect head forms the posterior portion of the conjoint tendon terminating in a central aponeurosis within the muscle, which extends a long way down the muscle. This central septum terminates approximately 10 cm above the superior pole of the patella and overlaps the distal rectus femoris MTJ. As a result it is possible and indeed not unusual to have a proximal MTJ injury in the distal thigh.
| Rectus femoris crosses two joints and contains a high proportion of fast twitch fibres, which is why it is the most commonly injury of the knee extensors during kicking injuries. |
Hamstring Anatomy
| The hamstrings consist of three muscles, all of which cross two joints with high proportions of fast twitch fibres. Like rectus femoris, this combination makes them extremely prone to exercise-related injury. These muscles all arise from the ischial tuberosity. |
The biceps femoris has two heads and is the most commonly injured hamstring muscle.
The semitendinosus and biceps femoris arise from a conjoint tendon from the posterior and more medial aspect of the ischial tuberosity. This tendon separates into its separate components 7–10 cm below its origin. The semitendinosus muscle belly arises from an epimysial proximal MTJ which lies on the posterolateral aspect of the muscle anterior to the sciatic nerve. Distally the semitendinosus forms a long tendon (hence the name semitendinosus) that, in the distal thigh, sits on top of the semimembranosus muscle belly looking a bit like a cherry on a bun!